Introduction
The study of sleep quality has gained interest in the scientific community due to its high impact on mood, memory, intellect, prevention of chronic disease, and the general lifestyle and well-being of individuals.1,2 In this sense, assessing sleep quality among medical students is critical because they are vulnerable to sleep and mental health disorders.3 Moreover, because of their constant exposure to the demands of their professional training, academic stress is also present in this university population, which may be associated with poor quality sleep.4
In a study conducted in Spain with 118 students from the Faculty of Medicine of the Universidad de Lleida, Oro et al.5 confirmed the presence of stress in medical students, as they found that 16.95% of participants had high levels of stress, a high percentage compared to the figures of other people their age in general. On the other hand, in a research carried out in Colombia with 217 medical students from the Universidad Tecnológica de Pereira, Machado-Duque et al.6 found that 79.3% of participants were poor sleepers. In turn, in a study of 326 medical students at King Abdulaziz University in Saudi Arabia, Safhi et al.7 found that stress and poor sleep quality were significantly associated (p<0.001).
The health crisis caused by COVID-19 has resulted in remote hospital internships and classes, forcing medical students to rapidly develop adaptive capacities and modify their professional development projects, which, when combined with stress and other problems unrelated to the pandemic, has had a psychological impact on this population.8-10
Furthermore, it has been proposed that a number of factors are associated with poor sleep quality in medical students, including sex;11-13 academic stage;11-13 screen time;11 dietary habits;11 caffeine, cigarette, and alcohol consumption;12 levels of physical activity;11 place of origin;13 and housing situation.11,13
To date, information on the variables "academic stress" and "sleep quality" during the COVID-19 pandemic is scarce in Latin America, so this study can serve as a basis for future research and for universities to take measures based on its results to ensure the well-being of their students.
Therefore, the purpose of this study was to evaluate the association between academic stress and sleep quality among medical students at a university in Lima, Peru, during the COVID-19 pandemic.
Materials and methods
Study type and population
Analytical cross-sectional study. Sample size was calculated using the statistical formula for analytical cross-sectional studies. For this purpose, a frequency of study event with an exposure factor of 77% (academic stress and poor sleep quality), a frequency of study event without exposure factor of 88%, a statistical power of 80%, and a confidence level of 95% were considered. Thus, a sample size of 410 first- to sixth-year students enrolled in the Faculty of Human Medicine of the Universidad Ricardo Palma during the second academic semester of 2020 was obtained. The sampling method was stratified random sampling, depending on the year of university career, in order to have a proportional representation of each year. Students who did not agree to participate or did not sign the informed consent form and those who provided incomplete responses were excluded from the study.
Variables and instruments
The primary variable academic stress was measured using the SISCO SV-21 Academic Stress Inventory adapted by Alania et al.14 to the context of the crisis by COVID-19; this instrument is composed of 48 items and had a Cronbach's alpha >0.88. The following scale was established for the assessment of stress levels:15
Mild level of academic stress: 0-33%.
Moderate level of academic stress: 34-66%.
Excessive level of academic stress: 67-100%.
The measurement of the main variable sleep quality was made using the Pittsburgh Sleep Quality Index (PSQI) adapted to Spanish by Royuela & Macias,16 who reported a Cronbach's alpha of 0.81 in their study. This instrument, which can be self-administered, has 19 items grouped into 7 components that provide a score for each component, obtaining an overall score ranging from 0 to 21 points, where a score >5 is considered as "poor sleep quality". In Peru, Rosales et al.17 confirmed the reliability of this instrument in their study.
In addition, sociodemographic variables and student habits that could be related to sleep quality were included; the intervening variables were: biological sex, age in years, year of university, place of birth, living with relatives, dependence on parents, childbearing, working in addition to studying, use of electronic devices one hour before bedtime, consumption of harmful substances (coffee, alcohol, energy drinks, and cigarettes), and level of physical activity, which were recorded using a data collection form.
Procedures
The procedures carried out in the study were approved by the Research Institute of Biomedical Sciences (INICIB) of the Universidad Ricardo Palma.18 The surveys were administered during the fourth week of October and the first two weeks of November 2020 using the Google Forms platform. Participation was voluntary and consented. Data were then tabulated using Microsoft Excel 2016.
Statistical analysis
Quantitative variables such as age in years and year of university were described using measures of central tendency and dispersion, and categorical variables were described using frequencies and percentages. The distribution of the responses to each question of the questionnaires was presented through frequencies and percentages. Bivariate and multivariate analyzes were performed using prevalence ratios (PR) with a 95% confidence interval to identify factors associated with poor sleep quality. Additionally, factors associated with academic stress were evaluated. Data were processed with IBM SPSS 25 and STATA 15, and a significance value of p< 0.05 was established for all statistical analyzes.
The following variables were dichotomized to carry out the statistical analysis: the year of university was divided into preclinical (from the first to the third year) and clinical (from the fourth to the sixth year); place of birth into Lima (people from the province of Lima) and not Lima (people from other provinces of Peru); use of electronic devices into one hour before bedtime (individuals who used electronic devices with a frequency per week of: every day, 3-5 times and 1-2 times) and no use (individuals who did not use them); physical activity into not adequate (frequency <5 times per week: never, rarely, rarely, and sometimes) and adequate (frequency >5 times per week: always and almost always); and academic stress into high levels (severe and moderate level of academic stress) and low levels (mild level of academic stress and no academic stress). The dichotomization of the latter variable was based on the findings by Almojali et al.19 and Alotaibi et al.20
Ethical considerations
The study took into account the ethical principles for research involving human subjects established by the Declaration of Helsinki,21 while maintaining the privacy and confidentiality of the data. Likewise, participants gave their informed consent to conduct the study, which was approved by the Research Ethics Committee of the Faculty of Human Medicine of the Universidad Ricardo Palma with the committee code PG-081-2020 of December 2, 2020.
Results
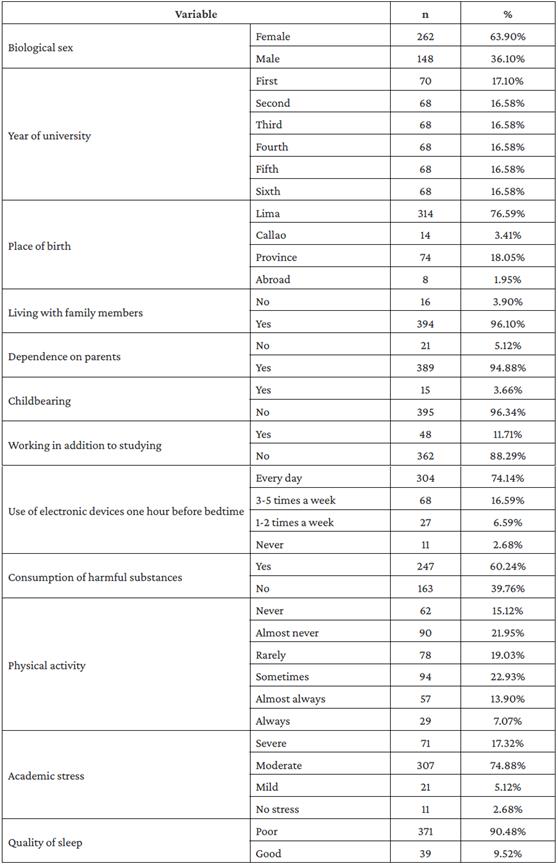
The mean age of the participants was 21.77 years (SD: ±4), the majority were women (63.90%), and the most frequent place of birth was Lima (76.59%). 97.32% of the students had academic stress in various categories, and 90.48% had poor sleep quality. The general characteristics of the sample are described in Table 1.
Table 2 shows the bivariate analysis of the factors associated with poor sleep quality. It is evident that there was a significant association with female biological sex (p=0.006), not living with relatives (p=0.000), and high levels of academic stress (p=0.000). Multivariate analysis revealed that the factors significantly associated with poor sleep quality were high levels of academic stress (aPR: 2.433; 95%CI: 1.619-3.657; p=0.000), not living with relatives (aPR: 1.264; 95%CI: 1.107-1.443; p=0.001), and working in addition to studying (aPR: 1.106; 95%CI: 1.012-1.209; p=0.026).
Table 2 Bivariate and multivariate analysis of factors associated with poor sleep quality.
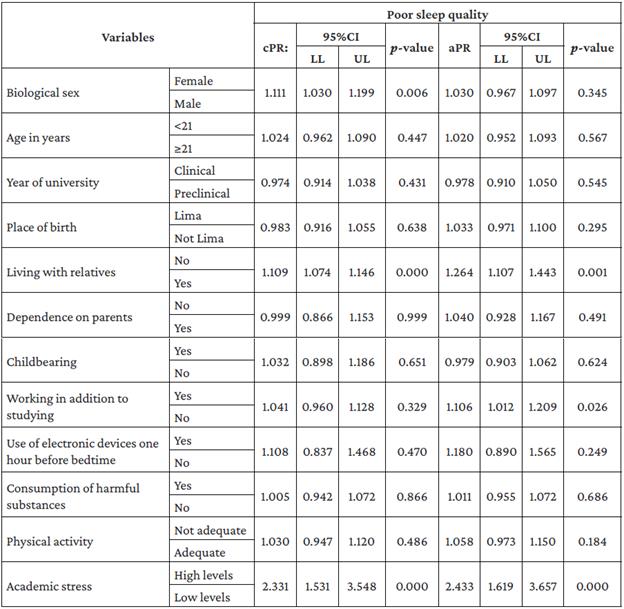
cPR: crude prevalence ratio; aPR: adjusted prevalence ratio; 95%CI; 95% confidence interval; LL: lower limit; UL: upper limit.
Source: Own elaboration.
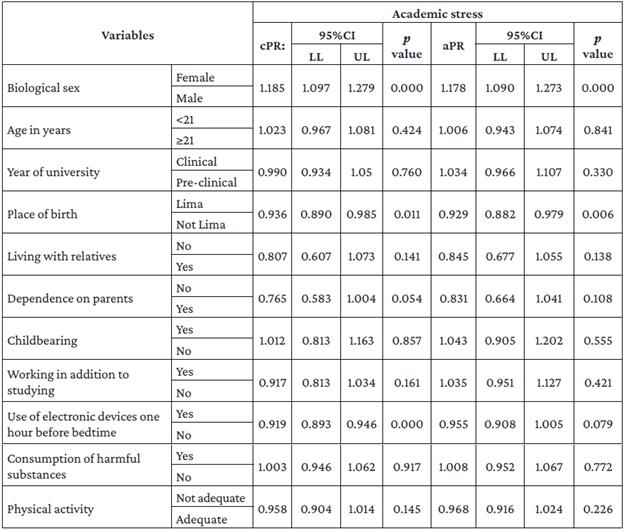
Furthermore, Table 3 shows that the variables associated with academic stress through bivariate analysis were female biological sex (p=0.000), place of birth Lima (p=0.011), and use of electronic devices one hour before bedtime (p=0.000), while the associated variables in the multivariate analysis were female biological sex (aPR: 1.178; 95%CI: 1.090-1.273; p=0.000) and place of birth Lima (aPR: 0.929; 95%CI: 0.882-0.979; p=0.006).
Discussion
The present study documented a significant association between academic stress and sleep quality (p=0.000), which is consistent with what has been observed in other studies.19,20,22-26 This demonstrates the importance of addressing these variables in the university population, as good sleep quality is not only a determining factor for health, but also an essential element for achieving a good quality of life and good daytime functioning, making it possible to have an adequate level of attention to perform different tasks.27 In this sense, studying sleep quality and associated factors in future physicians is relevant since they will take care of the health of the population in the immediate future.
It was found in the present study that 97.32% of the sample had academic stress and 90.48% had poor sleep quality, figures higher than those reported by Almojalí et al.19 in 2016 after conducting a research on 263 first- to fourth-year medical students from Saudi Arabia, which were 53.23% for prevalence of stress and 76.04% for poor sleep quality. These differences may be explained by the instruments used to measure the two main variables (Kessler's psychological distress index and the PSQI English version), as well as the socio-environmental contexts of each study, since the research by Almojalí et al.19 was conducted prior to the COVID-19 pandemic, unlike the present study, which was carried out in 2020 at the time when COVID-19 most impacted the world's population.
Habits and lifestyle play a fundamental role in the processes of health and disease. Of the students included in the present study, 79.03% did not perform sufficient physical activity, that is, 30 minutes 5-7 times a week according to the recommendations of the World Health Organization,28 which may have influenced the results, since there is evidence that physical activity has a positive and protective impact on mental health.29 In this regard, Chang et al.,30 in a study of 1 230 Taiwanese university students, found that students who had a better perception of their health or satisfaction with their exercise engagement also had a better quality of sleep and a better quality of life.
On the other hand, 60.24% of the participants analyzed here consumed harmful substances (coffee, energy drinks, alcohol, and cigarettes), which, according to Sawah et al.,31 is a common practice among medical students and can affect sleep quality and cause health problems.
It was also noted in the present study that 74.14% of participants used electronic devices every day one hour before bedtime and, if those who did this 3-5 times a week are included, this percentage rises to 90.73%. The recommendations of the Sociedad Española de Sueño (Spanish Sleep Society) for good sleep quality suggest avoiding the use of electronic devices with light emission at least two hours before the usual sleep schedule, as this slows the activity of the suprachiasmatic nucleus and delays the secretion of melatonin, postponing the onset of sleep and reducing wakefulness in the morning.32
With regard to the latter aspect, it is important to keep in mind that although studies, such as Vivanco-Vidal et al.,33 have established that the COVID-19 pandemic has resulted in restrictive confinement, suspension of face-to-face activities, social isolation and greater emphasis on online education, and that this has contributed to increased levels of stress, pressure and anxiety in the young population, the present study did not specifically address the variables of the online educational model or the social factors of the pandemic, namely, social restriction and remote classes, which involve multiple hours in front of the computer.
The female biological sex variable reached significance only in the bivariate analysis. This is in agreement with the findings of Vilchez-Cornejo et al.,34 who conducted a study in 1 040 medical students from 8 medical schools in Peru and found that being a female increases the probability of being a poor sleeper by 13% (PR: 1.13; 95%CI: 1.05-1.21), and by De La Portilla-Maya et al.,35 who studied 259 medical students at the Universidad de Manizales (Colombia) and found that male students tend to have lower sleep quality problems than women (p=0.0218). In this sense, social and cultural patterns, as proposed by Becker et al.36 and Surani et al.37 may be related to this result in females.
Multivariate analysis identified three independent factors associated with poor sleep quality: high levels of academic stress, not living with relatives, and working in addition to studying.
The significant association between high levels of academic stress and poor sleep quality (aPR:2.433; p=0.000) was similar to that reported in research conducted before the COVID-19 pandemic, such as Waqas et al.,23 who studied 263 medical students from Pakistan in 2014 and found a significant association between stress level and sleep quality (OR: 1.99; p<0.05), and Herawati & Gayatri,24 who in 2019 studied 450 undergraduates from 3 university communities (science and technology, social humanities, and health) in Indonesia and found a significant association between sleep quality and stress level (OR: 4.7; p=0.001). This association may be related to the fact that stress is accompanied by a decline in slow waves and rapid eye movement, and that sleep deprivation as a stressor has a significant impact on sleep architecture and circadian rhythms.19
It is striking that the association found in the present study between not living with relatives and poor sleep quality (aPR: 1.264; p=0.001) was not reported in studies carried out before the pandemic with medical students. However, it should be mentioned that in the theses published by Bautista-Gonzáles22 and Llanos38 it was identified that the variables type of family (p=0.857) and living alone (OR: 1.91; p=0.074), respectively, were not significantly associated with sleep quality.
At this point, it is important to mention that during the COVID-19 pandemic, family played an important role as a source of emotional, social, economic and security support when dealing with the adverse events caused by the health crisis.39-41 In this regard, for example, Cao et al.,42 in a study with 7 143 medical students during the COVID-19 pandemic boom in China, using the 7-item Generalized Anxiety Disorder scale, found that living with parents was a protective factor against anxiety (OR: 0.752; p=0.017).
In the present study, the variable working in addition to studying was also associated with poor sleep quality (aPR: 1.106; p=0.026), which is consistent with the findings of Ojeda-Meza & Padilla-Romero,43 who carried out a study in 2018 in 226 students enrolled between the eighth and the tenth semester of the Faculties of Human Medicine, Obstetrics and Child Care, Dentistry, and Nursing of the Universidad Católica de Santa María applying the PSQI instrument to obtain the values of sleep quality and found a significant association between work activity and sleep quality (p=0.046). The above seems to indicate that work is an important factor that can affect the quality of sleep and could be explained because this activity has its own demands that add to academic duties, thus causing an increase in the concern experienced by students that could be associated with poor sleep and daytime sleepiness. This coincides with the findings by Becerra-Rodríguez44 in the literature review conducted for the elaboration of his thesis, in which he aimed to analyze the relationship between sleep quality and academic stress and well-being in 224 students from 7 faculties of humanities and arts programs and 3 faculties of science programs of a private university in Lima.
Carrillo-Regalado & Ríos-Almodóvar,45 in a study carried out in 1 830 students with 4 or more semesters of studies enrolled in all the undergraduate courses of the thematic university centers of the Universidad de Guadalajara, established that two thirds of the university students who work experience a reduction in the time available for school and personal activities, which negatively affects their academic performance. Likewise, as evidenced by Ramirez-Ortiz et al.,46 the COVID-19 pandemic has resulted in work and study tasks being transferred to the home, and although these activities can be sustained, they are far from optimal performance, negatively affecting productivity and efficiency due to the increased interaction of home life with work and study tasks.
Moreover, Wathelet et al.47 also found a statistically significant association between stress and female sex (OR: 2.37, p<0.001). In this regard, it should be considered that, as stated by García-Araiza et al.48 in a study in which they surveyed 71 medical students to identify their stress levels, their reactions to stress and the strategies used to manage it, women, unlike men, have hormonal changes that make them susceptible to perceiving higher levels of stress. Furthermore, according to the findings of Lemos et al.49 in their study conducted with 217 medical students at a university in Medellín (Colombia) to characterize the levels of stress, mental health and its association with psychological, physiological and educational variables in Colombian medical students, the greater risk of stress in women is associated with social stigma and unequal opportunities in academic and professional training.
The variable place of birth Lima was a protective factor for the development of academic stress, but this finding cannot be compared because other similar studies have not reported this variable. However, in the study by Damián-Carmin,50 carried out with the aim of studying the relationship between academic stress and health behaviors in a group of 130 students in their first years of study at a private university in Lima, it was evident that students from the province had behavioral reactions more often (p=0.01), were prone to a higher degree of despair, anguish and anxiety (p=0.04), conflicts (p=0.01), and isolation (p=0.02). Similarly, Boullosa,51 in a research conducted with 198 first- and second-year students at a private university in Lima to describe and relate the levels of academic stress and coping, found that the students from the provinces had a higher proportion of psychological symptoms (p=0.03), trouble sleeping (p=0.03), prolonged fatigue (p=0.01), restlessness and inability to relax (p=0.05). The latter findings, prior to the pandemic, may be attributable to the fact that university students who had to migrate to Lima, the capital of Peru, must live new situations that require adaptation at the academic, cultural and social levels, which may even generate a state of acculturation that affects their well-being.50
The present study reports several important and significant findings; however, there are still some limitations inherent to its design, such as the fact that data collection was done at a single point in time, so it is not possible to establish a cause-effect relationship between the variables. In addition, the study sample only represents the medical school of a private university in Peru. Accordingly, it is suggested to include in future studies the evaluation of the learning modality of virtual classrooms and university education strategies during the pandemic.