Introduction
At present, HIV/AIDS infection continues to be one of the most serious public health problems in the world 1. New health policies around the world have led to greater access to antiretroviral therapy (ART) 2, allowing seropositive individuals to live longer and in better health 1,2.
At the global level, after confirming therapeutic failure (due to viremia or a detectable viral load in plasma or to toxicity), the presence of resistant viruses as the cause of this failure should be determined. This can be confirmed via HIV resistance genotyping to identify resistance mutations in the virus that may affect the antiretrovirals (ARVs) present in the therapeutic regimen. Only after identification can a patient's ART be customized and the best rescue therapy be chosen. Since 2014 in Colombia, the current guide recommends resistance studies after the first therapeutic failure 3.
The recommendations for the use of different ARV regimens have been updated based on efficacy, tolerability, lesser incidence of undesirable effects and ease of administration. The first-line regimens indicated today in Colombia include two nucleoside reverse transcriptase inhibitors (NRTIs) + one non-nucleoside reverse transcriptase inhibitor (NNRTI) or one integrase inhibitor or one potent protease inhibitor 3.
There is little evidence regarding HIV resistance to ARVs in Colombia 4-6, with a greater impact reported for NNRTIs and NRTIs. Documenting the frequency, type and repercussions of the resistances that affect different ARV drug families continues to be necessary to define strategies to guide the selection of ARV regimens for therapeutic rescue in patients with HIV in our setting.
The present study describes the sociodemographic and clinical characteristics of and the pattern and frequency of HIV resistance mutations to ARVs in HIV(+) patients with failed ART between 2002 and 2015 and who were treated by the specialized comprehensive care program of the Fight Against AIDS Corporation (Corporación de Lucha Contra el SIDA - CLS) in Cali, Colombia.
Materials and Methods
Design and sample
This was a cross-sectional descriptive study in a population of 403 HIV(+) patients over 18 years of age and of both sexes after ART failure, with a viral load >1000 copies of RNA-HIV-1/ml plasma and an available resistance genotyping profile between 2002 and 2015. All patients were under specialized care at CLS in Cali, Colombia, and previously signed an informed consent form for the use of their epidemiological, clinical and virological data.
Viral load quantification was performed with plasma isolated from blood samples obtained by venipuncture at a sampling point of CLS by trained personnel from the Colombian Red Cross - Cali, Valle District. Plasma samples were stored and preserved following biosecurity and cold chain protocols until use. HIV resistance genotyping, based on PCR and subsequent sequencing of the products amplified in the protease (PR) and retrotranscriptase (RT) viral regions, was performed using a TRUGENE® HIV-1 genotyping kit 7 at the Molecular Analysis Center (Centro de Análisis Molecular - CAM) in Bogotá. Mutations that confer resistance to different ARV drugs and drug families according to the list of the International AIDS Society USA 2015 (IAS-USA 2015)8 were considered. The period of time when the genotype tests were performed (2002-2006 vs. 2007-2015), the time of genotyping respective to therapeutic failure (early, < 6 months vs. late, ≥ 6 months) and the presence of relevant mutations according to the IAS-USA 2015 list were compared. Only mutations with a penalty score ≥ 15 for any drug according to the Stanford HIV Drug Resistance Database (HIVdb) (https://hivdb.stanford.edu/hivdb/by-mutations/) were studied.
Data collection was carried out by a group of research assistants trained and supervised by an internist specialized in HIV/AIDS. Data were collected using an individualized structured form on which sociodemographic data, habits, history of HIV/AIDS diagnosis, infection monitoring, and establishment of ART were recorded for each patient.
Statistical analysis
The data were input and analyzed in STATA version 12. For description and analysis, the sample was first divided according to the period when genotyping was performed, according to the recommendation for the use of genotyping for the first time in Colombia contained in the practical guide for HIV care adopted by the Ministry of Health of Colombia in 20069. For this purpose, the sample was divided into a group of patients with genotyping performed prior to the implementation of this recommendation for the first time in the Colombian guide9, namely, in the period of 2002 to 2006 (n1 = 98), and a second group of patients with genotyping performed between 2007 and 2015 (n2 = 305). Likewise, two groups were defined according to the time of genotyping, one containing patients with the first virologic failure documented, with "early" resistance genotyping, i.e., performed in the first six months after failure (n1 = 272), and another composed of patients with one or more documented virologic failures, with "late" resistance genotyping, i.e., performed six months after documenting the first virologic failure (n2 = 131). Descriptive statistics were used to determine the distribution of sociodemographic variables. The Shapiro-Wilk test was used to determine the normality of the distribution of quantitative variables. Groups were compared by period of identification of therapeutic failure and by time of resistance genotyping using tests for independent samples, including Student's t-test, the Mann-Whitney U-test and the chi2 test, according to the scale of measurement of variables. A significance level of 0.05 was adopted for all statistical tests.
Ethical aspects
Participation in the study was completely voluntary, and written consent was obtained from each participant for the use of the information recorded in the medical records. This study was reviewed, approved and supervised by the institutional ethics committee for research in humans of CLS (IRB number: IRB0000573232).
Results
Description of the study population (2002-2015)
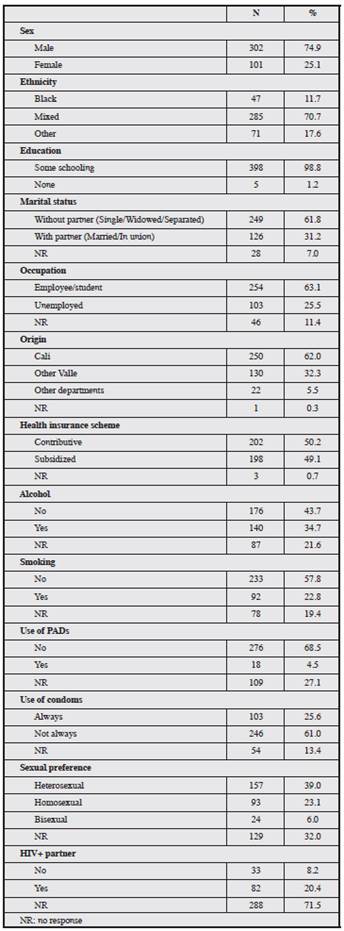
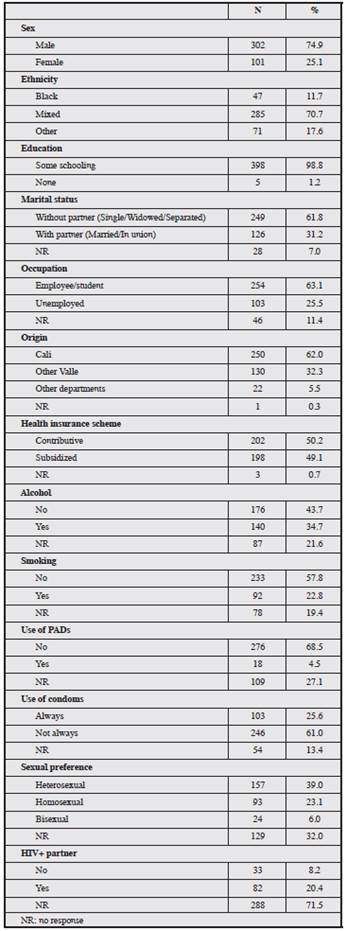
Table 1 shows the main sociodemographic characteristics of the 403 patients studied. The mean age at the time of genotyping was 38.7 ± 10 years, with a predominance of male (74.9%), mixed-ethnicity (70.7%) patients mainly from Cali (62%). A total of 61.7% did not live with a partner, more than half of the sample had some type of occupation, and those with health insurance predominated. Regarding habits, one-third drank alcohol, one in five consumed tobacco, and 4.5% used psychoactive drugs (PAD).
Only 25.6% reported always using a condom, 29% of the population were men who had sex with men (MSM) or bisexuals, and one-third did not respond with respect to their sexual preference. A total of 20.4% had a partner with HIV.
Analysis according to identification of failure and precocity in the study of resistance after therapeutic failure
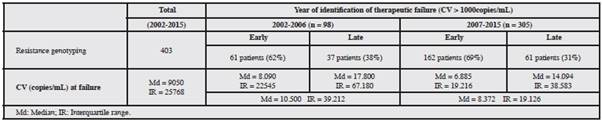
For this analysis, the 403 patients were divided into subgroups according to the period when therapeutic failure was detected, i.e., 2002-2006 (n = 98) vs. 2007-2015 (n = 305), as well as the time of resistance genotyping (early or late). The number of patients in each group is shown in Table 2.
ART (5) prior to and at the time of virologic failure
Table 3 shows the most frequent ARV drug regimens the patients were receiving when virologic failure was documented, by period and time of genotyping. Notably, the data for the different ARV regimens used at the time of virologic failure do not correspond to the full sample due to the lack of data in the medical records (patients with no information on regimens at the time of virologic failure = 5.7%). The most frequently used ARV regimen in patients with therapeutic failure was AZT/3TC+EFV, and its use was significantly higher in the 2007-2015 period and in the early genotyping group (Table 3). The regimens that included AZT/3TC plus efavirenz (EFV) or nevirapine (NVP) were the most frequently used in the early genotyping group, and protease inhibitors (PIs) were the most frequently used in the late genotyping group (Table 3).
The ARVs that the patients received before genotyping (Table 4) were also analyzed. The use of stavudine (D4T), didanosine (DDI), indinavir (IDV) and nelfinavir (NFV) was significantly more frequent during the 2002-2006 period, and the use of EFV and ritonavir-boosted lopinavir (LPV/r) was more frequent during the 2007-2015 period. Patients in the late genotyping group received AZT, D4T, DDI and all PIs significantly more frequently.
Table 4 Drugs in use prior to virologic failure according to time and period of resistance genotyping.
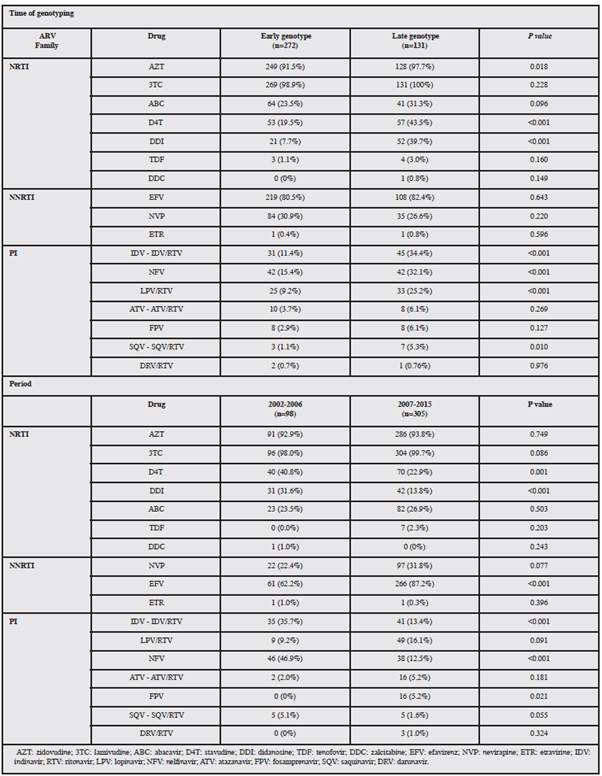
Regarding the NNRTI family, there was marked use of EFV and NVP, with no differences by genotyping time. However, exposure to EFV was higher for the study cohort during the 2007-2015 period (Table 4). For the PI family, the use of pioneering drugs such as NFV and IDV stands out, having greater representation in the 2002-2006 cohort and in the late genotyping group. The use of new PIs such as darunavir (DRV) was absent in the first period and very scarce during the 2007-2015 period (Table 4).
When comparing periods, exposure to ARV regimens with the three families of drugs at the time of failure was significantly greater during the first period (Figure 1A) and in the late genotyping group (Figure 1B). Thus, 46.4% of the patients with failure detected in the first period were PI-, NRTI- and NNRTI-experienced compared to 34.1% of individuals in the 2007-2015 period, the latter presenting a significantly greater use of regimens with NRTIs+NNRTIs (61.0%) than in the previous period (Figure 1A). In addition, the use of NRTIs+NNRTIs was significantly greater in patients in the early genotyping group (Figure 1B).
Identified drug-resistance mutations (DRMs)
The most frequent RT DRMs were M184V (for NRTIs) and K103N (for NNRTIs) in both genotyping periods and times (Figures 2). However, K103N was significantly more common (p = 0.032) in the early genotyping group during the 2007-2015 period (Figure 2A) than in the late genotyping group (p = 0.332) during the 2002-2006 period (Figure 2B).
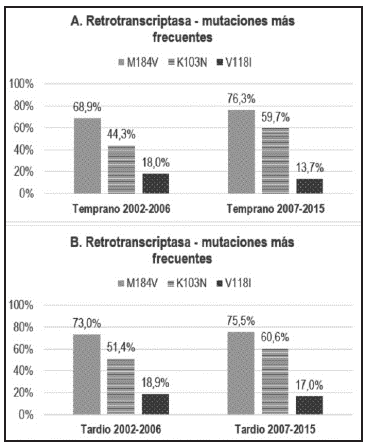
Figure 2 A. Most frequent mutations found for retrotranscriptase, according to period and early genotyping time. B. Most frequent mutations found for retrotranscriptase, according to period and late genotyping time.
The analysis also revealed the presence of other RT DRMs at the time of early genotyping when comparing both periods: mutations Y181C (p = 0.047) and G190A (p = 0.020) for NNRTIs were more frequent during the 20072015 period (Figures 3A and 3B). These mutations confer a high level of resistance to the family of NNRTIs used in Colombia (NVP and EFV) and to new second-generation NNRTIs such as etravirine (ETR) and rilpivirine (RPV) (Figure 3B).
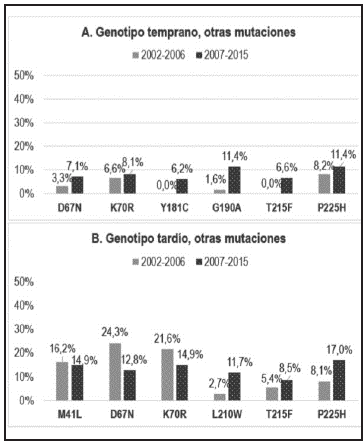
Figure 3 Other mutations found for retrotranscriptase, according to period and early genotyping time. B Other mutations found for retrotranscriptase, according to period and late genotyping time.
The frequencies of other DRMs found in the late genotyping group did not differ significantly between the two periods. However, there was a higher frequency of thymidine analog mutations (TAMs) (D67N, K70R), mainly in the late genotyping group during the 2002-2006 period (Figure 3B). These mutations are generally selected by exposure to AZT or D4T and are associated with cross-resistance to all NRTIs when two or more mutations are present.
With respect to the PI DRMs, there was a higher frequency of occurrence of PI DRMs during the 2002-2006 period (Figures 4A and 4B) for the D30N mutation (p = 0.002), associated with NFV failure.
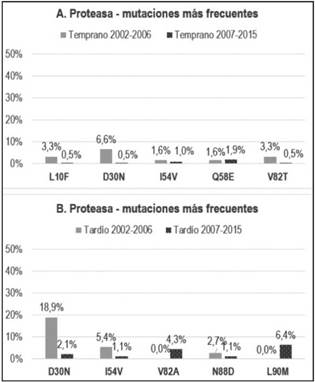
Figure 4 A. Most frequent mutations found for PI, according to period and early genotyping time. B. Most frequent mutations found for PI, according to period and late genotyping time.
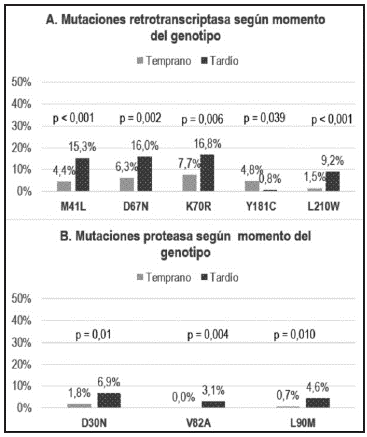
Figures 5A and 5B summarize the RT DRMs and PI DRMs, respectively, that showed a significantly different occurrence rate according to the time of resistance genotyping, confirming a higher frequency of occurrence of DRMs in the late genotyping group (except for the Y181C mutation) (Figure 5A).
Last, according to the impact on ARV families, the most frequent type of resistance in patients receiving ARVs mainly affected NRTIs (81.1%) and NNRTIs (78.9%), with a significant difference (p <0.001) between the 2002-2006 and 2007-2015 periods in the frequency of impact on NNRTIs (60.2 vs. 84.9%, respectively). The opposite was observed for the PI family, where the impact on this family was significantly greater (p < 0.001) in the 2002-2006 period (29.6%) than in the 2007-2015 period (11.2%). According to the time of genotyping, a significant difference was observed only for the PI family, with a higher frequency (p = 0.013) of impact in the late genotyping group (22.1%) than in the early genotyping group (12.5%) (data not shown).
Discussion
This study examines the pattern of appearance of resistance mutations to ARVs reported after resistance genotyping performed at the time of failure between 2002 and 2015 in Cali, Colombia. The subgroups under analysis, compared according to both the period and timing of genotyping, allowed evaluating and describing the involvement of different families of ARVs after the development of DRMs. The analysis was conducted considering both patients with late genotyping (possible abandoned virologic failures) and patients with early genotyping, performed after their first virologic failure, in compliance with current international and national guidelines for genotyping after the first virologic failure.
The results of the present study need to be considered in light of the Colombian context, as Colombia is a country with an intermediate level of resources, and in relation to the guidelines for the management of HIV/AIDS in Colombia, published in 2006 and 2014 3,9.
Before 2006, ART regimens were chosen based on the introduction of new drugs with greater potential for viral and immunological control, without considering the possible emergence of resistance associated with inadequate use due to patient-specific factors (poor adherence) or due to toxicity or poor tolerance of medications. This generated the need to document virological failure in order to implement effective rescue treatment and increase the therapeutic possibilities for patients with HIV.
The DRMs most frequently found in both genotyping periods and times were K103N and M184V in RT, affecting the NNRTI and NRTI families, respectively, and conferring different levels of resistance to the drugs of the corresponding families used in the therapeutic treatments employed in the country. A higher frequency of detection of the K103N mutation was identified in the 2007-2015 period in the early genotyping group, possibly associated with greater exposure to the NNRTIs EFV and NVP in this period. In low/middle-income countries, the most commonly used ARV combinations comprise two NRTIs and one NNRTI 10, consistent with the higher frequency of use in the sample of patients in our study. This finding helps to explain the higher frequency of the K103N and M184V mutations in RT, consistent with the pattern of use of ARVs in the sample and in previous studies 11.
As shown in the results, other mutations with high frequencies of occurrence that affect NRTIs (K70R, M41L, D67N, and L210W) and PIs (D30N and L90M), present with much greater frequency in the late genotyping group, were also relevant. This finding reflects a greater complexity of DRMs for the late genotyping group in both periods compared to that for the early genotyping group. The identification of mutation Y181C, which confers a high level of resistance to all drugs in the NNRTI family, including new ones such as ETR and RPV, was significantly more frequent in the early genotyping group during the 2007-2015 period. This result is associated with the previous use of NNRTIs such as NVP and EFV, generating cross-resistance to ETR and RPV and limiting their use as rescue therapy alternatives 12.
Resistance to the NRTI family was one of the main problems in the analyzed population because it affects not only first-line therapeutic options but also future therapeutic options when used as part of rescue regimens 13-15. Thus, DRMs to NRTIs selected by treatments that included drugs such as AZT, 3TC/FTC, ABC, D4T, DDI, and TDF (to a lesser degree) were observed, reducing the susceptibility of resistant viruses to these drugs and prolonging the time in which patients, mainly in the late genotyping group, remained in virologic failure, favoring the accumulation of DRMs. This allows establishing the importance of more frequent control of viral load and the early use of resistance genotype testing 16, with the expectation that this will limit the accumulation of mutations against NRTIs; if this is achieved, it would be feasible to use this family of ARVs in combination with another class of ARVs in a subsequent regimen.
The impact on the family of PIs was higher in the late genotyping group, with a significant difference compared to that in the early genotyping group. The probability of selecting DRMs to PIs has been reported in the literature as low due to their high genetic barrier, requiring the presence of several mutations for PIs to be compromised 17. High exposure to drugs such as NFV and IDV predominating in the 2002-2006 period could explain the documentation of resistance mutations to this group in the late genotyping group, where the majority of patients had been exposed to multiple ARV families, developing complex failures.
The accumulation of DRMs due to late documentation of therapeutic failure and increased exposure to different ARVs, among other causes, could lead to complex failures and to the selection of multidrug-resistant viruses to several ARVs. A meta-analysis reported that in patients taking medications in the NRTI and NNRTI families who were controlled at intervals of three or more months, the risk of accumulation of resistance to ARVs was increased to match that of accumulation of resistance of patients who were not virologically controlled; additionally, it was found that the frequency of resistance to NRTIs and NNRTIs increased as the time interval in which the genotype was established increased 10. Our results contribute to the evidence of the usefulness of performing resistance genotyping early after the first virological failure to prevent the accumulation of mutations.
The objective of rescue ARV regimens is to achieve sustained virological control once again, guided by analysis of the resistance profile prior to establishing the regimen. The use of three, or at least two, active drugs should be taken as a guideline, including in the regimen at least one drug from a new family to which the patient after failure has not been exposed. The therapeutic decision must be fast to prevent the progression of the infection, elevation of the viral load and greater immunological impairment 3. Important factors that may cause therapeutic failure should be corrected, offering the patient a comfortable, well-tolerated, low-toxicity regimen, always based ideally on the documentation of DRMs and the selection of drugs according to the susceptibility of the virus to the drugs and always reinforcing patient adherence.











 text in
text in