Introduction
Infective endocarditis is a disease characterized by infectious involvement of the endocardial surface of the heart that predominantly affects the heart valves but that can also involve other tissues, such as the chordae tendineae and the mural surface, or previous anatomical defects such as interauricular or interventricular communications 1. It has a low prevalence, which is calculated at 9 per 100,000 inhabitants 2,3, with a mortality rate of approximately 15-20% of those affected, which has changed little despite established diagnostic methods and treatments 2-5.
Cardiac abnormalities, whether congenital or acquired, intravenous drug use, catheters for hemodialysis or medication administration and degenerative heart disease are recognized as major risk factors for the development of infective endocarditis 1. The diagnosis of this entity is based on previously validated clinical, imaging and microbiological criteria, which when added provide a probability of having or not having the disease 6.
The main treatment regimens are derived from American and European guidelines 3,4,7-10 for cardiology and infectious diseases based on the described epidemiology in developed countries 3,4,10. In Colombia, previous epidemiological descriptions have been carried out 11. However, given the change in the causative microorganisms of this entity as well as greater population aging and greater health coverage, conducting epidemiological, clinical and microbiological characterization to obtain current country-specific results is necessary. Such characterization will also help validate or suggest changes to the empirical administration of antibiotic therapy and thus reduce the risk of therapeutic failure, with a consequent decrease in mortality, length of hospital stay and health system expenses derived from the disease.
Methods
A descriptive case series study was performed with patients with infective endocarditis in a quaternary level hospital in the city of Bogotá, Colombia. The medical records of patients diagnosed with endocarditis from 2013 to 2017 according to the ICD 10 (acute and subacute infective endocarditis (I330), unspecified acute endocarditis (I339), unspecified valve endocarditis (I38X), endocarditis and heart valve disorders in diseases classified elsewhere (I390), unspecified valve endocarditis in diseases classified elsewhere (I398)) were reviewed. To expand the search, the database of the noninvasive cardiology imaging laboratory was consulted, and reports with a diagnosis of endocarditis or vegetation were investigated for subsequent review of the corresponding medical records.
The adopted inclusion criteria were patients older than 18 years with infective endocarditis. Patients without reports of blood culture in the medical records or who were transferred to another institution before disease resolution were excluded. Data were collected from clinical history records, and each of the variables was categorized and recorded in a data collection form to be subsequently analyzed and plotted using descriptive statistics. The variables collected were divided into sociodemographics (age, sex, and rural or urban origin), comorbidities (hemodialysis, chronic kidney disease (CKD), chronic obstructive pulmonary disease, diabetes mellitus, HIV infection, heart failure, and periodontal disease), risk factors (intravenous drug use, cardiac stimulation devices, congenital cardiac disease, previous valve disease, invasive medical procedures in the last three months, steroid use, and protein-calorie malnutrition), clinical presentation (fever, de novo heart murmur, Osler' s nodes, splinter hemorrhages, Roth spots, Janeway lesions, embolic events, splenomegaly, and conjunctival hemorrhage), paraclinical findings (leukocytes, C-reactive protein, erythrocyte sedimentation rate, hematuria, rheumatoid factor, and blood cultures discriminated by the type of microorganism), echocardiographic findings (native or prosthetic valve tissue, vegetation, abscess, fistula, new valve prosthesis dehiscence, and valve insufficiency), treatment (medical or surgical, with the latter divided into emergency, urgency and elective) and last, mortality. Data were collected by two internist physicians in training specializing in cardiology and by three research assistants, who entered the data from the forms into a database in Microsoft Excel®.
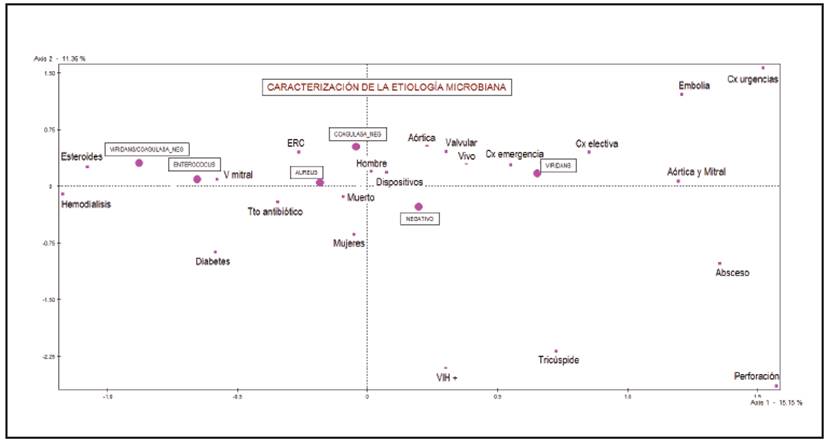
The variables were described using measures of central tendency and dispersion (when quantitative) and by absolute and relative frequencies (when qualitative). To explore a possible association between qualitative variables, multiple correspondence analysis, which searches for relationships between variables according to their proximity or similarity, was performed. In this type of analysis, the results are interpreted as a function of their relative position and proximity to dimensional spaces, without the need to meet the assumptions required by other tests (Chi-square test, Fisher's exact test, etc.), and they are represented in a factorial plane 12-14. Microorganisms were considered illustrative variables and sex, CKD, diabetes mellitus, HIV infection, hemodialysis, steroid use, type of valve involved, type of treatment received, and complications presented were considered active variables.
Statistical analyses were performed using the statistical packages Stata 13® and SPAD®.
This study was approved by the ethics committee for research on human subjects of San José Hospital.
Results
The case search and selection process for analysis is described in Figure 1; the process resulted in a total of 34 cases for analysis.
Sociodemographic description
The patients had a mean age of 59.9 years (standard deviation 15.3), and the majority was men (76.5%), with a male:female ratio of 3.2:1 (26 men and eight women); most came from urban areas (58.8%).
Clinical manifestations
In 64.7% of patients, fever manifested as the main reason for consultation. A total of 18.1% showed functional class impairment as one of the symptoms of heart failure. The most frequent signs were de novo heart murmur (67.3%), embolic events (14.7%) and splenomegaly (8.8%) (Table 1).
Table 1 Clinical and paraclinical findings in patients with a diagnosis of infective endocarditis.
| Variable | N (%) | |
|---|---|---|
| Clinical findings | ||
| Fever | 22 (64.7) | |
| De novo heart murmur | 6 (17.6) | |
| Signs and symptoms of heart failure | 6 (17.6) | |
| Embolic events | 5 (14.7) | |
| Splenomegaly | 3 (8.8) | |
| Conjunctival hemorrhage | 1 (2.9) | |
| Roth spots | 1 (2.9) | |
| Janeway lesions | 0 (0) | |
| Osler's nodes | 0 (0) | |
| Splinter hemorrhages | 0 (0) | |
| Paraclinical findings | ||
| Leukocytosis | 21 (61.8) | |
| C-reactive protein | ||
| Positive | 17 (50) | |
| Negative | 1 (2.9) | |
| Not applicable | 16 (47.1) | |
| Erythrocyte sedimentation rate | ||
| -Positive- | 6 (17.6) | |
| Negative | 1 (2.9) | |
| Not applicable | 27 (79.4) | |
| Hematuria | 10 (29.4) | |
| Rheumatoid factor | 1 (2.9) | |
Factors related to infective endocarditis
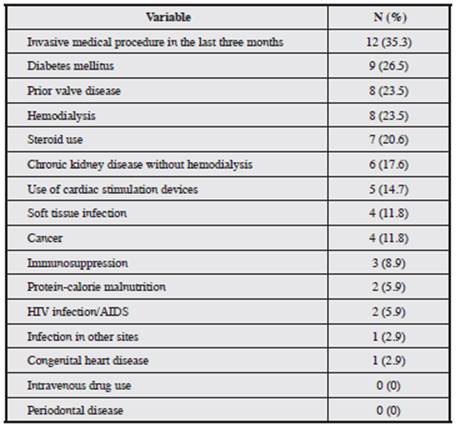
The following were found: invasive medical procedures in the last three months (35.2%), a cardiac disease preexisting the diagnosis of infective endocarditis (26.5%); diabetes mellitus (26.4%), previous valve disease (23.5%), hemodialysis (23.5%), steroid use (20.5%), CKD (17.6%), use of cardiac stimulation devices (14.7%) and cancer (11.7%) (Table 2).
Echocardiographic findings
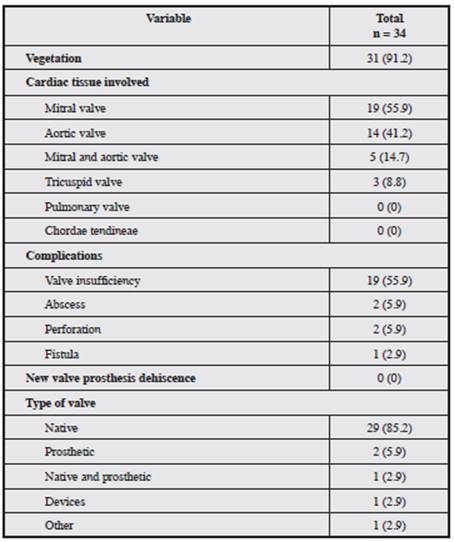
Transthoracic echocardiography detected the presence of vegetation in 31 patients (91.2%), and the most frequent valve involvement was mitral (55.8%), followed by aortic (41.1%), multivalvular (14.7%, aortic and mitral) and tri-cuspid (8.8%). Infective endocarditis of the native valve was more frequent (85.2%). These results are presented in Table 3.
Laboratory and microbiological data
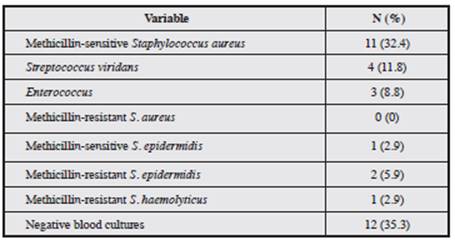
A total of 61.7% of patients had leukocytosis, and 50% were positive for C-reactive protein. Hematuria was present in 29.4% of patients (Table 1). Regarding microbiological isolates, 64.7% of the patients had positive blood cultures. The most frequently isolated microorganisms were S. aureus (32.3%), S. viridans (11.7%), coagulase-negative staphylococci (8.8%), and enterococci (8.8%); no gram-negative microorganisms were isolated. Of all blood cultures, 35.2% were negative (Table 4).
Empirical treatment
Infective endocarditis in native valves was found in 29 of the 34 patients. The most commonly used drug combination was piperacillin/tazobactam plus vancomycin (17.2%), followed by meropenem plus vancomycin (17.2%) and vancomycin plus cefepime (13.8%). Aminoglycosides were included in the antimicrobial regimens of 20.7% of the sample.
Infective endocarditis with prosthetic valve impairment and associated with the use of devices was found in three patients (prosthetic valves, n = 2; devices, n = 1). Of the patients with prosthetic valve impairment, one received management with vancomycin plus gentamicin and rifampicin, and the other received monotherapy with ceftriaxone; the patient with infective endocarditis associated with an intracardiac device did not receive an antibiotic regimen due to the presence of negative blood cultures.
Characterization of the microbial etiology
Infection by S. aureus was observed in 50% of patients with hemodialysis, in 11.1% of patients with diabetes mellitus, in 11.1% of patients with heart failure, in 41.7% of those who had undergone invasive procedures in the last three months, in 12.5% of patients with previous valve disease and in 14.3% of patients who reported steroid use. Of these, 27.3% required surgical management, and no deaths were recorded in this group.
Figure 2 shows the results of the multiple correspondence analysis. Patients who had polymicrobial infections were characterized by steroid use and being on hemodialysis. For patients in whom enterococci were isolated, there was greater mitral valve compromise, they had diabetes, and most received medical management. Patients in whom coagulase-negative Staphylococcus were isolated were characterized by being mostly men, having previous valve disease, using devices and aortic valve involvement. Patients in whom S. viridans was isolated were the group that most required surgical management.
Surgery
A total of 29.3% of patients required valve replacement surgery. Only 8.8% of all patients had an indication for emergency surgery, and 17.6% underwent elective surgery (Table 5).
Complications of endocarditis
Complications included embolic events (14.7%), valve insufficiency (55.9%) and heart failure (1.08%), valve perforation (2.9%), fistula (2.9%) and abscess (5.8%) (Table 3).
Discussion
Given the importance of infective endocarditis, it was necessary to describe the different clinical, microbiological, echocardiographic and treatment characteristics in a quaternary hospital. This description is the basis for subsequent proposals of management strategies based on the local epidemiology.
The mean age of presentation of infective endocarditis in the present series was 59.9 years (standard deviation 15.3), similar to that reported in European and American studies, where half of the patients with infective endocarditis present after age 50 8. This finding may be related to a decreased prevalence of rheumatic disease in our setting; however, this hypothesis requires studies that explore and evaluate the association between the presentation of infective endocarditis and the presence of rheumatic heart disease as a pre-existing condition. These results differ from those reported by Senior et al. 11 in Medellín, where the young population was mainly affected, which could indicate a higher frequency of rheumatic disease in this population at the time that series was evaluated and/or an increased frequency of risk factors such as intravenous drug use compared to that in our series.
The male:female ratio showed that males were predominantly affected (3 to 1), which is consistent with the literature 15,16. Among the clinical manifestations, fever was the most frequent reason for consultation (64.7%), followed by functional class deterioration. De novo murmurs and splenomegaly were the most frequently encountered physical examination findings; these are typically the clinical findings described in different reports 16,17, which suggests the need to obtain an adequate clinical history and perform a physical examination for a timely diagnosis.
Among the risk factors for infective endocarditis described in the literature 18,19, invasive procedures in the last three months was the most frequent (35.2%), followed by diabetes mellitus, prior valve disease, hemodialysis and steroid use. Many of these risk factors are also significant for infective endocarditis due to S. aureus18, the main infective endocarditis agent in the world and in our series to date 20.
The detection of vegetation in our study was higher (91.2%) than that found in the literature (approximately 60%) 21. This can be explained by the way in which the data were collected for this series, given that the cases were identified through an echocardiography database using vegetation as one of the keywords, which may have led patients with criteria for definitive infective endocarditis other than vegetation to not be included in our analysis.
Valvular involvement, as in the epidemiology described at the global level, was primarily mitral, followed by aortic valve involvement 11,15,16. Although there were no intravenous drug users in our series, the tricuspid valve was involved in 8.8% of cases, indicating the likely presence of other risk factors for infective endocarditis in our patients, such as hemodialysis or other invasive procedures.
As described in the literature, native valve infective endocarditis was the most frequent (85.2%); however, the frequency reported for prosthetic valves was lower (5.8%) than that found in other studies (12%) 22.
The paraclinical findings most often presented were leukocytosis, C-reactive protein and hematuria. This is consistent with a Colombian series 11,17 and with findings from other studies worldwide 17. However, in the majority of patients, other clinical laboratory tests that are part of the minor criteria were not performed, such as the rheumatoid factor, which can improve the proper categorization of infective endocarditis diagnosis as definitive, possible or discarded.
The positivity of blood cultures was low (64%) compared to those in European and American studies but very similar to that reported in Colombia 11. This low frequency may be explained by the fact that patients could receive antibiotics prior to blood cultures, a variable that was not assessed in our study. In addition, no slow-growing or non-culturable microorganisms were investigated.
The most frequent microorganism was S. aureus, which indicates that the globally reported switch from streptococcus as the main microorganisms in the past to S. aureus5 is also found in the evaluated population and is probably related to the same reasons, such as increased invasive procedures (vascular catheters, intracardiac devices, etc.), the main risk factor present in our series.
The empirical antibiotic therapy used in our series differs from that recommended in guidelines 8. The use of broad-spectrum antibiotics as the first-line treatment was the most frequent; this may be due to the more critical condition of the patients or to the greater frequency of risk factors for resistant microorganisms in the treated patients. These data were not evaluated in our series, but their study is key to promoting the rational use of antibiotics in any institution.
Infective endocarditis of prosthetic valves in our series was caused by S. aureus, and only one of these patients received the complete antibiotic therapy regimen recommended by current guidelines 8. The second patient did not receive combined rifampicin. All S. aureus isolates were susceptible to methicillin, and only 54.6% of cases were de-escalated to oxacillin after culturing. All this could indicate the need for standardization of management in the different contexts of infective endocarditis and the generation of awareness of de-escalating antibiotics when sensitivity allows.
The most frequent complication was insufficiency of the affected valve (55.9%) and symptoms of heart failure and embolic events (14.7%), in agreement with the literature, which reports cardiac complications as the most common, followed by neurological events 23,24.
In our series, the percentage of patients undergoing surgery was lower (29.3%) because for the majority of studies, half of patients with infective endocarditis required surgical treatment due to serious complications 8,23. This lower frequency of serious complications requiring surgical management could explain the low intrahospital mortality (8.8%) compared to the stable rate reported in the literature in recent years (15-20%) 6.
While this series included 34 patients over a period of four years in a quaternary hospital, this is a frequency comparable or greater than that reported by other series, except the study by Senior et al., in which 92 patients were included over a longer period (11 years) and from three referral centers. The sizes of these series are explained by the low prevalence of infective endocarditis. As in all case series, the main limitation of this study is related to possible information bias because the data were collected retrospectively; nevertheless, objective measurements of the majority of the outcomes can decrease the occurrence of bias.











 text in
text in