Introduction
The population pyramid has been changing over the last few years, with a significant increase in the number of older adults: an estimated 2 billion people at or above the age of 60 worldwide between 2015-2050 1. In Colombia, according to DANE [the Colombian national statistics department] records, there were 5,332,644 inhabitants over the age of 60 in 2015 and it is predicted that this figure will reach 6,435,899 by 2020, with an aging index of 49.78 2. Sarcopenia and frailty are geriatric syndromes which often affect this population group with significant implications for the health and quality of life of those affected.
Sarcopenia is characterized by progressive generalized loss of muscle mass, strength and physical performance 3. Frailty results from progressive deterioration of multiple physiological systems, with an altered homeostatic reserve and a reduction in the organism's ability to withstand stress, increasing vulnerability to adverse health events 4,5. These two conditions are considered to be mutual risk factors and may coexist in the same individual 6, leading to a greater probability of negative outcomes such as limited ability to carry out activities of daily living, osteoporosis, falls, extended hospital stays, readmissions and death 7.
The prevalence of these entities varies widely in the literature and is probably affected by age, sex, the environment studied and the methods used to measure the variables required for the definition of each one 8. Sarcopenia is generally found in a broad range from 0.9-32.8% 9-11; in outpatients it varies from 1-29% and in institutionalized patients from 14-33% 12. The prevalence of frailty ranges from 4-16% in adults at or above the age of 65 13. Data are scarce in the hospital setting, despite their proven impact on clinical outcomes, morbidity and mortality 14,15. This study seeks to describe the prevalence of sarcopenia and frailty, and the clinical characteristics of adults over the age of 65 with these conditions under the internal medicine service of the Fundación Valle del Lili.
Materials and methods
This was a descriptive, prospective cross-sectional study. Men and women were included who were 65 years old or older and hospitalized under the internal medicine service at the Fundación Valle del Lili (a tertiary-care institution located in the city of Cali, Colombia) between September 1, 2016 and February 28, 2017.
Participants were identified through the daily admissions census, selecting those who agreed to participate and signed an informed consent for the measurements. Patients who had conditions which prevented the measurement of essential variables for the definition of sarcopenia and frailty were excluded, such as those with pacemakers and amputees (because of difficulty in measuring muscle mass), those with primary myopathies and upper limb involvement which made strength measurement difficult, and those with an altered state of consciousness. A database was constructed for electronic recording using BDClinic, which was subsequently transferred to the Microsoft® Excel® 2014 program. Demographic variables were included such as age, sex, type of healthcare insurance: contributory system (enrollees able to pay for access to health care), subsidized (the poorest population in the country, unable to pay; their access to healthcare services is government subsidized), prepaid medicine (enrollees in additional healthcare plans, optional and voluntary benefits), and special system (enrolled in exceptional healthcare programs who, because of their employment have a special healthcare system). Other variables considered included education; socioeconomic level; living situation; medical history such as hypertension, diabetes mellitus, chronic obstructive pulmonary disease, cardiovascular diseases, arthrosis, dementia, eye diseases, hearing disorders, and the use of medications for dementia and insomnia; and data related to the hospitalization such as the admitting diagnosis, admission site (emergency room, intensive care unit, surgery) and days of hospitalization. The measured variables were: mass, muscle strength and physical performance.
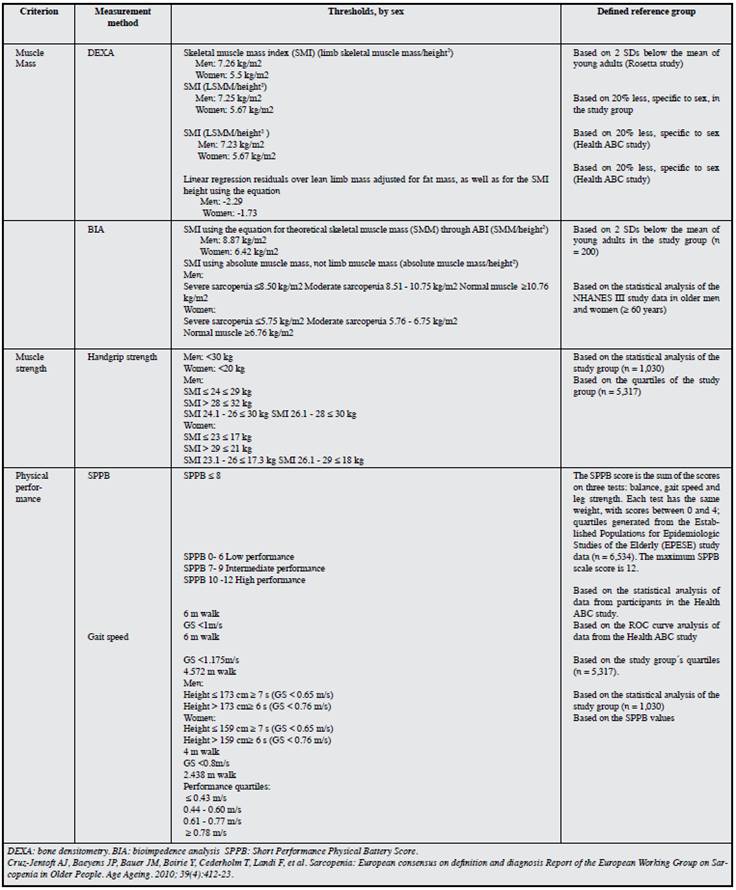
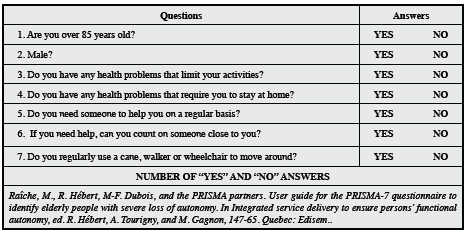
Sarcopenia was defined according to the 2010European Working Group on Sarcopenia in Older People(EWG-SOP) diagnostic criteria: criterion 1 plus criterion 2 or 3, where 1 is decreased muscle mass, 2 is decreased muscle strength and 3 is low physical performance 8,9. Muscle mass was evaluated using bioimpedance to establish the skeletal muscle mass index (SMI), with the following cutoff points: men: severely diminished ≤ 8.5 kg/m2, moderately diminished: 8.51-10.75 kg/m2and normal muscle: ≥10.76 kg/m2; women: severely diminished: ≤ 5.75 kg/ m2, moderately diminished: 5.76-6.75 kg/m2, and normal muscle: ≥6.76 kg/m29. Muscle strength was determined by handgrip using a digital dynamometer. It was defined as decreased in men if it was < 30 kg and in women if it was < 20 kg 9. Physical performance was measured with theShort Physical Performance Battery (SPPB) which assesses balance, gait, strength and resistance, considering a score≤ 6 points to be low performance 9. Bioimpedance was used for measuring muscle mass because it was easy to measure in a hospital bed and was less expensive than densitometry and tomography (Annex 1). Frailty was diagnosed using the PRISMA 7 questionnaire 16, considering those with a score equal to or greater than three on the following questionnaire (each positive answer worth one point) to be frail:
Are you older than 85 years?
Male?
In general, do you have any health problems that limit your activities?
Do you need someone to help you on a regular basis?
In general, do you have any health problems that require you to stay at home?
If needed, do you have someone close you can count on?
Do you regularly use a cane, walker or wheelchair?
This type of questionnaire was used due to its good sensitivity (83%) and applicability in the hospital context (where other scales are difficult to apply), despite having a low specificity 17 (Annex 2).
For the statistical analysis, quantitative variables were reported as averages or medians with standard deviation and interquartile range as measures of dispersion, according to their fulfillment of assumptions of normality using the Kolmogorov-Smirnov test. Categorical variables were described in absolute values and percentages. Frequency tables were constructed according to the presence or absence of sarcopenia and frailty. They were compared with each of the variables using Student's t-test or the Mann-Whitney-Wilcoxon test for quantitative variables and Chi square or Fisher's exact test for categorical variables, according to the fulfillment of assumptions. The statistical analysis was done with STATA 13. This study was approved by the institutional biomedical research ethics committee.
Results
A record of 141 eligible patients was obtained, corresponding to 76.5% of individuals 65 years old and above in the general internal medicine wards from September 1, 2016 to February 28, 2017. Of these, 16.3% were excluded because they did not meet the conditions for muscle mass measurement (one had amputated lower limbs and two had pacemakers, which interfere with muscle mass measurement using bioimpedance), and the other 13 were excluded because they did not have an accompanying adult to complete the informed consent, leaving 124 participants for analysis.
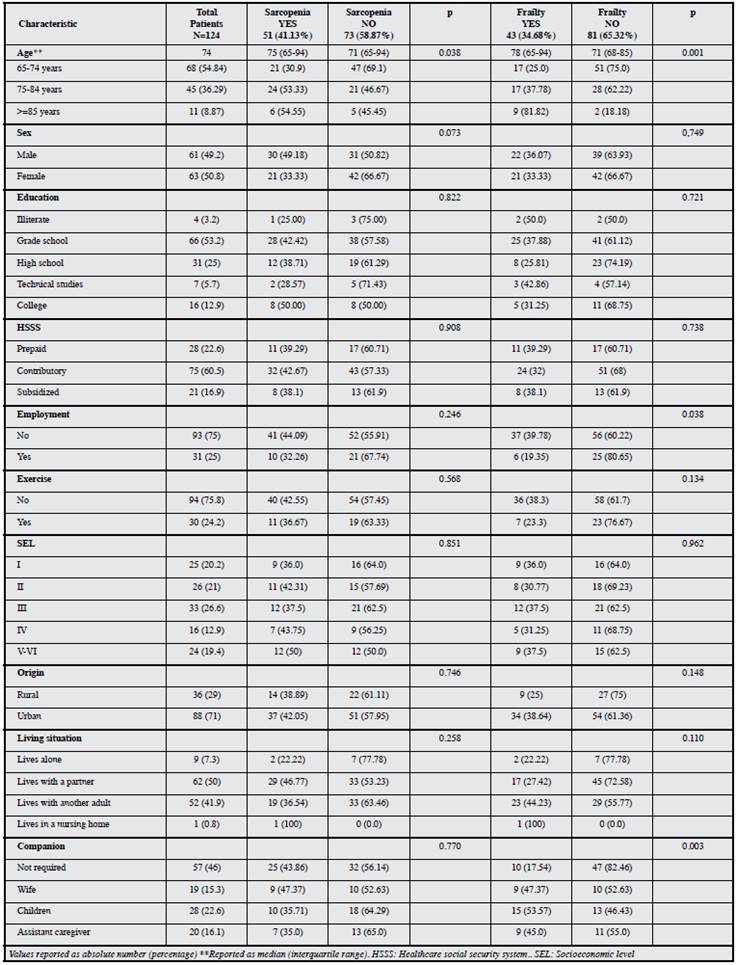
The prevalence of sarcopenia was 41.13% (51/124 patients) and of frailty was 34.68% (43/124 patients). Both conditions were found in 18.55% (20 out of 124). The population characteristics are shown inTable 1. The median age was 74 years. The distribution by sex was 50.8% women (63/124) and 49.2% men (61/124). A total of 60.5% of these individuals belonged to the contributory system, 71% were from urban areas, and 54% needed a constant companion. The prevalence of sarcopenia increases significantly with age, p= 0.038 (confidence interval, CI 1.30-2.33), as does frailty (p=0.001, CI 1.80-3.31). Altogether, 33.3% of women and 49.18% of men had sarcopenia; the gender relationship was not statistically significant. Frailty was found in 36.07% of men and 33.36% of women; the sex-frailty relationship was not significant (Table 1).
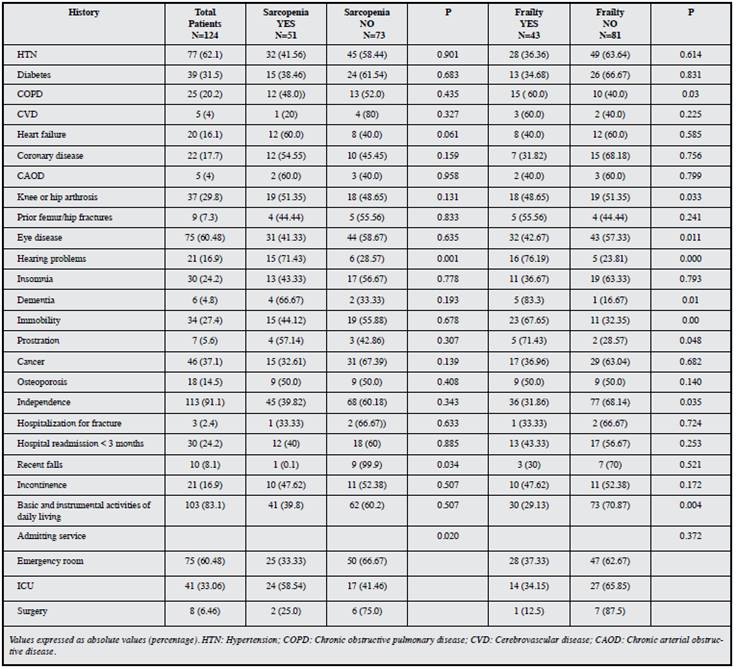
The most commonly found concomitant diseases were hypertension, diabetes and chronic obstructive pulmonary disease (COPD), none of which were significantly associated with sarcopenia. These diseases were not significantly associated with frailty, either, except for COPD which was significantly related (p=0.03 with a CI of 1.59-2.01). Altogether, 37.1% of those studied had some type of malignancy which was not significantly related to these geriatric syndromes; 24.2% of the patients had been hospitalized within the three months prior to the current admission, with no significant relationship between this condition and having or not having sarcopenia or frailty (Table 2). Eye diseases were found in 60.48% of those studied, with no significant association with sarcopenia, but significantly associated with frailty; 16.9% had auditory disorders, a condition which was significantly associated with these syndromes.
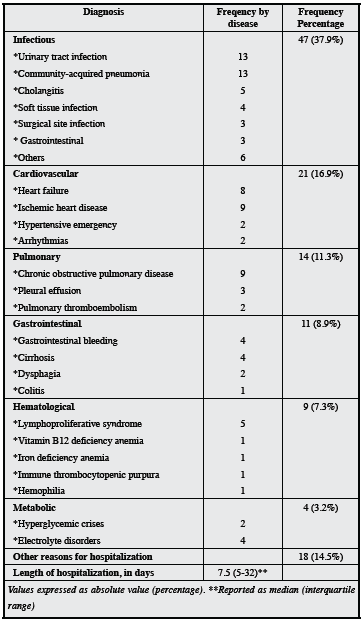
Most of the hospitalized patients were admitted through the emergency room (60.5%). The median hospitalization was 7.5 days, with a range of 1-32 days. Infectious causes (urinary tract infection and pneumonia) were the most frequent causes of hospitalization (Table 3).
Discussion
The population pyramid has undergone significant changes in the last few years 1. The older adult population has been increasing, and at the same time entities such as sarcopenia and frailty are more frequent. These conditions must be identified and treated promptly to minimize the health consequences for the affected individuals.
The literature is congruent in highlighting that these syndromes are independent risk factors for adverse health outcomes, leading to diminished quality of life and increasing health care costs 14,18. In our study, the prevalence of sarcopenia was 41.13%, which differs from the published results. This difference is probably due to the study population or the methods used for evaluating this condition; however, the results may also be due to real differences. Most studies have been carried out in the community or in nursing homes. According to the systematic review published in 2014 12 which evaluated 18 studies on the prevalence of sarcopenia, using the EWGSOP criteria, sarcopenia was found in 1-29% of older adults in the community, and in 14-33% of those in chronic care institutions. This coincides with what was reported by Tasar 33.6% 19, Aras 32.8% 20 and Landi 24.5% 10 in similar environments.
In Colombia, it has been estimated at 11.5% in a population of older adults evaluated in the community 21. There are few studies in acute care hospitals, with an estimated 10% of patients possibly being affected 22; however, a study of acutely ill patients hospitalized for malnutrition found sarcopenia in 21.4% of patients, while gait speed or handgrip strength were not able to be measured in 22.3%, thus lacking at least one of the EWGSOP criteria for diagnosis. Therefore, it may not be possible to satisfactorily apply these criteria to a relevant proportion of hospitalized patients 23, leading to an underreporting of cases. The prevalence we found was significantly greater than that reported in the previously mentioned publications, probably related to the acute condition and types of illnesses treated in the institution, which, being a tertiary-care center, handles the most severe cases. Thus, in this case, the variables assessed, such as muscle strength and physical performance, may have a greater probability of being impaired. Another possible influencing factor could have been the method used for defining this entity. In the study published by Gariballa 24, muscle function was only measured using handgrip pressure, while in our population, the physical performance test was also evaluated.
Generally, in most studies, sarcopenia is higher in women. In India, in a tertiary-care hospital, there was an estimated prevalence of 15.3% in men and 20.5% in women 22. In the SABE study, carried out in Colombia, the condition was also higher in women (12.6% vs 9.8%), contrary to what we found in our study, where men were the most affected (49.18% vs 33%), similar to what was reported in other studies performed in nursing homes 10,20,23. The gender difference, in our study, was not statistically significant. Age is an important determinant for sarcopenia; prevalence increases with age, a finding which coincides with most reported studies. Salvá et al. found a linear tendency with the condition increasing with increasing age 25, similar to what was documented in our study. With regard to diseases and other health conditions affecting the study population, cardiovascular diseases, arthrosis, hearing problems and dementia were found to be the most frequent in patients with sarcopenia. However, there was no statistically significant relationship between them, possibly due to the sample size.
A significant relationship was found between patients admitted to intensive care and sarcopenia, a finding which so far has not been evaluated in other studies. In general, infectious diseases were the most frequent reason for hospitalization, a variable which has not been evaluated in other studies. It is important to highlight this point as a possible factor related to the presence of sarcopenia.
The prevalence of frailty was 34.68%, a figure higher than that reported in other studies. The SABE study found 9.4% 21; however, this study was carried out in older adults in the community and there are no studies to date which measure this condition in the hospital setting. Another factor which could have affected the difference is the measuring instrument: they used the frailty phenotype scale developed by Fried et al. 26, while in our study we used the PRISMA 7 scale 17,27. These scales evaluate different aspects; there is no unified instrument to measure this condition in hospitalized patients. The prevalence of frailty increases with age, and the frequency was similar between men and women. These findings are similar to those of other studies 21. The variables which were significantly associated with frailty were COPD, eye diseases, hearing problems and dementia; these findings have not been evaluated in previous studies, but are conditions which cause greater dependency.
Finally, sarcopenia and frailty are known to be closely related as geriatric syndromes and may coexist. In In our population, these two entities were found simultaneously in 18.55%, a percentage similar to that found in the SABE study (17%), which suggests a possible relationship in the presence of these two conditions. However, in a study performed in the Netherlands 27, the intraindividual correlation between sarcopenia and frailty was low, possibly explained by the difference in pathophysiology, since the first is based on musculoskeletal alterations, while frailty has a complex multifactorial cause including, according to the assessment tool, emotional and cognitive elements. More studies with a larger population are needed to determine this relationship.
Conclusion
The prevalence of sarcopenia and frailty increases with age. The first was more frequent in men and the second was more frequent in women. The frequency of these conditions was higher than that reported in the available literature. This may be explained by the assessment setting, where acute illness leads to significant physical and metabolic alterations which ultimately result in loss of muscle strength or mass, decreased physical performance and, consequently, a greater propensity to frailty.
Ethical responsibilities
Protection of persons and animals. The authors declare that no experiments on human beings or animals were performed for this research study.
Data confidentiality. The authors declare that they have followed their work center's protocols on the publication of patient data. Right to privacy and informed consent. The authors declare that no patient data appear in this article.











 texto em
texto em