Introduction
Chronic kidney disease places a high burden of morbidity and mortality on the patients who suffer from it. This is why the rate of hospital admissions for any cause is 147% higher for this group compared to those who do not have kidney disease 1. Likewise, there are differences in the frequency of hospital admissions, depending on the severity of the kidney disease. In 2016, patients with Stage 1 and Stage 2 disease had 478 registered admissions to the emergency room per 1,000 inhabitants; for Stage 3, there were 565 for every 1,000; and for Stage 4 and 5 (non-dialysis), 863 admissions were reported for every 1,000 1. Finally, patients on hemodialysis and peritoneal dialysis had 1.7 hospitalizations/year 2.
For the same year, in the United States, patients on hemodialysis were reported to have had an average of 11.3 inpatient days, while patients on peritoneal dialysis had 12.2 days 2. During the same year, in Chile, patients on hemodialysis were found to have an average of 15 inpatient days 3. In Colombia, 9.43 days have been reported for patients on hemodialysis and 8.29 days for patients on peritoneal dialysis 4. Cardiovascular events are the main source of hospitalization and death in this population group; in the USA they represent 40% 5, in Argentina 46.1% 6, in Japan 26.5% 7, in Chile 14% 3, and, finally, in Colombia 19.38% of these events 4.
The second group of illnesses that cause the most hospitalization and death in patients with end stage renal disease are infections, presenting in people who have various immune system disorders secondary to uremic toxins 8,9 which impair their response to different microorganisms. In Argentina they make up 21.3% 6, in Japan 20.8% 7, in Chile 13.7% 3 and, finally, in Colombia (taking treatment-related infections into account), they make up 27.91% 4. The third group of illnesses that cause hospital admissions are distributed among gastrointestinal diseases, causes related to renal therapy and cancer events, varying according to the country where they are registered.
Methods
This is an observational, analytical, dynamic, historical cohort study. Clinical records were reviewed of patients with end stage renal disease on hemodialysis (cohort 1) and peritoneal dialysis (cohort 2) renal replacement therapy who were admitted to Hospital Universitario Mayor between June 1, 2015 and December 31, 2016. Only those who had been treated for infectious diseases were selected. To evaluate the inpatient stay needed to treat this group of diseases, two dates were taken into account, namely: 1) the date of admission to the emergency room and 2) the date of hospital discharge.
The inclusion criteria were: a) patients with advanced chronic kidney disease on hemodialysis or peritoneal dialysis renal replacement therapy for three or more months, b) 18 years old or older, and c) a chief complaint and current illness compatible with an infectious process, regardless of the site of origin. The exclusion criteria were: a) pregnant women, b) patients for whom an infectious reason for admission was ruled out during the course of hospitalization.
The Epidat statistical program was used to calculate the sample size. This process involved hypothesis testing and comparison of means. This technique was used since differences were sought in the average number of inpatient days needed to treat infectious diseases in patients on hemodialysis and peritoneal dialysis. A confidence level of 95% and power of 80% were selected, yielding a sample size of 242 patients distributed as follows: 172 on hemodialysis and 69 on peritoneal dialysis. The patients who entered the study were included through non-probabilistic methods.
Statistical analysis of the data
The whole sample was characterized using descriptive statistical methods. Categorical variables were reported using absolute frequency and relative frequency. For quantitative variables, normality was proven using the Kolmogorov-Smirnov statistical test. For quantitative variables with a normal distribution, the data were reported using mean as the measure of central tendency and standard deviation as the measure of dispersion. For quantitative variables with a non-normal distribution, the data were reported using the median as the measure of central tendency and interquartile range as the measure of dispersion.
The Chi square test for two independent samples was used to detect differences between the patients on hemodialysis and those on peritoneal dialysis, when evaluating categorical variables, since the expected values were greater than five. However, Fisher's exact test was used to compare central nervous system infections between the two types of dialysis, since expected values lower than five were found. Similarly, the Mann-Whitney U test was used to detect differences between the patients on hemodialysis and those on peritoneal dialysis, when evaluating a quantitative variable.
This study was submitted to and approved by the RTS-Baxter human research ethics committee and the research committee of the Hospital Universitario Mayor.
Results
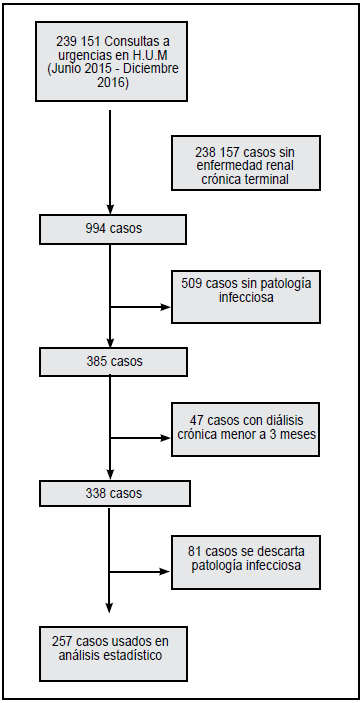
During the 18 months from June 1, 2015 to December 31, 2016, 994 patients with chronic kidney disease on renal replacement therapy were admitted to the emergency room at the Hospital Universitario Mayor (H.U.M.). After evaluating the inclusion and exclusion criteria, 257 patients were obtained and included in the statistical analysis. The patient selection flowchart is shown inFigure 1.
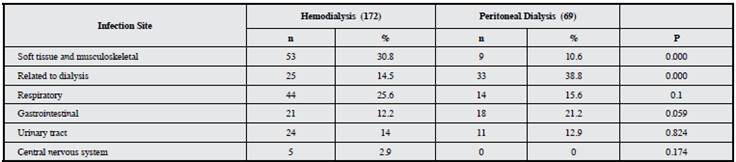
The baseline characteristics of all the patients included in the statistical analysis, including demographic, hospital admission and infection site characteristics, as well as those evaluated during the hospital stay, are shown inTables 1and4.
Table 2 Characteristics on hospital admission. Ca: Calcium, Na: Sodium, Hb: Hemoglobin, P: Phosphorus, Hb A1c: Glycated hemoglobin.
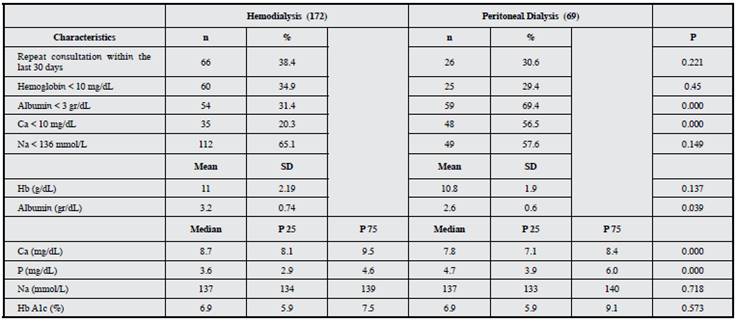
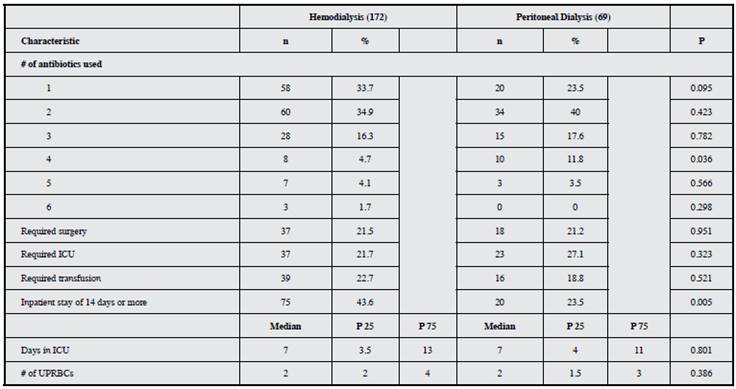
Table 4 Characteristics during hospitalization, by type of dialysis therapy. ICU: Intensive care unit, UPRBCs: Units of packed red blood cells.
The quantitative variables of hemoglobin g/dL, serum calcium mg/dL, serum albumin g/dL and serum sodium mmol/L were converted to categorical variables in order to determine which patients had the following on admission: anemia, hypocalcemia, hypoalbuminemia or hyponatremia, respectively. Furthermore, the infectious diseases were categorized in six large groups, namely: 1: soft tissue and musculoskeletal infections (including diabetic foot); 2: dialysis-related infections (including therapy-induced complications such as infectious endocarditis); 3: respiratory tract infections; 4: gastrointestinal and abdominal infections not related to dialysis; 5: genitourinary system infections; and 6: central nervous system infections (including spondylodiscitis).
Finally, a table was constructed, summarizing various events documented throughout the hospital stay which were related to the various infectious diseases that led to the emergency room consult. These include the proportion of patients who required intensive care unit (ICU) management, the proportion of patients who required surgery to control the infectious process, or the number of patients who had hospital stays longer than 14 days.
Blood cultures were taken from 113 (44%) patients; 80 (70.6%) were reported as negative,Staphylococcus aureus (S. aureus)was isolated in 12 (10.6%),Escherichia coli (E. coli)was isolated in five (4.4%),Klebsiella pneumoniae (K. pneumoniae)was isolated in three (2.7%), andEnterobacter cloacae (E. cloacae) was isolatedin two (1.8%).Finally, in the last 9% of cultures, the following microorganisms were found, evenly distributed (one each, 0.9%): Enterococcus faecalis (E. faecalis), Serratia marcescens (S. marcescens), Staphylococcus epidermidis (S. epidermidis), Staphylococcus hominis (S: hominis), Staphylococcus lugdunensis (S. lugdunensis), Staphylococcus spp, Streptococcus agalactiae (S. agalactiae), Streptococcus pneumoniae (S. pneumoniae), Aeromona hydrophila, andS. aureus + S. epidermidis, S. aureus + E. coli.
Urine cultures were also taken from 41 patients (16%); 14 (31.1%) were reported as negative,E. coliwas isolated in nine (22%),K. pneumoniaewas isolated in three (7.3%),Proteus mirabiliswas isolated in two (4.9%),S. aureuswas isolated in two (4.9%) and, finally, in the last 26.4%, the following microorganisms was found equally distributed, one (2.4%) each:E. faecalis, E. faecium, E: cloacae, Pseudomona aeruginosa, S. marcescens, S. agalactiae, Citrobacter amalonaticus, Candida tropicalis, Candida glabrata, E: coli + E: faecalis, and Pseudomona aeruginosa + Aeromona hydrophila.
Secretion cultures were also taken from 17 patients (6.6%): from a lower limb in six (35.3%), a surgical wound in five (29.4%), an abscess in three (17.7%), oral-tracheal secretion in two (11.8%), and the urethra in one (5.8%). Of these samples, the following reports were obtained:S. aureuswas isolated in six (35.3%),E. coliwas isolated in two (11.6%) and, finally, in the last 53.1%, the following microorganisms were evenly distributed, one each (5.9%):Proteus mirabilis, Morganella morganii, K. pneumoniae, Haemophilus influenzae, E. faecium, E. cloacae, E. cloacae + Citrobacter freudii, E. coli + K. pneumoniae, and Pseudomona aeruginosa + Proteus mirabilis.
Discussion
This study describes the characteristics of infectious disease hospitalizations in a population of patients with Stage 5 chronic kidney disease receiving renal replacement therapy through either hemodialysis or peritoneal dialysis who were admitted to the emergency room at the Hospital Universitario Mayor (Mederi). A literature review of the average hospital stay in this group of patients showed that this epidemiological indicator is presented as an average obtained from the inclusion of various groups of unrelated diseases (such as infections, cardiovascular diseases, cancers and gastrointestinal diseases, among others), making hospitalization a data point which summarizes entities that are hard to compare and which could result in incorrect therapeutic objectives 5-7,10.
In our opinion, this is one of the few existing studies which seeks to evaluate the length of hospital stay required to treat infectious diseases. Thus, it was found that hemodialysis patients require longer hospital stays than peritoneal dialysis patients, a similar finding to that of Sanabria et al. 4. This may be due to the fact that peritoneal dialysis patients are more likely to have a home hospitalization plan and therefore have fewer inpatient days.
In addition, the proportion of respiratory, central nervous system and urinary tract infections in both types of renal replacement therapy were found to be very similar to those reported by other authors 11,12. On the other hand, contrary to what other studies report, the proportion of infections related to renal replacement therapy was lower, which could be secondary to the high quality standards (in matters related to the type of dialysis access) required of dialysis providers in the country, due to its high cost. Furthermore, the percentage of soft tissue infections was found to be greater than that reported by the same authors, which indicates the need to reinforce the management of diseases such as diabetic foot within the patients' outpatient care.
From a microbiological isolation standpoint, the main microorganisms isolated from blood cultures wereStaphylococcus aureusin the group ofGram positives and E. coliin the group ofGram negatives,which is very similar to what is described in the literature 13,14. However, it is noteworthy that in 70% of cases, the blood culture was negative, which could be interpreted as a greater performance of this test in infections which do not cause bacteremia. Nonetheless, it opens the door to continued research related to infectious events associated with patients with chronic kidney disease.
In conclusion, we believe that more detailed knowledge of the causes and characteristics of hospital admissions for patients with Stage 5 CKD who are on hemodialysis and peritoneal dialysis is essential to direct the clinical measures needed to improve the clinical outcomes of outpatient treatment, avoid hospital admissions and optimize their management. In our particular case, we observed that patients on peritoneal dialysis require fewer inpatient days to resolve infectious diseases and that therapy-related infections have a lower incidence than reported globally; however, diabetic foot soft tissue infections are a problem which needs to be given special attention in our country's renal units.











 text in
text in