Introduction
Scleroderma is an autoimmune disease of unknown etiology which mainly affects the skin 1 but may also involve multiple organs including the lungs, heart, gastrointestinal tract, kidneys and musculoskeletal system 2. Scleroderma renal crisis (SRC) is one of its most serious complications, with high morbidity and mortality 1. It is characterized by malignant hypertension and rapidly progressive renal failure ending in renal replacement therapy or death. Blood pressure control with angiotensin converting enzyme inhibitors (ACE inhibitors) is the current treatment of choice which, if started early, may halt the progression of renal failure in most cases 3. For patients with end-stage renal disease (ESRD), treatment options include dialysis and kidney transplantation 4. However, little has been studied regarding the outcomes of kidney transplantation in patients with scleroderma and the recurrence rate of SRC and evidence is very scarce. The case of a kidney transplant patient with SRC who was successfully treated with ACE inhibitors is presented below.
Clinical case
This patient was a 64 year-old female with a history of ESRD secondary to diffiuse scleroderma, for which she received a cadaveric donor kidney transplant in 2002. She was given immunosuppressant treatment with cyclosporine, mycophenolate and prednisone, which was changed in 2011 to everolimus (meta levels 5-8 ng/mL) and prednisolone 5 mg/day. The patient's comorbidities included high blood pressure being treated with amlodipine and clonidine, pulmonary hypertension and hypothyroidism. In 2017, she was seen in the emergency room for a one-week history of headache, asthenia, adynamia and oliguria. On blood pressure self-monitoring at home, the patient had seen a progressive increase in arterial pressure over the last few days. Hypertensive crisis was documented on admission (with figures up to 180/110 mmHg) along with acute deterioration of renal function with elevated creatinine up to 2.2 mg/dL (baseline 1.2 mg/dL). Her physical exam revealed cutaneous scleroderma findings on her face (microstomia, rhagades), ankle edema, sclerodactyly and telangiectasias on her extremities. Complementary paraclinical exams showed proteinuria 75 mg/dL (1,200 mg in 24 hours), microhematuria with five per field, a complete blood count with no anemia or thrombocytopenia, and a blood smear without schistocytes. A doppler of the kidney graft had elevated resistance indices up to 0.8 in segmental arteries, without renal artery stenosis, signs of thrombosis or vascular flow abnormalities. She had positive autoimmune tests (homogeneous pattern ANA 1:1,280, and nucleolar pattern ANA 1:640, anti-Scl-70: 181). Graft dysfunction secondary to an active infectious process, dehydration or rejection was ruled out. Thus, the diagnosis was considered to be scleroderma renal crisis of the transplanted kidney, and treatment was begun with high-dose enalapril at 40 mg/day. She improved progressively with controlled blood pressure (130/80 mmHg) and decreased creatinine to baseline levels (1.2 mg/dL) after three days of treatment.
Discussion
Scleroderma is a connective tissue, autoimmune, multisystemic, rare disease which disproportionately affects women of childbearing age 2. It is characterized by three different pathophysiological processes: vascular disease, immune activation and inflammation, and skin and subcutaneous tissue fibrosis. However, it also frequently affects internal organs such as the heart, lungs, kidneys and gastrointestinal tract. This disease can have three phenotypes: limited, diffuse and syndromic overlap with lupus, myositis and inflammatory arthritis 5,6.
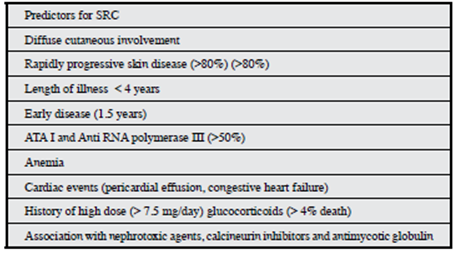
Scleroderma renal crisis is one of the most feared complications, considered a medical emergency, which presents with malignant hypertension and acute kidney injury. Other related clinical characteristics include microangiopathic hemolytic anemia, proteinuria, heart failure and hypertensive encephalopathy. It is suggested that this disease be diagnosed when a scleroderma patient presents with new onset moderate or severe hypertension and/or an acute increase in serum creatinine 3,5-9. Scleroderma renal crisis is rarely the initial manifestation of the disease, and may often present during the first four years after diagnosis. However, in the African American and male population it may present late. The risk factors for SRC are described inTable 1 5,6,8.
There is no standard definition of SRC to date. The International Scleroderma Renal Crisis Survey (ISRCS) panel of experts suggests the following clinical parameters, updated in 2014:
Systolic blood pressure (SBP) ≥ 140 mmHg or an increase ≥ 30 mmHg
Diastolic blood pressure (DBP) ≥ 90 mmHg or an increase ≥ 20 mmHg
Increased serum creatinine ≥ 50% over baseline, or > 120% of the upper limit of normal
Proteinuria ≥ 2 + on urine dipstick or a proteinuria/creatinuria ratio ≥ the upper limit of normal
Hematuria ≥ 2 + on urine dipstick or ≥ 10 red blood cells per high power field
Platelet count < 100,000/mm3
Hemolysis (schistocytes or red blood cell fragments on a peripheral blood smear or elevated reticulocyte count)
Scleroderma renal crisis is the result of genetic susceptibility added to multiple insults to the renal vasculature; however, its etiology is not clearly known 1. Platelet factors have been proposed as the cause of increased vascular permeability, fibrin deposits and collagen formation, which lead to narrowing of the vascular lumen and decreased cortical blood flow. This, together with episodes of vasospasm, fosters juxtaglomerular apparatus hyperplasia and increased renin levels 3,6-11. Kidney biopsy is not required to confirm the diagnosis of classical SRC. When a biopsy is performed, the findings show arteriolar endothelial injury and ischemia. In addition, small vessel lumen narrowing is seen, caused by endothelial cell proliferation and the deposit of "mucoid" extracellular material, which leads to the classical onion bulb lesion. If the clinical disease progresses with ongoing kidney ischemia, glomerulosclerosis and interstitial fibrosis are produced 9-11.
The morphological diagnosis of recurrent SRC following transplant can be challenging. Various pathological processes can produce a similar histological appearance, including malignant hypertensive vascular disease, vascular rejection, chronic transplant glomerulopathy and calcineurin inhibitor nephrotoxicity 3. Recurrences of SRC in kidney transplant patients have been reported in 2-50%, associated with early failure and loss of the renal graft 5,8,9,12.
The predictors of and risk factors for recurrent SRC in renal allografts have not been well studied. Some authors suggest that signs of active scleroderma (skin hardening, anemia, pleuropericarditis with pericardial effusion) are risk factors, together with an elapsed time of less than two weeks between the SRC and ESRD in native kidneys 4,8.
The experience with regard to rejection prevention following transplantation in patients with SRC-related ESRD is largely anecdotal, but is streamlined around the mechanism of action of various antirejection strategies.In vitroand animal model studies have shown that mTOR inhibition decreases the production of collagen by dermal fibroblasts, which suggests a possible beneficial role of these medications in the treatment of fibrotic skin disorders, with, however, adverse effects such as greater hypertension, edema and increased creatinine. Therefore, although evidence-based recommendations are still lacking, immunosuppresion with mTOR inhibitors could be an appropriate option for treatment rather than calcineurin inhibitors in patients with SRC who undergo kidney transplantation 8. This was taken into consideration with this patient, and that is why she was switched to mTOR in 2011.
The use of ACE inhibitors has contributed to improving SRC outcomes, probably due to the rapid control of blood pressure and the reduction in renin levels and bradykinin expression, which seems to be specific for ACE inhibitors but not for angiotensin II antagonists. Thus, ACE inhibitors are the treatment of choice in SRC and should be started rapidly and titrated to the maximum possible therapeutic dose. If, despite this, blood pressure is not controlled, other antihypertensive medications such as dihydropyridine calcium channel blockers and diuretics may be added. As third line agents, centrally acting agents such as clonidine and beta blockers may be used 6-9.
Our patient had a hypertensive crisis associated with acute kidney injury with proteinuria, without other causes to explain it, and thus it was considered an SRC. A kidney biopsy was not performed because it was initially contraindicated due to the hypertensive crisis, and kidney function subsequently improved rapidly with treatment. Our case is unusual because the SRC recurred 15 years after transplant, which indicates that SRC can reappear at any time and appropriate clinical consideration is required when assessing renal graft dysfunction in this type of patients.
The patient had the following risk factors for SRC: diffuse cutaneous involvement, cardiopulmonary dysfunction due to moderate pulmonary hypertension, a history of anticalcineurin use and chronic steroid use, which possibly contributed to the recurrence. In particular, our patient's renal function improved rapidly with the introduction of an ACE inhibitor, and her creatinine level has been stable ever since.
Conclusion
Recurrent SRC in a kidney graft is a rare entity and this case indicates that an index of suspicion of recurrent disease is always justified. We propose that risk factors be identified, and optimal management instated, involving early recognition of the disease, diagnosis and rapid treatment with ACE inhibitors, which will affect the survival of the patient and the kidney transplant.











 text in
text in