Introduction
Moyamoya disease is a chronic disease characterized by progressive bilateral stenosis of the terminal portion of the internal carotid artery and its proximal branches with the consequent neoformation of an abnormal collateral arterial network of the arteries which make up the circle of Willis, with variable and nonspecific clinical manifestations 1-3.
This is a rare disease with a very low prevalence in Hispanics, with seizures and stroke symptoms being among the least frequent manifestations in adults 19,21.
The purpose of this article is to present the clinical case of a patient with this disease who arrived in a generalized tonic-clonic seizure preceded by a headache, with subsequent complete neurological recovery, and in whom right basal ganglia hemorrhage and bilateral arterial disease typical of this illness was documented through digital subtraction angiography of the brain 3,5.
Case report
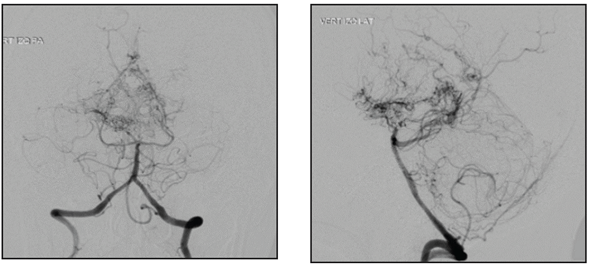
A 45-year-old female, ethnically mestizo patient with no significant past medical history was admitted to the emergency room of a quaternary hospital in the city of Cartagena (Bolívar) on July 1, 2019, due to a one week history of moderately intense holocranial headaches and a subsequent generalized tonic-clonic seizure, with sphincter relaxation and an unspecified length of the seizure. On admission to the emergency room, her blood pressure was 140/90 and the rest of her vital signs were normal with no focal neurological deficits. A simple computerized tomography (CT) of the head showed intraparenchymal hemorrhage in the right basal ganglia, mild multifocal small vessel ischemic disease, malacic changes in the right occipital region and an old left frontal ischemic event adjacent to the left lateral ventricle (Figure 1). The initial lab exams showed no abnormalities, with normal red and white blood cell and platelet counts, and nitrogen compounds, electrolytes and coagulation times all within normal limits. Cerebral panangiography found thinning of the internal carotid and posterior cerebral arteries (the latter seen in 50% of cases) with abnormal neovascularization in the basal nuclei, compatible with moyamoya disease (Figure 2). With these results, her possible treatment plan was assessed by a neurosurgery medical panel, concluding that she could benefit from endovascular treatment. However, in light of the high risk of recurrent bleeding, this procedure was postponed for at least four weeks.

Figure 1 Head CT without contrast. Axial section showing hypodensity of the right basal nuclei, suggestive of bleeding.
Discussion
Moyamoya disease is a chronic illness characterized by progressive bilateral stenosis of the terminal portion of the internal carotid artery and its proximal branches, with the ensuing neoformation of an abnormal collateral network of the arteries which make up the circle of Willis, with an as yet unknown etiology 1-3. The term is derived from the appearance of the collateral arteries which develop progressively throughout the course of the disease and look like "cigar smoke in the air" ("moyamoya" in Japanese) on angiography 2.
The case we present refers to this disease, which must be differentiated from moyamoya syndrome which is linked to unilateral vascular lesions associated with other entities such as neurofibromatosis, sickle cell anemia, Down syndrome, meningitis, trauma, autoimmune diseases, secondary to cranial radiation and Graves' disease 4,6.
This entity tends to be more common in Asian people and less common in Hispanics, as some studies have shown. However, it may affect people of any ethnic background. In Japan, a prevalence of 3.16 per 100,000 inhabitants has been found, while in the United States (US) the disease prevalence has been found to be 0.086 per 100,000 inhabitants. It affects women more than men in a 2:1 ratio, and two incidence peaks have been reported: children between 5-9 years old and adults between 40-50 years old (more common) 7-9. In Colombia, in 2013, only four cases of moyamoya disease had been described, all in children 22; while in 2015, only one case of an adult female patient was reported, with a fatal outcome 23.
The clinical manifestations of this disease vary according to age. Children 5-9 years old with moyamoya disease typically present with arterial ischemic strokes or transient ischemic attacks (TIAs) 11, while geographic variations have been noted in adults from 40-49 years of age, with intracranial bleeds being more frequent in the Asian population compared to the US population 1,10. As has been noted, our patient had the sociodemographic factors of age, mestizo ethnic background, and female sex along with the bleeding process which is characteristic in adults with this disease.
The typical presentation in adults includes seizures; ischemic, hemorrhagic or transient cerebrovascular accidents (with focal signs and symptoms depending on the lesion site); cognitive impairment, personality changes and headache. The individual variations in degree of arterial involvement, progression of the stenosis, ischemic regions of the cortex and response to reduced blood supply help to explain the broad range of clinical presentations.
In our case, moyamoya disease presented as a first generalized seizure with subsequent recovery, without apparent motor or cognitive deficits, caused by an intraparenchymal hemorrhage in the right basal nuclei detected through a simple cranial CT. This finding matches the literature which mentions that intraparenchymal hemorrhage is more common than the intraventricular or subarachnoid forms in patients with this disease, and that the most common locations are the basal nuclei, the medial temporal lobe, and the thalamus 1,4.
The possible causes of bleeding in patients with moyamoya disease include rupture of a fragile collateral vessel and/or an aneurysm caused by the alterations in cerebral flow (high and low-pressure zones formed during the disease). The most common places for these aneurysms to form are the terminal portion of the basilar artery, and the posterior communicating artery. The location of the bleeding in our case suggested a differential diagnosis of a ruptured aneurysm or bleeding from an arteriovenous malformation.
Various tests for assessing cerebral vasculature, such as angiotomography and angioresonance, are used for diagnosis, with good results. However, cerebral panangiography (also known as digital subtraction angiography) is the gold standard for definitive diagnosis of moyamoya disease, when the characteristic arteriographic appearance is seen. It detects stenosis of the terminal portion of the internal carotid artery and its proximal branches, as well as the formation of the network of collaterals 4. In our case, cerebral panangiography was ordered as part of the workup for intracraneal hemorrhage in a young patient, and it showed progressive thinning of both internal carotid arteries, along with neovascularization and bilateral disappearance of the medial and anterior cerebral arteries.
No treatment can stop the progression or reverse the arterial changes produced in patients with moyamoya disease. Treatment is aimed at relieving the symptoms, preventing the recurrence of cerebrovascular accidents and limiting cognitive impairment 12. Medical and surgical measures are available. The recommended medical measures include the use of antiplatelet agents, except in patients with intracranial hemorrhage. Long periods of dehydration and hyperventilation should also be avoided, and patients who present with a migraine should be given medications such as topiramate, and nonsteroidal anti-inflammatory drugs are not recommended 13. The most important surgical measure in these patients is revascularization (direct, indirect or combined), whose general objective is to improve cerebral blood flow 14. Various studies have shown that revascularization in patients with moyamoya disease decreases the rate of recurrence of cerebrovascular accidents (ischemic and hemorrhagic), reduces symptoms (like headache), improves the functional clinical status and even improves cognitive disturbances, with a satisfactory safety profile 15-18. It is therefore recommended by the American Heart Association (AHA) 19. In addition, Liu et al. reported that revascularization therapy has a positive impact on the prevention of rebleeding in patients with a hemorrhagic presentation 20. Revascularization therapy is indicated in our case (endorsed by a medical panel), which was postponed for one month due to the recent intracerebral bleeding.
Moyamoya disease should be suspected in children or adults under the age of 50 with clinical signs of acute ischemic and/or hemorrhagic cerebrovascular disease without risk factors, with or without a history of neurological deficit or focal neurological episodes. It is important to determine the diagnosis quickly, since the evidence shows that therapeutic measures, both medical and surgical, are associated with a better prognosis, with the latter being the treatment of choice and the one which produces the best results. The prognosis for patients with this disease is not completely predictable.











 text in
text in