Introduction
Optimization of a healthcare institution's beds is a process which helps to make good use of the resources, becoming not only an institutional but also a governmental policy 1. Despite this, studies in different countries show that these processes are often not efficient, leading to inappropriate lengths of stay, thus wasting both economic and human resources and exposing patients to unnecessary risks such as infections, falls, thromboses, and increased costs, among others 2,3. Furthermore, with the imbalance between bed supply and demand, if a hospitalized patient has a problem with discharge, he/she does not free up a bed for a patient from another area such as emergency or surgery, among others, thus collapsing these services 4.
In addition, the most noticeable processes affecting the use of beds in an institution are the availability of beds, the timely beginning of treatment and the patients' discharge 5. The latter has become very relevant today; while our country has joined efforts to make the process more efficient, as seen in strategies such as transfers to home care programs, prompt delivery of discharge medications, special programs (diabetes, anticoagulation, oxygen therapy and cancer, among others), daily rounds, audits (real-time audits), and national guidelines 6, we find that the impact is often low, leading to unnecessary stays 7 which may affect more than 30% of inpatients 8,9.
An inappropriate hospital stay may be related to a delayed discharge. This concept, which is summed up as the blocking of a hospital bed, is defined by the National Health Service (NHS) of England as when a patient, from a clinical perspective, can be discharged, but continues to occupy a bed 10, a concept which has also been accepted in Latin American countries 11. Delayed discharge is a high impact problem; it is estimated that it may explain up to 70% of the causes of inappropriate hospital stay 12. It also causes a high loss of resources; reports from countries such as England note that it may cost close to €100 million and consume 1.2 million bed-days per year 13.
Non-clinical delayed discharge generally results from the conditions or needs patients have for discharge. These conditions may vary depending on the country, healthcare system, clinical condition, or age. In Spain, Giraldo et al. 11 described the problem in an internal medicine service, finding the principal cause to be socio-familial difficulties in assuming the patient's care after discharge. Hendy et al. in the United Kingdom 14, after analyzing the possible problems (such as delayed discharge) in the healthcare of 83 patients, explained that 21% of the cohort's hospital stay was due to delayed discharge and most of these cases were due to delays in the provision of social and therapeutic requirements. In Colombia, in 2017, Sánchez HS 15 analyzed 27,324 observations of quality of care deficiencies and described that these deficiencies led to a prolonged stay which generated a cost overrun of US$1,380,817. He also noted that the deficiencies explaining the inappropriate stays were due to problems related to the payer.
In another vein, in Colombia, health conditions and the provision of health care differ greatly from one department to another 16, leading to the need for patient transfers from one department to another or from distant municipalities to centers which offer the services required by the patients. This situation is seen by some entities as an opportunity to offer their more complex services; however, at discharge or when the patient needs to return to his/her place of origin, this is also a challenge to the healthcare system which has to offer appropriate conditions for this transfer. However, clinical personnel often observe that the patient cannot be discharged due to different problems, including administrative problems, which contribute to an inappropriate hospital stay.
The objective of this paper was to describe the proportion of patients with non-clinical delayed discharge, along with their sociodemographic and clinical characteristics, and to estimate the direct costs of nonclinical delayed discharge from June 1 to August 31, 2017, in a tertiary care institution.
Materials and methods
This was a retrospective descriptive study of hospitalized patients who fulfilled the criterion of delayed discharge between June 1, 2017 and August 31 of the same year at the Clínica Somer, which is a tertiary care institution located in Rionegro, Antioquia. This institution has close to 220 beds, with approximately 13,000 discharges per year. The institution provides services to subsidized and contributory medical insurance entities as well as private patients, and it should be noted that there are service agreements with nearby towns but also with other regions of the country.
The operative definition of delayed discharge and the only inclusion criterion was: patients who from a clinical perspective (attending physician) could be discharged due to their health condition, but who continued to occupy a bed due to nonmedical problems 11. To obtain the cases, the hospital census was reviewed daily by the research group and the clinic's auditing physician to find patients who fulfilled this criterion. Subsequently, the medical chart was reviewed to verify that the patient fulfilled the criterion of discharge or discharge order by the attending physician and the patient was followed until the actual discharge. The variables collected were: sex, age, place of origin, type of medical insurance, insurance company, discharge diagnosis, attending service at the time of discharge, total length of hospital stay, days from medical discharge until the patient left the institution, and reason for the delayed discharge.
For costs, the following factors were considered: total cost of the patient's stay, the cost caused by the delayed discharge, and the percentage of this cost compared to the total cost. The analysis was carried out from the payer's perspective; the costs which were considered for the study were: inpatient days (room), medications, oxygen, supplies and medical assessments. Subsequently, the figures were converted to American dollars, using the average market exchange rate at the time of the study (2,951 pesos per American dollar). Since the study's scope was to measure the total direct cost of the problem, the itemized cost was not analyzed.
With regard to the statistical analysis, absolute and relative frequencies expressed as percentages were used for qualitative variables, and the average with standard deviation or median with interquartile range were used for quantitative variables, depending on the distribution. The data were stored and processed in Excel. With regard to ethical considerations, the study was approved by the institution's Research Ethics Committee.
Results
During the three months analyzed, 79 patients with non-clinical delayed discharge were found out of a total of 3,273 discharges, corresponding to 2.4% (Table 1). There was a predominance of women with 59.5% of cases. The median age was 49 years, with a broad range from six months to 93 years. Most patients 62 were covered by subsidized medical insurance; 60.4% came from other departments or distant towns. The total inpatient days were 1,989, with 547 days being contributed by delayed discharge (corresponding to 27.5% of the length of stay), with an average of 6.6 days of delayed discharge per patient.
Table 1 Characteristics of patients with an inappropriate length of stay, n=79.
| Median age in years (range) | 49 (0.5-93) |
| Female patients, number (%) | 47 (59.5) |
| Subsidized insurance coverage, number (%) | 49 (62) |
| Coming from other departments or distant towns, number (%) | 48 (60.7) |
| Total delayed discharge days (range) | 547 (1-25) |
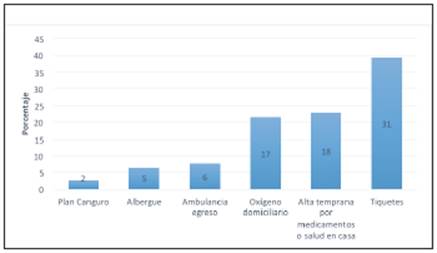
The causes of delayed discharge identified were (Figure 1):
The need for tickets to return to their place of origin (39.5%), mostly corresponding to low-income patients who were unable to cover these expenses.
Early discharge with medications (22.8%) corresponding to treatment not generally included in the insurance's approved list of medications or special programs (anticoagulants, nutrition, supplementary milk, HIV program and TB, among others), without which the patient could not leave the institution.
Need for home oxygen in order to be discharged (21.5%).
Other causes added up to 16.5%: corresponding to requests for ambulance transport for discharge, which was necessary for transporting patients who, due to their critical condition, were unable to travel on public or even private transportation. Guesthouses or temporary shelters indicated as an option for groups of patients from distant locations who needed to finish a treatment, for instance radiation, chemotherapy and the kangaroo plan for preterm newborns.
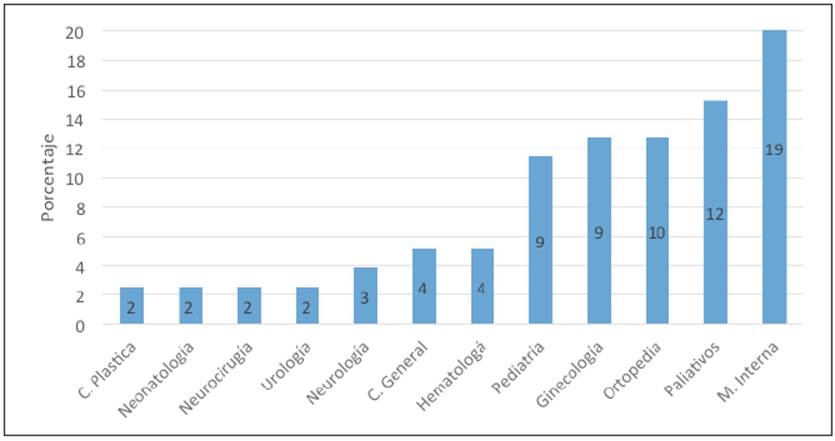
The specialties which were most affected were: internal medicine 24.1%, palliative care 15.2%, orthopedics 12.6% and gynecology 11.3%, although, on the whole, it affected multiple healthcare areas, albeit to a lower degree (Figure 2). It should also be noted that none of the affected patients experienced an adverse event during this period.
The total cost of care for the 79 patients was US$637,050.82, of which US$83,935.66 (13.1%) corresponded to delayed discharge (Table 2). The average cost per day was US$153.44, which includes one day of hospitalization (room), medications, oxygen, supplies and medical assessments. The average per patient was US$1,062.47. The most affected services were: internal medicine US$14,709.55, palliative care US$11,735.93, pediatrics US$11,383.62 and orthopedics US$10,123.07, which contributed 57.1% of the cost. In addition, it should be noted that this amount was undertaken by the payer corporations. Figure 3 details the costs by healthcare service.
Table 2 Distribution of patients by month, total cost and cost due to inappropriate length of stay, in dollars (1 dollar = 2,951 Colombian pesos), 2017
| Month | Patients | Inappropriate length of stay in days | Total billed cost | Cost of inappropriate length of stay (% of the total) |
|---|---|---|---|---|
| June | 21 | 145 | US$102 867.81 | US$22 545.70 (22) |
| July | 29 | 184 | US$260 49.31 | US$31 834.26 (12) |
| August | 29 | 218 | US$273 691.70 | US$29 555.70 (11) |
| Total | 79 | 547 | US$637 050.82 | US$83 935.66 (13.1) |
Discussion
Delayed discharge is a healthcare problem which causes a significant unnecessary use of resources. We can see that in just one clinic, during the three months which were reviewed, there were 79 cases, corresponding to 2.4% of all discharges. A systematic review by Landeiro et al. in 2017 3 showed that these cases may affect anywhere from 1.6% to even more than 38% of all inpatients, depending on the case definition used, population or institution evaluated. Although it is a low percentage, a closer look shows that the total inpatient days lost due to this cause was 547, which is equivalent to the use of almost 18 beds for one month in any healthcare institution. This, in a tertiary care institution where hospital beds are generally a limited resource and with other services collapsed waiting for the beds to be freed up, is a highly significant figure.
In our study, delayed discharge was related to the place of origin and type of healthcare insurance coverage. Almost 60% of the patients had subsidized insurance and were referred from other departments or distant towns such as San Andrés, Chocó, Santander, and western Antioquia, among others, as well as from indigenous communities (data not shown). It is to be expected that this population is the most affected, understanding the geographic and social difficulties of our country, in which the healthcare network for this insurance coverage is more limited 16, with greater barriers to access 17.
The problem affected all areas of hospitalization. The analyzed data show that it covers all ages and all healthcare services in our clinic. Those most affected were internal medicine and palliative care, possibly due to being attending services or unloading services for other specialties, although it has been shown that the internal medicine specialty explains a large portion of the problems of delayed healthcare 15. The average days of delayed discharge per patient was 6.6 days. Other countries like Cuba, Mexico, and the United Kingdom have reported averages ranging from 2.2 to 12.7 days 3,18, depending on the type of institution or affected specialty.
The main reasons for delayed discharge were the need for return tickets, the need for medications for discharge and the need for home oxygen, in 60% of cases. This finding matches what was described by Sánchez et al. 15 who also found inappropriate stay problems related to delays in delivering medications or outpatient services, home oxygen and transportation from the hospital to home. The problem of patients' return to their place of origin was related to a low socioeconomic condition and inefficient procedures, in many cases, by healthcare providers, which is reflected in a significant financial loss. Although transportation home is not included in our obligatory healthcare plan, a large proportion of these patients are low-income and are unable to cover the cost of their tickets. On occasion, the healthcare institutions underwrite the cost, but until the discharge is resolved, the patients continue to use resources. The need for oxygen and essential discharge medications, and the need for an ambulance due to the patient's clinical condition, also reflect the need to strengthen the insurers' services.
Delayed discharge generates a high cost for the system. The cost generated by the cases found was US$83,935.66. The average cost per patient was US$1,062.47. We understand that this figure varies from one institution to another. Institutions in Colombia record payments of up to US$276,180 on this account 15. Data from other countries show that this problem may cost between €2,352 and 9,317 per patient 13,18. In the United States, there are reports of US$1.8 million for a period similar to that of our study 19. This shows that it is a very high figure for the system and depends on the characteristics of the institution. If we multiply this figure times 12 months of health care and times all the institutions in Colombia, the problem is even greater. As we stated previously, the payment of this cost was assumed by the payer corporations.
Study implications
We consider that the information contributed may be useful for healthcare administrators, focusing on the management efficiency and functionality of the services, especially to improve the patient discharge process. It is clear that the rational use of hospital stay and diagnostic aids is a key element in quality management and the ability to impact on the wasting of resources. Several actors should participate in its solution. Healthcare providers should identify early on what factors could result in a timely discharge (even beginning at admission), to act on them. For example, a physician can predict that his/her patient will need home oxygen, special nutrition or a supplementary formula in the case of a newborn, at the time of discharge; the next step would be to begin the paperwork early.
The insurance companies should also institute measures to provide an efficient healthcare network, timely delivery of medications, home hospitalization, or to determine at the time of referral how the patient will return to his/her place of origin, especially with low-income patients. In addition, the territorial authorities should insist on improving access to good quality and high complexity healthcare services to avoid, as much as possible, interdepartmental transfers.
Areas of uncertainty and limitations
The findings of this study, it should be noted, are limited to institutions with similar characteristics. In order to comprehensively understand the implications of delayed discharges, the behavior of the problem on an individual level and at different levels of care must be observed. We also note that the evaluated time was short, due to the exploratory nature of the study, but it would be good to analyze the problem over longer periods of time to avoid period biases and to observe the behavior over time.
The scope of the study did not include measuring costs or losses incurred by the institution nor the costs generated by this stay for the patients, which would also be an area for research.











 text in
text in