Introduction
The global population over the age of 65 is estimated to be 900 million people 1, and this figure is expected to triple by 2030 in a phenomenon known as the “silver-haired tsunami” 2. In Colombia, in 2009, there were an estimated 2.5 million people over the age of 65 and one million older than 75. In addition, life expectancy by 2025 will be approximately 77.6 and 69.8 years for women and men, respectively 3.
This long-lived population, even with healthy lifestyle habits, represents an age group with a greater risk of developing multiple diseases. These include fragility fractures 2, which are caused by low-energy trauma due to mechanical force equivalent to a fall from standing height or less, which would not normally cause a fracture 4.
Fragility fractures may occur in the hips, vertebrae or wrists, and are not only a diagnostic criterion of osteoporosis in the absence of densitometry studies, but also indicate its severity 5-7.
Osteoporosis has an enormous personal and financial cost 6,7, as it accounts for almost two million fractures per year 8. In Europe, disability due to osteoporosis is greater than that caused by cancer (with the exception of lung cancer) and is comparable to a wide variety of chronic noncommunicable diseases such as rheumatoid arthritis, asthma and arterial hypertension 7. In the United States, osteoporosis-related morbidity and mortality cost approximately 17.9 billion in 2005 and involved about 432,000 hospital admissions, 180,000 admissions to geriatric homes and 2.5 million visits to general medicine. In addition, the chronic pain associated with osteoporosis is related to disability and quality of life sequelae 9.
To avoid the complications caused by osteoporosis with regard to fractures, the at-risk population must be identified and diagnostic studies performed, with therapeutic strategies established for those who warrant them 10. Interventions have been described that reduce the general population’s risk and may be used both for primary and secondary prevention. These strategies include exercise, moderate alcohol consumption, pharmacological treatment, fall prevention and avoiding smoking 9.
With regard to pharmacotherapy, in our country, there are various medications covered by health insurance which may lower the risk of fractures by anywhere from 20.7 to 70% 9,11.
Despite the foregoing, the vast majority of patients continue to be undiagnosed and consequently lack treatment 12. Therefore, in addition to characterizing patients with fragility fractures, the study also intended to determine who met the screening criteria for this disease, according to the osteoporosis treatment guidelines, in order to determine if those at risk for, or diagnosed with, osteoporosis are actually being appropriately addressed and treated.
Materials and methods
A prospective study was performed on patients admitted to the Orthopedics and Trauma Service of the Hospital Universitario San Jorge de Pereira (HUSJ) from March 1 to September 1, 2018. Patients of both sexes were included, who were over the age of 18, were diagnosed with a fragility fracture, and signed the informed consent. Eleven patients from whom variables of interest were unable to be obtained were excluded.
The group of patients selected for the study were characterized according to the following variables:
Sociodemographic: age, sex and type of health insurance.
Clinical: body mass index (BMI), comorbidities (diabetes mellitus, chronic obstructive pulmonary disease, active cancer, hyperthyroidism, hypogonadism, adult osteogenesis imperfecta, chronic malnutrition, chronic malabsorption, chronic liver disease, dementia, rheumatoid arthritis), anatomical location of the fracture, type of fracture, previous fractures, prolonged corticosteroid use (> 3 months), age at menopause, smoking, alcohol consumption (>3 drinks/day), family history of osteoporosis or fragility fractures, regular follow up by a general practitioner or specialist, diagnosis of osteoporosis, bone densitometry (DEXA) and result, treatment employed and knowledge of fall prevention.
Temporal: time elapsed from the fracture to admission to the hospital, time elapsed from hospital admission to surgery, length of inpatient stay and vital status at discharge.
In addition, screening criteria for osteoporosis were applied to the patients according to the guidelines with the highest impact in the literature, such as the United States Preventive Services Task Force (USPSTF), International Society for Clinical Densitometry (ISCD), National Osteoporosis Foundation (NOF), American Association of Clinical Endocrinologists (AACE), American Academy of Family Physicians (AAFP) and Canadian Osteoporosis Society (COS); and the risk of fragility fractures was estimated using the bone fragility fracture risk calculator (FRAX®). With this calculator, each country›s risk of osteoporotic fractures in patients between 40 and 90 years old within the next ten years can be calculated, and the next steps can be determined according to the results (not treat, send for densitometry, or treat).
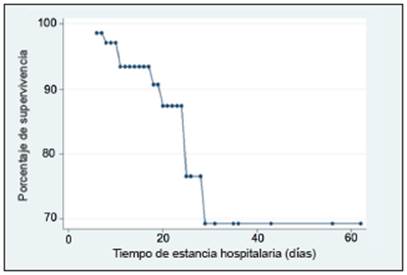
The information from HUSJ de Pereira›s medical records was used to collect the data, in addition to an interview with each patient and/or his/her family. The data were recorded in a previously designed Excel database, and the STATA version 15.1 statistical package for Windows was used for analysis. A Kaplan-Meier analysis was used to estimate the inpatient survival probability of patients with fragility fractures.
This study was approved by the bioethics committee of HUSJ de Pereira as a «no risk research study», according to Colombia´s Ministry of Health Resolution No. 8430 of 1993. The ethical principles of autonomy beneficence, nonmaleficence and information confidentiality established by the Declaration of Helsinki were adhered to.
Results
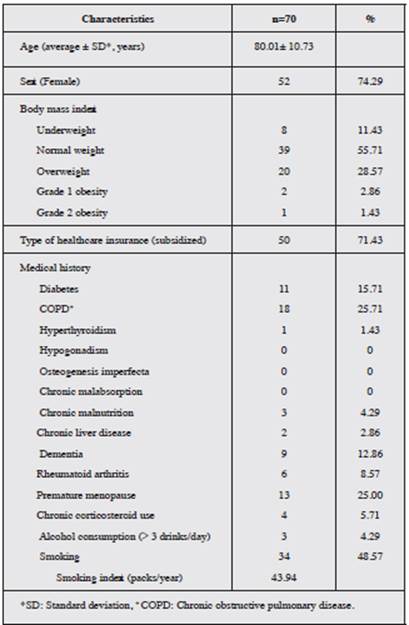
The 70 patients included reported an average age of 80.01 ± 10.73 years. Altogether, 74.29% of the study subjects were women. A total of 11.43% of the patients had a low BMI. The prevalence of reported comorbidities was as follows: COPD (25.71%), diabetes mellitus (15.71%), dementia (12.86%) and rheumatoid arthritis (8.57%). In addition, 25.0% of the women were found to have had early menopause. With regard to pharmacological and toxicological history, 5.71% of patients had a chronic intake of corticosteroids, 48.57% had a history of smoking, with an average smoking index of 43.94 packs/year, and the frequency of alcohol consumption was 4.29% (Table 1).
Fragility fractures presented in the hip in 98.57% and in a vertebra in 1.43%. Of the hip fractures, extracapsular ones were the most common at 68.57%, with the trochanteric subtype representing 60.0%. The left hip was the most affected with a frequency of 52.17%. A total of 22.86% of the patients had had previous fractures, and 5.72% had had two or more prior events. Patients who underwent surgical treatment made up 85.71% of the sample, while 14.29% received nonsurgical treatment. With regard to the temporal variables, the time elapsed from hospital admission to surgery was 11.48 ± 6.06 days, and the length of hospital stay was 18.11 ± 10.84 days. Out of the cohort, 12.86% of the patients died during hospitalization (Table 2).
The Kaplan-Meier analysis reported a probability of survival close to 70% for stays of 30 days or more, while, if a patient was able to be discharged at 15 days, survival was 94% (Figure 1). Of all the deaths, 22% were due to sepsis, 33% to pulmonary thromboembolism, 11% to active cancer and in 33% of the cases the exact cause of death was not able to be determined.
Altogether, 81.43% of patients reported having been seen by a physician in the year prior to the fracture; 64.91% of these patients had been seen by general medicine, while 33.33% had been seen by general and specialized medicine, and only 1.75% had been seen by a specialized physician. Fifty percent of the patients reported having been educated by their physicians regarding fall prevention (Table 3).
In regard to indications for osteoporosis screening through bone densitometry, of the total number of patients, 65.71%, 95.71%, 97.14%, 74.29%, 65.71% and 90.0% were found to meet the criteria according to the USPSTF, ISCD, NOF, AACE, AAFP and COS guidelines, respectively (Figure 2). Despite this, only eight patients (11.43%) had undergone this study.
Figure 2 Number of patients with an indication for osteoporosis screening according to the various guidelines.
Of the total population, nine patients had a prior diagnosis of osteoporosis. Of these, four had a densitometry diagnosis, four had both a clinical diagnosis by fracture as well as a densitometry diagnosis, one was diagnosed without clinical signs or DEXA, and none had a clinical diagnosis by fracture, despite 12 patients having a fracture history. Of the nine patients previously diagnosed with osteoporosis, only five had been receiving pharmacological treatment. Of these, three patients received ibandronate, one received alendronate and one received strontium ranelate.
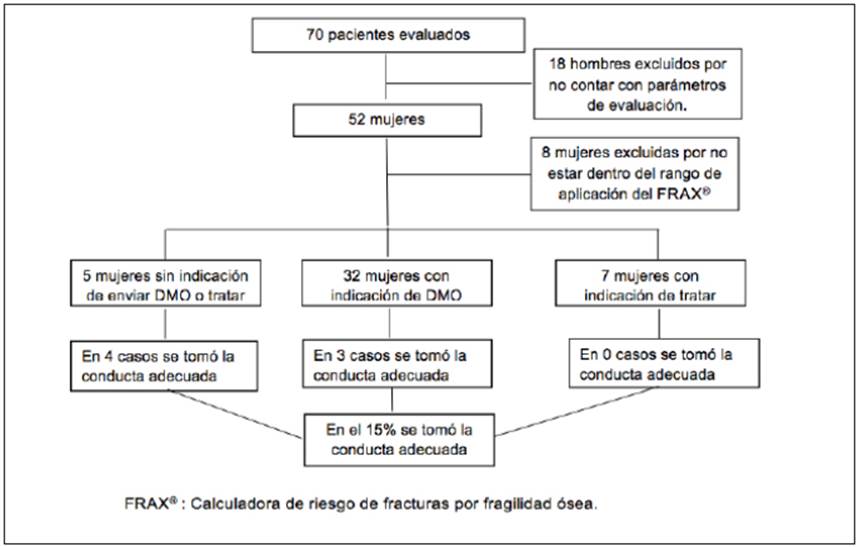
Finally, using the FRAX® tool exclusively applicable to postmenopausal women and validated in our country, it was determined that of the 52 women included in the study, five patients had no indication for treatment, 32 had an indication for DEXA, seven had an indication for treatment, and the FRAX® tool could not be applied to eight patients because they did not fall within the proper age range (Figure 3).
Discussion
This study determined that the average age of the population with hip fractures was 80 years and the female sex was the most affected, which is consistent with the reports in the global and local literature 12,13. The location of the hip fracture which most affected the study population was extracapsular, which was to be expected, since these fractures are the ones which most affect the long-lived population 13.
Surgical treatment was found to have been performed on 85.71% of the patients, an intervention which, according to the literature, has proven to have a lower mortality rate, better clinical outcome, less functional dependency and a shorter hospital stay compared with nonsurgical treatment, although the latter may be necessary in patients who have weakness, instability and terminal diseases 14,15.
Global guidelines recommend early surgery, within the first 24 to 48 hours, as this results in fewer related complications (pulmonary thromboembolism, pneumonia, pressure ulcers and delirium) and a lower mortality rate 16,17. Studies in the United States and Spain show a median wait of 1.8 and three days, respectively 18,19, while in our study, the patients had to wait approximately 10 days for surgery, which is concerning due to the associated adverse outcomes. The average hospital stay was 18.11 days, compared to other studies in which the stay does not exceed 8.1 days 19. With regard to survival, the studies are not conclusive, and most establish it at 30 days after discharge 19,20. In our study, post-discharge assessment was not performed, which is a limitation in terms of real survival. However, it was observed that the longer the hospital stay, the lower the inpatient survival, reaching 69% at 30 days. In addition, 55% of the deaths in this study were due to sepsis and pulmonary thromboembolism, which are related to the fracture itself or to extended hospital stay.
Considering the importance of osteoporosis in the development of fragility fractures, the authors decided to include the main risk factors for acquiring this disease, based on the FRAX® tool 21,22. Smoking, COPD, previous fractures and diabetes mellitus were found to be the main related precedents, which is consistent with the reports described in the literature 23.
Currently, there are multiple guidelines for osteoporosis screening using DEXA 24-29. In our population, at least 65% of the patients met the criteria for screening and only 11.4% had received it. With regard to the application of the FRAX® tool and its consequent recommendations, in only 15% of cases was the appropriate conduct adopted. This is a wake-up call regarding the shortfalls in prevention which we are experiencing in our setting, especially when 81.43% of the study patients were regularly seen by a physician during the previous year. This situation is alarming, since screening leading to early diagnosis and prompt treatment may lead to up to 41% reduction in the risk for, and recurrence of, osteoporotic fractures, thus enabling a decrease in morbidity and mortality and their associated costs 11,22,30. This analysis could not be performed on the males as there are no currently available assessment parameters for the Colombian population 11, a situation which places this population group at somewhat of an assessment disadvantage, despite being a minority.
Finally, concerning the treatment employed in patients with a diagnosis of osteoporosis, ibandronate was found to be the most frequently prescribed medication with 33.34%, followed by alendronate and strontium ranelate with 11.11% each. It is remarkable that ibandronate was the preferred medication in this population with a predominance of hip fractures, since this medication has not been shown to prevent these fractures, as opposed to alendronate and zoledronic acid, which are considered to be first choice medications, having shown evidence of reducing both hip and vertebral fractures 6.
Conclusion
As our population ages, it increases its risk of fragility fractures. This is a frequent problem in our setting which leads to multiple complications including death. Despite this, the treatment and intervention times are slow once the fractures are diagnosed, and both primary and secondary prevention efforts are insufficient due to the lack of timely identification of the at-risk population.











 text in
text in