The outbreak of the novel SARS-CoV beta-coronavirus has been - as of June 21, 2020 - confirmed in 182 countries and multiple territorial zones, affecting approximately 8,708,008 people worldwide, of whom 5.3% have died 1. The emergency situation caused by this outbreak has become, without a doubt, the greatest difficulty faced by humans in the twenty-first century, and has broken into all aspects of daily life, with immeasurable sociocultural, political and economic consequences, and, of course, hav ing a direct impact on the health of the patients who develop moderate to severe forms of the disease. However, it has also had an indirect impact on other population groups affected collaterally by the pandemic, such as healthcare staff, who have been affected by contagion during patient care in hospitals, but have also been victims of acts of discrimination, threats and physical and psychological attacks in and out of the hospitals.
Regarding the lives at risk within the hospitals
Today, healthcare professionals are the most valuable resource each country has for combatting the disease, and it should be a universal principle that they receive the bio safety equipment needed to reduce the risk of contagion during the care of patients infected with coronavirus 2. This is especially important considering that, while the main strategy worldwide has been to instruct the population to remain at home, healthcare personnel prepared to do the opposite; that is, to travel to the healthcare institutions to provide care for patients carrying a virus with a very high ability to spread 3.
The international press reported the case of the infec tion - and subsequent death - of Dr. Chaolin Huang, one of the first to report the signs found in patients with coro navirus disease (later named “COVID-19”). The infection of Dr. Wenliang Li was also described, who warned of the outbreak emergency and was subsequently reprimanded by the local police; as well as that of Dr. Zhiming Liu, the president of Wuchang Hospital in Wuhang, Hubei Prov ince, the region where the outbreak is presumed to have originated 4,5. Since then, it has been confirmed that, as a result of exposure to the virus, the rate of nosocomial infections has been high and linked to the act of health care.
In China, at least 3,300 healthcare workers have been affected 3. In Italy, almost 5,000 healthcare workers infected, and in Spain, more than 3,000 workers. In Co lombia 6, the last report from the Instituto Nacional de Salud (INS) [National Health Institute] shows that there are at least 1,547 professionals affected with the disease, corresponding to 2.4% of all confirmed cases in the country. Of those affected, 32% are nurse aides, 19% are physicians and 12.9% are professional nurses. Interestingly, 88% of the confirmed cases are symptomatic, which could indicate a large number of underreported asymptomatic or untested individuals. To date, three hospitals have had to be closed due to massive transmission to healthcare and administra tive staff in these institutions 7-9.
Furthermore, in Cuba, a healthcare staff infection rate of 7.7% had been recorded up to the end of April, according to the Ministry of Health report, with 92 healthcare workers infected, including 47 physicians. Of the 300 healthcare workers confirmed to have COVID-19 up to June, none were reported to have died. Likewise, in Panama, 440 cases had been counted in healthcare personnel at the beginning of June, and the Health Minister of this country stated in an interview that 17.5% of the Ministry of Health physicians had acquired the disease.
Peru, as of June 26, 2020, occupied the sixth position worldwide for COVID-19 cases, with 268,602 infected, 8,761 deaths and 156,074 recovered.
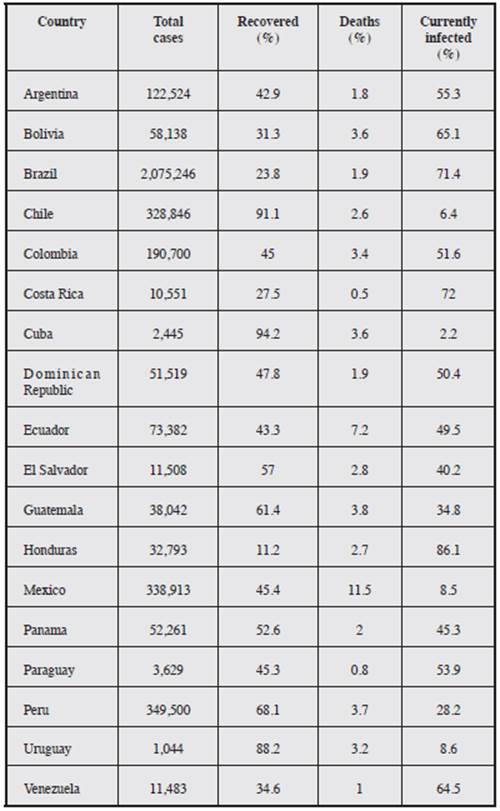
Peru is only surpassed in Latin America by Brazil, which is in second place worldwide with 1,233,147 infected, 55,054 deaths and 673,729 recovered. Table 1 shows the Latin American figures up to July 18, 2020.
The Colegio Médico del Perú [Medical College of Peru], as of June 26, 2020, reported 1,850 physicians infected, of whom 46 were in intensive care and 12 were very seriously ill. To date, 65 physicians have died in Peru 19.
In Argentina, according to National Ministry of Health data, the total cumulative confirmed cases of COVID-19 in healthcare workers up to July 13, 2020 was 7,979 (with no history of travel) and represented 7.73% of all confirmed cases in the country. Altogether, 39.6% of the cumulative cases had at least one risk factor. The cumulative number of healthcare worker deaths is 26 cases and represents 1.37% of all deaths from COVID-19. The lethality in healthcare workers is 0.33%.
At a healthcare institution level, three major factors have influenced the predisposition of healthcare workers to contract the disease.
First, that the emergency room staff was not trained on a novel virus, with which there was no experience and which has many aspects which have been discovered throughout the course of the epidemic. This has led to frequent changes in care protocols, predisposing to errors and confusion. Al ready in 2018, an American study showed that emergency healthcare professionals often lack specialized knowledge for dealing with infectious disease threats 11.
Second, that the disease may manifest with mild symp toms, atypical symptoms, or even behave asymptomatically, and thus healthcare staff may have been exposed to infected patients who appeared healthy or consulted for other rea sons, creating a false sense of security. In addition, in Latin America, the outpatient and emergency waiting rooms tend to be constantly crowded and have considerable waiting times, which contributes to the spread of the disease. Worse still, the coronavirus infection coincided with the epidemiological peak of dengue and yellow fever, as well as with other con tagious diseases which are prevalent in our setting like HIV and tuberculosis, making it hard to concentrate resources and jeopardizing the possibility of implementing the necessary contingency plans to comply with biosafety protocols 12,13.
Third, that the high transmissibility of the virus requires the use of biosafety equipment which is costly, uncomfort able and must be disposed of after use. The fact that it is costly means that countries with limited resources will have trouble acquiring it. Its being uncomfortable means that there will be increased physical wear and tear on healthcare staff, and it requires time for correct placement, which may delay care processes or procedures. The fact that it must be re moved and disposed of after use indicates that multiple suits will be required for patient care, and, therefore, healthcare institutions will get as much use out of them as possible, even requiring that they be reused, or that elements be recycled which, for safety, should be thrown away. In fact, it has been reported that, in some centers, as the epidemic advanced, the quality of the materials of the biosafety elements was noted to decrease.
Finally, it should be remembered that all of the above does not only apply to the personal protective equipment for physicians, but also for nurses and nurse aides, for respiratory therapists, for x-ray and laboratory technicians, paramedical staff, cleaning staff, food staff, and also includes transportation and sample handling staff, all of whom need protective equipment.
As the pandemic advances, it is expected that there will be a progressive shortage of biosafety equipment, followed by a competitive commercial war to acquire and ensure the availability of medical devices, which will put countries with fewer resources at a disadvantage.
If the protection tools are not available, healthcare staff may decide to limit or avoid patient care to avoid exposure and contamination without the necessary protection. Under this principle, social networks and television news programs have reported healthcare staff resignations (physicians, nurses, respiratory therapists), who have ceased activities upon not receiving biosafety equipment from their healthcare centers 14,15. Unfortunately, it was also reported that, in some institutions, the healthcare professionals who led the requests for guaranteed safety equipment or who requested to be tested after exposure to patients with the disease were fired from their workplaces 16.
The importance of supplying personal protective equip ment appropriate for the healthcare staff has been expressed vehemently through statements by individuals, scientific societies and health sector groups 17. Under the social security structure in Colombia, a debate was raised regard ing whose responsibility it was to supply the healthcare team; whether it was the responsibility of the healthcare institutions (e.g. hospitals or hospital centers), or if the re sponsibility belonged to the occupational risk insurers. The lack of legislation and governmental supervision, who did not take on the supply function either, led to these parties failing to fulfill the required supply, and legal gaps were created in the process. In many cases, healthcare staff had to resort to their own resources or third-party donations to acquire disposable equipment.
In Ecuador, the Medical Federation reported the serious lack of equipment as well as the expiration of others. For example, tomography machines which have been function ing for more than 10 years and have reached the end of their useful lives, and are no longer a diagnostic aid. In addition, it reported cases of stock-outs of essential medicines for sur geries and intensive care, lack of basic supplies, poor quality of N95 masks, and lack of clothing and protection for all the healthcare staff in the country´s hospitals; and that, due to this problem, many healthcare workers had been infected 18.
Regarding psychological attacks
The panic situation caused by fear of contracting or transmitting the disease, as first responders on the frontlines of the pandemic, has been amplified by various factors. On one hand, it has to do with lack of knowledge regarding a new viral disease with erratic behavior, and for which there are no proven treatment strategies to date. Besides that, it has to do with the uncertainty caused by the indefinite clo sure of businesses and the actual duration of the quarantine measures. Finally, the constant bombardment with scenes of distress through the media and social networks, in some cases disseminating inaccurate information, has had a nega tive impact on already frustrated and exhausted healthcare staff. This uncertainty is also reflected in the healthcare staff who work in the emergency room, due to the psychological impact caused by:
The workload required to care for critical COVID-19 patients who frequently develop sudden respiratory failure and thus need frequent reassessments and con stant monitoring under heavy protective equipment and meticulous biosafety protocols, which quickly wears out the staff.
The possibility of contracting the infection and/or trans mitting it to loved ones, especially in places with incon sistent availability of the protective equipment necessary to provide care. And, in turn, with the worry of healthcare staff who are responsible for other people (e.g. mothers who are heads of households, only children), regarding who will take responsibility for their loved ones in the event they should succumb to the disease 19.
The financial burden that would result from periods of inactivity due to having to step down in the event of contracting the disease - or due to preventive quarantines after exposure to the virus - which in some countries, such as Colombia, were not duly clarified in the legal framework, leaving healthcare professionals without legal support and health and occupational risk insurers without the obligation to pay for sick leave. Although it should be clarified that in other, more fortunate coun tries, like Costa Rica, the Ministry of Health regulated the administration of paid sick leave while professionals complied with isolation.
The high burden of deceased patients, especially in epi center zones such as Bergamo, Madrid and New York, where healthcare centers were rapidly oversaturated, causing feelings of anguish due to the magnitude of the situation, or a high emotional impact at having to make very important ethical decisions about human lives under extreme conditions. This includes the burden derived from the responsibility of providing medical care to very complicated patients, with incomplete, insufficient or inadequate resources 2. Finally, it includes the mourn ing and impact on the morale of healthcare teams caring for colleagues, friends, professors or teachers who are infected or die from the disease 21.
It is important to note that although the healthcare staff, especially in the emergency room, is oriented to face high risk situations with fortitude, they usually do not receive mental health training strategies from their hospitals. Even experienced members of the healthcare staff, with regular experience in the task of imparting bad news, may have been overwhelmed by the prospect of having to report deaths day after day during pandemic peaks, especially if this was accompanied by feelings of helplessness or guilt. In Italy, at least two suicide cases were reported in nurses, and this may occur in other places 22. Measures must be taken to encourage counseling for healthcare staff in this demanding situation, especially if they show signs of burnout, anxiety or depression, in order to minimize the risk of developing psychiatric illness. In China, for example, some specific measures were taken to alleviate the described difficulties. The healthcare institutions resorted to guaranteeing break rooms where the medical team could rest, providing food and daily life items, supplying relaxation tools, providing more security for dealing with uncooperative patients, and ensuring protective and biosafety equipment, which perhaps represents the greatest concern of the working staff and their families at home 23. Likewise, other institutions, including WHO, have published guidelines and recom mendations with strategies for protecting the professionals’ mental health 24.
Preliminary results presented by the research group on Women’s Health of the Universidad de Cartagena (Co lombia) on “occupational stress and fear of COVID-19 in general practitioners” reported that, out of 531 physicians surveyed, 84% reported experiencing fear regarding CO VID-19. Seventy-five percent of those surveyed reported feeling uncomfortable when thinking about the pandemic, 68% felt nervous when reading or hearing news related to the disease, 55% felt palpitations when thinking of the virus, and 54% could not sleep for the same reasons. Thirty-eight percent of those surveyed reported having thought they had symptoms similar to those caused by the virus. In addition, the study found that female physicians reported three times more anxiety than the males surveyed 25,26.
To conclude, the psychological pressure that the authori ties may have exerted to keep physicians or healthcare staff from expressing their concerns to the community, upon pain of disciplinary sanctions or losing their employment, should be highlighted. In Venezuela, cases of physicians and nurses being punished by government agencies for denouncing the hospital crises have been reported (Annex 1).
Regarding discrimination against healthcare staff
Strikingly, another facet of this psychological attack dur ing the pandemic has been seen in a kind of discrimination, evidenced by the refusal of members of the general popu lation to have contact with healthcare staff outside of the hospital, suspecting that these healthcare workers will spread the virus to them. This discrimination gradually changed to more direct attacks like forbidding healthcare staff to enter supermarkets and stores, keeping them from using eleva tors or common areas in buildings, and asking healthcare professionals to leave their apartments. In Bogotá, a case was reported of a healthcare professional who received graffiti death threats against his wife and children if he did not give up his apartment 27. In cities like New York, the psychological bombardment aimed at presenting healthcare staff as potential transmitters of the virus forced physicians and nurses themselves to decide to sleep in their vehicles and not return to their homes. This attitude of persecution and discrimination contrasts sharply with the applause and ovations offered by the community for a few minutes as a sign of support for healthcare workers.
Another form of discrimination was seen in the refusal of public transportation to take medical or nursing staff dressed in scrubs to the hospitals. Although the healthcare staff quickly clarified that once at the hospitals they changed their street clothes for hospital clothes, the community maintained its refusal, which forced authorities in some cit ies to provide transport vehicles or exclusive transportation routes to ensure the mobility of healthcare workers 28-29. The healthcare institutions, in turn, asked their staff not to travel wearing this type of clothing, to avoid confrontations. However, this often led to healthcare professionals out of uniform being fined by the authorities who believed they were breaking the mandatory quarantine.
In Argentina, the number of queries at the Instituto Na cional Contra la Discriminación, la Xenofobia y el Racismo [National Institute against Discrimination, Xenophobia and Racism] (INADI) increased considerably between March and May 2020. Out of 718 queries, 208 refer specifically to situations related to COVID-19, including cases of dis crimination against patients, attacks against and mistreat ment of exposed individuals, and stigmatizing declarations against various groups such as the Chinese community and migrants from several countries, among others. On average, four of every 10 queries were related to the pandemic and/ or isolation, while one out of every 10 had to do specifically with discrimination due to COVID-19. The discrimination situations occurred predominantly in women (57%) rather than men (41%). The neighborhood and dwellings were the most frequently reported setting (71) in the 208 queries denouncing COVID-19 related discrimination, followed by social networks, where many discriminatory, derogatory and violent comments are posted, often fed by the diffusion of “fake news” which not only misinforms, but also creates fear, anxiety and opinions based on information and events which are not very truthful. The work and public administration environments had 20 and 17 queries, respectively, while 13 of these 208 referred to healthcare providers and centers.
In Colombia, President Iván Duque has condemned the acts of discrimination and attacks on medical staff, and the Public Defender has opened anonymous hotlines for report ing acts, threats or harassment to which they may be sub jected 30. The Colombian Penal Code (Article 134 A-C) states that people who commit discriminatory acts may be punished with prison sentences ranging from 12-36 months and fines of 10-15 legal current minimum monthly wages, with the risk of increasing the penalty by one third to one half when the conduct takes place in a public area, public establishment, or site which is open to the public. Even so - criminalized by law - at least 20 cases of aggression in various Colombian cities were found in the national press, of which at least eight were attacks against women (nurses, nurse aides, a social worker, a hospital care technologist) and practically all of them were discrimination situations, especially in dwellings and supermarkets. Three physicians have received death threats, and yet, to date, nobody has been penalized for these acts.
A compilation of the information published in the Latin American press shows that cases of discrimination or violence against healthcare staff have occurred in many countries besides Colombia, with at least 111 cases recorded, distributed as follows: Mexico: 40, Colombia: 20, Argentina: 10, Venezuela; 9, Paraguay: 8, Honduras: 4, Panama: 4, Peru: 2, Costa Rica: 1 and El Salvador: 1 (Annex 1). Forty-five per cent of the cases of discrimination or violence have been against women, while 28% have been against men. Forty percent of the cases of discrimination or violence are against physicians, 40% against nurses and nurse aides 31 and 11% against various members of the healthcare team simultaneously.
Twenty-seven per cent of the cases occur in healthcare centers and another 25% have occurred in the victims’ dwell ings or buildings; 19% of the cases have occurred in public areas, 12% on public transportation, 5% have happened in commercial establishments such as restaurants, super markets and banks, and 4% of the cases have been through social networks, although cyberbullying and defamatory messages sent by these means may be much more frequent but hardly ever reported.
With regard to the main forms of violence, we find that 31% of the news items identified correspond to various forms of discrimination. In 21% of the cases, the violence was physical aggression, and in 7% of the cases it was verbal, with 13% of the cases being mixed aggressions. In 9% of the cases there was police abuse or persecution of healthcare staff. In 11% of the cases there were threats to the healthcare staff.
Most cases of discrimination and attacks against health care staff seem to occur in Mexico, where the current pandemic has seen an increase in violence. People who want to burn a hospital, who throw hot coffee or chlorine at physicians and nurses. We should recognize that the vio lence against healthcare professionals did not begin with the pandemic, it was simply amplified, made more visible, more crude and ruthless. According to Mexican civil law, a certain type of responsibility arises from illegal acts. Article 1910 of the Federal District Civil Code establishes that who ever causes damage in the course of committing an illegal act or an act against public decency is obligated to repair the damage caused. Therefore, if a member of the medical community is harmed, the person who caused the harm would be criminally and civilly liable for repairing it. The harm caused may be to property, that is, having to do with financial loss, or may also be non-property damage, which mainly comprises moral damages. We should work hard to improve healthcare professionals’ legal protection, but we must recognize that our main responsibility is to generate the will in the authorities to enforce the law. A document is needed to forcefully encompass the medical community and healthcare staff’s feelings regarding the social reality of the context, the crushing anarchy created by impunity, the lack of legal actions, and the arguments that need to be pushed in all the congresses and local chambers, so that laws will be drafted and enforced in an exemplary manner as soon as possible, before calamity goes from being an anecdote to being part of everyday life; this is imperative.
In Bolivia, a survey on attacks on healthcare workers found that, of 184 responses, 77.2% responded affirmatively to having suffered some form of aggression, especially women. Most attacks occur against physicians (72%), in healthcare centers and leaving work/on the way to work. The main types of aggression reported by those surveyed were verbal aggression, followed by discrimination, physical violence and death threats. In 8.3% of these aggressions, the police had to intervene, but only in 42% was there a police report. Ninety-four percent of those surveyed knew of other healthcare workers who had been affected.
In Paraguay, there have been statements issued by SPMI and the Sindicato de Médicos de Guairá [Guairá Physician’s Union] (SIMEG) warning of the concern regarding the me dia’s reporting 32,33 the identity of colleagues affected by COVID and regarding the abuse suffered by one physician at the hands of the police force.
In contrast, and fortunately, we found that other coun tries such as Cuba, Guatemala, the Dominican Republic and Uruguay have not reported major cases of attacks or discrimination against healthcare workers.
Regarding physical attacks
Even before the outbreak, the constant limitations of healthcare systems had created a sense of frustration and discontent in the community, which has adopted defiant and unkind attitudes towards healthcare workers. In turn, healthcare workers also reached this epidemic frustrated by the limitations of the healthcare systems, with high burnout rates, and feelings of helplessness in the face of demanding schedules, delayed payment, employment instability and informality, and lack of legal guarantees and social benefits 28,34. All of this predisposes to a state of extreme tension which fosters mistreatment and complicates communication channels during patient care. Cases of physical confronta tion have been reported, especially by patient companions or relatives, with improper treatment of healthcare staff. A meta-analysis in China showed that workplace violence against healthcare staff reached levels as high as 62% 5.
Patients’ relatives or companions frequently direct their feelings of frustration and guilt toward the healthcare team members, and the strict isolation requirements due to the pandemic have increased complaints against and lack of confidence in the hospitals. In other places, frustration is also a product of the need to separate patients from their relatives, who are left with the dilemma of not being able to see their loved ones again until they have recovered, or, unfortunately, until they have died, in which case the funeral arrangements will likewise be limited. In Colombia, there were frequent conflicts with relatives of deceased patients who, on being informed of the measures for the disposition of the bodies, refused to accept the notification protocol and the international recommendation of cremation. This behavior went so far as to lead the general population to doubt the medical reports, influenced by sensationalist media from which arose the false belief that the classification of patients without the disease as COVID-19 cases was provid ing personal or financial benefits to healthcare workers or healthcare centers, when, on the contrary, the costs of care, imaging and purchase of protective equipment have gener ated cost overruns and large losses for healthcare institutions.
Indeed, the most recent criminal acts have been attacks by family members against the physical plants of healthcare centers on being notified of the death of a relative. Despite the medical team having expressed its total willingness to face this battle, with no responsibility for the appearance of the outbreak, patients’ relatives continue to see them as being responsible for the fatal cases, which has led to death threats or lawsuits alleging medical errors or malpractice, generating derogatory comments which can affect the pro fessionals’ reputation and tear down their efforts and spirit. In the worst cases, the resentment of those who blame the healthcare team for the death of their relatives has reached the point of considering the hospital’s work as blatant murder of their relatives; clearly an attitude of flourishing terror in limited and misguided minds, lacking clarity but with an undefined and frightening danger of the tangential risk of intra or extramural aggression.
Other aggressive attitudes are related to the inappropriate behavior of the patients themselves who, despite being aware of the need for confinement to avoid infecting other people, refuse to cooperate with the hospital’s measures and directly confront the attending staff, putting their physical integrity at risk. In addition, cases have been reported of healthcare professionals or administrative staff who, on their way to the healthcare centers, have been heckled or intercepted by individuals who have physically and verbally assaulted them 34-37. The WHO regretted the death of one of its workers in Myanmar who was attacked while transporting coronavirus samples in a vehicle 38.
Regarding policies for staff in training
Healthcare systems worldwide will probably operate at maximum capacity for many months. However, unlike the mechanical ventilators, which may be manufactured or purchased, healthcare staff cannot be purchased or work at maximum capacity for long periods of time 3. In addition, the possibility that the active healthcare team may be infected, require hospitalization, require sick leave or, in the worst case, die, has led to healthcare services becoming progressively short-staffed.
The response to this situation has been to recruit staff who do not usually work in the emergency rooms (sub-specialists, residents in other fields) and to carry out improvised gradu ations of final year students in healthcare fields 39 to deal as common soldiers with the care of complicated patients according to care protocols which often change very rapidly, based on the scant available evidence. This desperate mea sure may make sense in places with a complete collapse of the healthcare system, but in settings that have not reached a critical point it means enlisting untrained staff in a situation with a high risk of contagion and with frequent complaints of lack of protective equipment. Some institutions have redesigned their academic training programs, orienting the students to “non-COVID” services or the performance of activities which do not involve direct patient care contact, such as call center management or telephone follow up of patients who are referred to home observation due to their mild symptoms. In other institutions, the teaching alliances have withdrawn their students indefinitely, and now have them cover portions of the curriculum through virtual meetings or carry out research activities, with the impact of this modality on the quality of professional education still unknown.
In Colombia, there are at least nine confirmed cases of healthcare staff students who have been affected by the dis ease 6. It is essential that the continuity of clinical practice or rotations go hand in hand with careful coordination and with the absolute guarantee of biosafety measures which, as professionals in training, they deserve.
Final reflection and request
Based on the foregoing, there is a need in all our continent to continue strengthening awareness raising tasks in order to prevent and eradicate the cases of discrimination, stigmatiza tion and/or violence which occurred during the study period, many of which had the distinction of referring to situations specific to the exceptional context which the pandemic has presented. In effect, we are presented with a new setting, with multiple challenges, in which pre-existing situations worsen and new ones appear, tied to the historical moment the world is experiencing, which forces us to think of new approaches and strategies to reach the greatest number of people possible.
For these reasons, we, clinical specialists from all Latin American countries, call for guarantees in this relentless fight which is about to begin in its fiercest form, through the following requests and recommendations, extended also to human rights organizations, government organizations, the International Labour Organization and other multinational authorities:
That the supply of inputs be guaranteed in all healthcare centers or patient care sites.
That physicians have their children’s education and fam ily’s livelihood guaranteed through an insurance policy, in case of death. Payment of their full salary to their family, social security until their children are of age, free education up to the university level and lifelong social security for their spouse.
That when physicians and healthcare staff experience personal or property damage, reparation be guaranteed, as well as appropriate compensation if the physicians are unable to continue practicing their profession, with their families’ insurance being activated.
That compensation be commensurate with the risk and job performed, so that physicians can work for a single institution, rather than having to double and triple their shifts.
That the physician’s reputation be respected, and that when it is unfairly damaged, no matter by whom, repa ration of the damage to his/her professional image and prestige be required.
That filming a physician at work, publishing his/her image on networks without his/her authorization be considered illegal, have consequences for the aggressor and be punished by forcing the aggressor to repair the damage financially and morally.
That work shifts during training be those stipulated by law, without the excuse that since they are staff in train ing, their shift may be extended without justification; and, if it is, that they be compensated according to the time worked.
That all types of transportation be prioritized for facilitat ing the travel of physicians and healthcare personnel.
That their status as women be respected, along with their particular periods such as pregnancy, breastfeeding and their children’s illnesses.
That there be an office especially in charge of matters related to physicians and healthcare staff, which will streamline and activate the mechanisms for enforcing the law, punishing crimes and guaranteeing physicians the previously mentioned line items; that each country’s law be enforced in all its breadth and rigor, and that with this effort, flaws which injure the physicians’ profes sional practice in these difficult circumstances may be eradicated.
The Foro Internacional de Medicina Interna (FIMI) [International Forum of Internal Medicine] has drafted a decalogue of the conditions under which all physicians should be able to practice their profession (Annex 2).
Likewise, the message from the FIMI authorities for all Latin American colleagues is transcribed (Annex 3).











 text in
text in