Introduction
Cocaine is the second most-used illegal drug in Colombia, exceeded only by marijuana, with a prevalence of consumption in 2017 of 3.23%. With regard to geographical distribution, Antioquia and the "Coffee Belt" departments have higher illegal drug consumption rates than the rest of the country, and it is more prevalent in men than women, with greater consumption between 18 and 24 years of age 1.
To date, no national estimate of emergency room visits related to the consumption of psychoactive substances (PASs) has been recorded. Some isolated studies have been performed in Bogotá, which estimate that eight out of 100 people presenting to the emergency room have used some type of PAS in the last six hours 2.
The reported incidence of myocardial infarction in patients with cocaine-associated chest pain ranges from 0.7 to 5.7% 3,4,5 and appears to be a significant contributor to AMI in young people.
We present a case of acute myocardial infarction associated with the use of cocaine in a young, addicted patient.
Clinical case
We present a male 38-year-old patient who was admitted to the emergency room due to three days of sharp retrosternal pain triggered by physical exertion and associated with dyspnea and nausea. The only significant medical history was use of inhaled cocaine for the last 10 years and an alcoholic drinking habit for the same length of time, with no other findings on a review of systems.
On physical exam, the patient was in satisfactory general condition with the following vital signs: blood pressure 127/85 mm/Hg, heart rate 95 bpm, respiratory rate 21 bpm, and oximetry 97% with no need for supplementary oxygen. The rest of the systems had no significant findings.
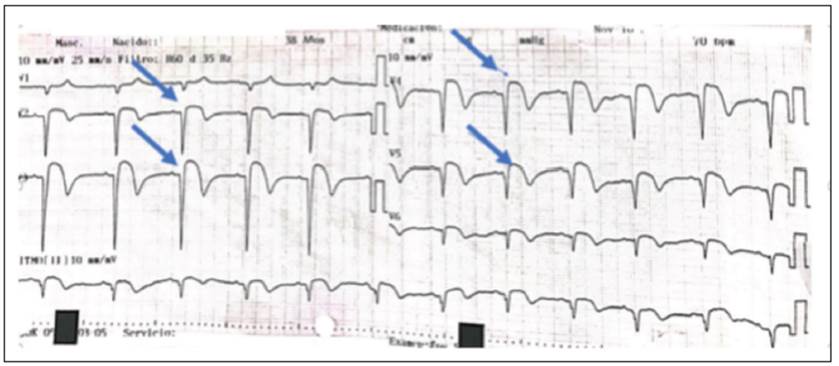
A 12-lead electrocardiogram showed an extensive anterior subepicardial lesion (Figure 1), constituting an acute myocardial infarction (AMI) with ST segment elevation. Two hours later he underwent primary angioplasty, finding 100% obstruction of the proximal third of the anterior descending artery (Figure 2A), where two medicated stents were implanted (Figures 2B-2C).
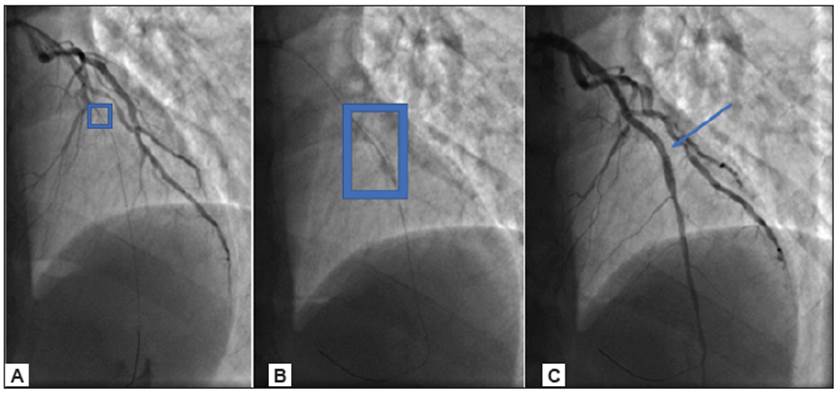
Figure 2 Primary angioplasty, finding 100% obstruction of the proximal third of the anterior descending artery (Figure 2A), where two medicated stents were implanted (Figures 2B-2C).
The patient progressed satisfactorily without mechanical or electrical complications from the infarction. He had no further chest pain episodes, and his echocardiogram showed ischemic heart disease with a 30% left ventricular ejection fraction. Therefore, he was started on neurohumoral inhibition, which he tolerated well. The first phase of cardiovascular rehabilitation was completed, and after being seen by psychiatry and being admitted to the addiction control program, he was discharged four days after the infarction to complete outpatient treatment for one year with dual ASA+prasugrel antiplatelet therapy, with no further complications.
Discussion
All patients with chest pain after cocaine ingestion must have an immediate 12-lead electrocardiogram (ECG) and a chest x-ray, since in addition to acute coronary syndrome, the differential diagnosis includes aortic dissection which was present in some case series in which a high percentage of patients (>20%) had a recent history of drug use and dissection 10,11.
Regarding the approach to chest pain, the electrocardiogram reading and interpretation of cardiac biomarkers will be carried out as indicated in the fourth definition of infarction, as studies suggest that it is feasible and safe to use risk stratification and the classic clinical approach when dealing with a patient with chest pain and associated cocaine use 12.
In general, cocaine-associated acute myocardial infarction occurs more frequently shortly after use, with a 24 times higher risk after the first hour of use 13. However, it has been shown that even low or undetectable concentrations may trigger acute coronary events; therefore, the studies have reported that the range may go from the first minute to up to four days after use . 14
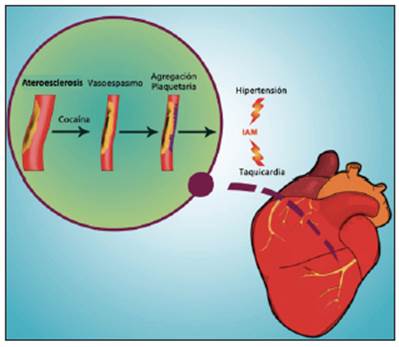
Cocaine's effects on the cardiovascular system are very diverse, with several mechanisms that can facilitate myocardial ischemia and lead to an acute myocardial infarction. The main mechanism is related to increased circulating norepinephrine secondary to inhibited reuptake. This results in an increased cardiovascular sympathetic response which triggers greater myocardial oxygen demand and lower myocardial perfusion secondary to coronary vasospasm 6,7.
While this is the most frequently described form, chronic use has been reported to accelerate atherosclerosis through the development of vascular endothelium defects leading to increased permeability to peroxidase and low-density lipoproteins 8. Associated thrombosis has been described due to increased platelet activation and aggregation 9 (Figure 3).
Studies have reported that 56-80% of electrocardiograms in patients with cocaine-associated chest pain are abnormal 9, but not all changes indicate acute ischemia or AMI. In a study of 238 patients, 33% had a normal ECG, 23% had nonspecific changes, 13% had a left ventricular hypertrophy pattern and 13% only had an early repolarization pattern. Electrocardiographic changes specific for ischemia or infarction were only present in a minority of patients; only a small percentage of patients with cocaine-associated chest pain and J point elevation actually have an MI 9.
With regard to the coronary stratification method, the attending physician should follow the general principles for evaluating risk in patients with possible acute coronary syndrome in the general population, based on the best available evidence, considering the electrocardiographic anomalies found and cardiac biomarker results, and according to the available resources.
If a cocaine user presents with a myocardial infarction with ST segment elevation within the window of time since the onset of pain, immediate thrombolytic therapy or a percutaneous coronary intervention should be performed, keeping in mind the high risk of thrombosis due to increased platelet activation and aggregation 9. As was previously explained, only a small percentage of patients with cocaine-associated chest pain and J point elevation actually have an MI; therefore, if primary angioplasty is available within the stipulated time frame, this is the strategy of choice.
The importance of this case report lies in knowing that the mechanism of infarction in this group of patients is not only secondary to vasospasm. Therefore, this patient, as described, underwent cardiac catheterization with secondary angioplasty within the stipulated time frame, just as a non-user would.
Cocaine damages the vascular endothelium, increases platelet aggregation and impairs the normal fibronlytic pathways. Consequently, AMI is not only a result of the sympathetic response, and thus the use of ASA, P2Y2 receptor antagonists, glycoprotein IIb/IIa inhibitors, heparins and statins is clearly pathophysiologically justified in this group of patients.
Patients with myocardial infarction without ST segment elevation or unstable angina have a higher risk of subsequent events, as well as a greater chance of benefiting from early coronary stratification by cardiac catheterization and, depending on the findings, myocardial revascularization, just like patients with ACS unrelated to cocaine use 9.
Stopping cocaine use is the main goal of secondary prevention, since chest pain recurrence is high among patients who continue to use 15. Therefore, a decreased risk of readmission may depend on the implementation of addiction rehabilitation programs.
Stopping smoking, decreasing alcohol use, controlling comorbidities like hypertension and diabetes, and aggressive lipid-lowering therapy, together with cardiovascular rehabilitation, are strategies that do not have clinical trials in this specific population, but which are standard for patients with coronary disease in general, and apply to this condition 9.
Whether in the context of stent implantation, STEMI or a high associated thrombotic risk, dual antiplatelet therapy with high-intensity P2Y2 receptor antagonists such as prasugrel and ticagrelor is indicated for the currently established length of time 16, a strategy which was used with the patient described.
The chronic use of beta blockers should be reserved for those with strong indications such as left ventricular systolic dysfunction or ventricular arrhythmias. Their use as primary prevention in the context of chronic cocaine use has not proven useful in reducing events 9.
Conclusions
In recent years, cocaine use, beginning at a very early age, has increased both in the Colombian as well as the global population, with its use being one of the main causes of ACS in young patients.
The pathophysiological mechanisms are diverse and range from an increased sympathetic response to increased atherosclerosis and the risk of thrombosis, with a variable time range for clinical presentation after use. Diagnosis and treatment do not differ much from the indications given by international guidelines for managing patients with ACS not related to cocaine use.
Proper management of the addiction takes on special relevance in this group of patients as a secondary prevention strategy, together with the recommendations which apply for coronary events unrelated to drug use.











 texto em
texto em