Introduction
Paracoccidioidomycosis (PCM) is a systemic mycosis caused by Paracoccidioides brasiliensis and endemic to Latin America. It is more common in Brazil, which has 80% of the cases, followed by Colombia, Ecuador, Venezuela, Bolivia and Argentina. The incidence in our country is 0.52.2/100,000 inhabitants/year, and Caldas is one of the most affected departments with 2.9/1,000,000 inhabitants/year. Being male and agriculture, especially exposure to coffee and tobacco fields, have been recognized as risk factors for contracting the fungus, while smoking, malnutrition and alcoholism are associated with the development of symptomatic disease 1,2.
The germ is acquired through the respiratory tract and mainly affects the lungs, lymph nodes, mucosas, skin, adrenal glands and bone. With this in mind, four clinical states have been described: the acute/subacute or juvenile form which affects people under the age of 30 and develops within a few weeks, accounting for 10-15% of cases; the chronic or adult form which is seen between 30 and 50 years of age and takes months to progress, accounting for 80-90% of cases; the subclinical or asymptomatic form; and the residual form or sequelae 3,4. We present the case of a patient with the acute/subacute form, with lymph node involvement and eosinophilia.
Case presentation
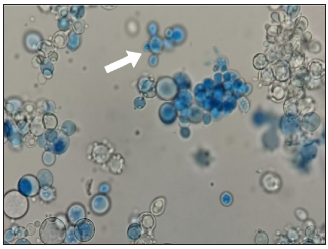
In a tertiary care hospital in the department of Caldas, in Colombia's coffee-growing zone, a 25-year-old man was seen in August 2019 with a complaint of one month of mesogastric pain, fever, a 6 kg weight loss and diaphoresis. He had no significant history except that he used to work as a farmer, and he smoked and used marijuana. The physical exam showed a body mass index of 19.4 and cervical and axillary lymphadenopathy, with no other pathological findings. On lab exams, he had a complete blood count showing 16,400 leukocytes/µL, 4,000 eosinophils/µL, 8,800 neutrophils/µL, 2,300 lymphocytes/µL, hemoglobin 13.5 g/dL and 565,000 platelets/µL; C-reactive protein was 25 mg/dL (normal range < 1 mg/dL) and albumin was 3.3 g/dL; the peripheral blood smear, lactate dehydrogenase, kidney and liver function tests and coagulation tests were normal. An abdominal tomography showed enlarged retroperitoneal lymph nodes (Figure 1A) and a chest tomography and spirometry were normal. An upper GI endoscopy found acute erosive esophagitis. Serology for HIV and hepatitis B was negative, while hepatitis C was positive but negative for viral load. A biopsy was taken from a cervical lymph node which reported caseous necrosis, negative Ziehl-Neelson stain and fungal stains which were positive for paracoccidiodes spp. (Figure 2). Subsequently, a serum immunodiffusion test for fungi was performed, which was reactive for paracoccidiodine. Serum protein electrophoresis showed a monoclonal spike in the gamma region, IgE > 2,000 IU/µL (normal range <150 IU/µL), IgG 3,153 mg/dL (normal range 600-1,808 mg/dL) and IgM 395 mg/dL (normal range 50-283 mg/dL), while IgA was normal. Given these findings, it was considered to be a mild acute/subacute PCM, and he was treated as an inpatient with oral itraconazole 200 mg q 8 hr. for five days and then discharged with a prescription of 200 mg/ day for a total of nine months.
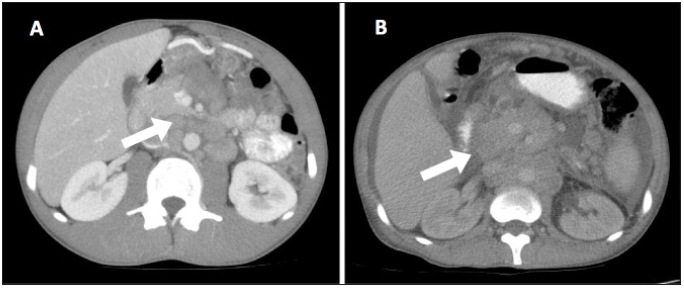
Figure 1 Abdominal computerized tomography with contrast. A. Image from the beginning of the illness: multiple lymphadenopathies with areas of central necrosis and post-contrast transcavity reinforcement of the omentum, hepatic hilum, para-aortic area and mesentery (see arrow) B. Image five months after abandoning treatment: large conglomerates of retroperitoneal lymphade nopathies which had grown in size and number compared with the previous study (see arrow).
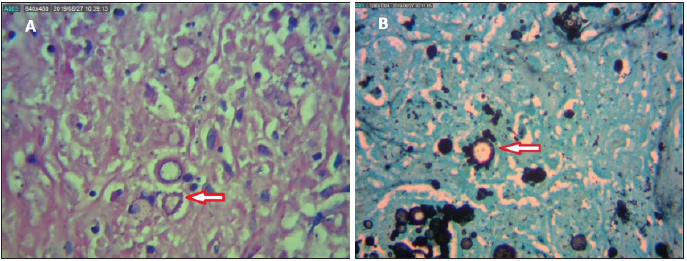
Figure 2 Histopathology of a cervical lymph node. A. Periodic acid-Schiff stain with 40X magnification. B. Grocott-Gomori stain with 40X magnification. Numerous 10-15 micron diameter spheroidal or ovoid formations showing capsule highlighting with “boat rudder” budding (see arrows).
However, the patient stopped the outpatient treatment and follow up and returned to the emergency room five months later with the same symptoms. His lymphadenopathy had grown since the previous assessment, he had jaundiced sclera and clinical signs of ascites. At that point, the labs showed 20,000 leukocytes/µL, 2,200 eosinophils/ 15,400 neutrophils/µL, 1,400 lymphocytes/µL, hemoglobin 8.3 g/dL, hematocrit 25.6%, mean corpuscular volume 82.7 fl, 274,000 platelets/µL, total bilirubin 2.5 mg/dL, direct bilirubin 1.8 mg/dL, indirect bilirubin 0.7 mg/dL, alkaline phosphatase 613 IU/l (normal range 38126 IU/µL), and gamma-glutamyl transferase 1,671 IU/l (normal range 15-73 IU/µL), with normal transaminases.
A new abdominal tomography revealed increased retro-peritoneal lymphadenopathy and hepatosplenomegaly (Figure 1B), and mediastinal lymphadenopathy appeared on chest tomography. The cervical lymph node biopsy was repeated with histopathological findings similar to the first one, stains and tissue cultures ruled out bacterial and mycobacterial superinfection, and a fungal culture using Sabouraud medium and potato-dextrose agar revealed white cerebriform fungal growth (Figure 3). During his hospitalization, he experienced abdominal pain which was very difficult to control, and the ascites increased. He therefore underwent paracentesis, and the peritoneal fluid studies showed 1,200 lymphocytes/µL, with no other cells; stains and cultures for the usual germs were negative, a polymerase chain reaction (PCR) test for mycobacterium tuberculosis was negative and cytology was negative for neoplasia. The serum-ascites albumin gradient was 1.2, with no thromboses or portal hypertension on a duplex exam of the portal vessels. In light of the progression of his systemic involvement, intravenous amphotericin B was added for three weeks, reaching a cumulative dose of 1,050 mg, after which ambulatory treatment with oral trimethoprim-sulfamethoxazole (TMP-SMX) 960 mg q 12 hr. was ordered for one month, followed by 480 mg q 24 hr. for two years. However, the patient once again dropped out of follow up and his current status is unknown.
Discussion
Paracoccidioidomycosis is a diagnostic challenge, as its clinical signs, especially in the acute/subacute form, are similar to those of other disorders such as Hodgkin lymphoma and tuberculosis 4,5. In this patient, a lymphoproliferative disorder was initially suspected. Pulmonary involvement is the most frequent finding, occurring in 64% of cases, and oral mucosal involvement occurs in 50%, while generalized lymphadenopathies only account for 28% 6. This depends on the type of clinical presentation, with the chronic form being the most frequent and where pulmonary involvement is seen, with radiological findings of ground glass opacities and cavitary nodules, as described in case reports in our setting of patients with mild chronic forms and a more severe case with associated adrenal crisis and cardiopulmonary arrest 7,8. The acute/subacute form is seen in young patients and tends to involve the lymph nodes more, due to hematogenous dissemination of the fungus facilitated by immune system immaturity 6. In a cohort study of pediatric patients, 87% were found to have generalized lymphadenopathy, 75% fever, and 65% weight loss, but only 5% had abdominal pain and 3% ascites 9. In our setting, only two cases of acute/subacute PCM have been described to date, one of them being a 12-year-old patient, which contrasts with our patient who was already in the third decade of life, and had marked abdominal pain and ascites 10,11.
The laboratory findings in acute/subacute PCM show anemia in 88% of cases, leukocytosis in 78%, hypoalbuminemia in 65%, hypergammaglobulinemia in 81%, and eosinophilia in 30-78% of cases 4,9, as was found in our patient. Eosinophil elevation is a very striking finding which has been described in another case report in our country and is attributed to high levels of IL-5 and a Th2 cellular response, although unlike our patient, there was no liver involvement or ascites 11. The marked production of immunoglobulins may explain the false positive for hepatitis C antibodies, which has been described in a peritoneal dialysis patient with peritonitis due to Candida parapsilosis12. However, this is the first report of this finding in individuals with PCM, to date. While the cultures and histopathology identify the presence of the fungus, the time it takes to obtain results may delay treatment; therefore, the serum antibody test could help provide an earlier diagnosis, although it has the problem of cross reactivity with other mycoses and highly variable results from one laboratory to another 5,13. In Colombia, nested PCR has been studied for detecting the gene which codes for the paracoccidioides gp43 membrane protein in tissue samples, bronchoalveolar lavage and sputum, finding 100% sensitivity and specificity. Thus, this could be another more precise and rapid diagnostic tool 14.
Our patient was treated according to the recommendations from the most recently published guidelines 4. Itraconazole was used as the first line because he initially had a mild presentation. This medication offers an earlier cure compared with TMP-SMX, although some authors state that it is also more effective 15,16. However, we faced a difficulty with compliance which led to disease progression and the appearance of a more severe picture which required amphotericin B, with reported cure rates of 100% at one year of follow up 17. For chronic treatment, TMP-SMX continues to be an acceptable choice due to its low cost and easier access, with cure rates of 74% and compliance in up to 68% of patients, which is why it is another treatment strategy in our setting, as used with our patient 18.
This clinical case shows the importance of considering acute/subacute PCM in the differential diagnosis of young patients with lymphadenopathies and eosinophilia. In addition, it is important to seek new strategies like PCR to confirm this infection more rapidly and, finally, consider TMP-SMX as an option in patients with mild forms and difficulty in obtaining itraconazole.











 text in
text in