Introduction
Over the last decades, the world's population has experienced an increase in the prevalence of chronic noncommunicable diseases (NCDs) 1 such as obesity, hypertension, atherosclerosis and type 2 diabetes mellitus, with an estimated 15 million deaths per year in people between the ages of 30 and 69. This is a consequence of rapid and unplanned urban development, the globalization of unhealthy lifestyles and population aging increasing the prevalence of cardiovascular diseases (CVDs), which are currently the first cause of death worldwide (70%).
Preoperative assessment is a challenge in this setting, since pulmonary complications are as common and morbid as cardiac complications, with an elevated mortality rate close to 50%, which is also reflected in the data reported by the national surgical quality improvement program (NSQIP), in which postoperative pulmonary complications reached 6% 2,3. Likewise, cardiovascular events require attention in order to identify risk groups, as a 3% incidence has been documented, and venous thromboembolism-DVT (deep vein thrombosis, pulmonary embolism) constitutes another complication with elevated morbidity and mortal ity which affects approximately one in every four general surgery patients who do not receive preventive measures 4. Pulmonary embolism is one of the most common pre ventable causes of inpatient death following surgery 5.
In light of these considerations, the goal of physicians involved in preoperative assessment is to detect risk fac tors that may increase surgical complications beyond the baseline and propose strategies to reduce the risk. To do this, patients must be stratified according to the possible perioperative adverse events. For cardiovascular adverse events, Goldman, Detsky and Lee indices can be used; the Caprini scale is valid for evaluating the risk of venous thromboembolism (VTE) in surgical patients; and while no stratification models for pulmonary risk in general sur gery have been validated to date, the American College of Physicians (ACP) has adopted some specific respiratory complication risk estimation scales 6-10.
The American College of Surgeons National Surgical Quality Improvement Program's (ACS-NSQIP) surgical risk calculator is an interactive risk tool first published in 2013 as an online software which requests information on demographic data, functional status, comorbidities and the American Society of Anesthesiologists' (ASA) functional class classification 11.
The importance of this study lies in the fact that the Hospital Central del Instituto Venezolano de los Seguros Sociales (IVSS) Dr. Miguel Pérez Carreño handles a high volume of surgery, which has been limited by the socio economic crisis facing the country. Thus, we believe it is necessary to compare the ACS-NSQIP calculator to stan dardized risk indices for pneumonia, cardiac complications and venous thromboembolism.
Materials and methods
Study design and location
This is a single-center, cross-sectional correlational study in patients over the age of 35 undergoing noncardiac surgeries under the care of general surgery, obstetrics-gynecology, urology, plastic surgery, neurosurgery and trauma at the Hospital Central del IVSS "Dr. Miguel Pérez Carreño," who were seen for internal medicine and emergency preoperative consultation by the previously mentioned services between June 2018 and March 2019. Patients who were transferred to another hospital, were discharged from the hospital, or had pneumonia, DVT or a cardiovascular event at the time of assessment were excluded.
A registration form was created on which to record the admission medical chart number, past medical history, surgical intervention data, physical exam, and data on post anesthesia recovery, resuscitation, intensive care unit stay, preoperative risk indices results and 30-day postoperative follow up. For consistency, the same person carried out the entire medical chart review and physical exam, entered all the patients in the risk calculator (assigning them all a CPT code) and stratified the risk using the Lee, ACP pneumonia and Caprini scale scores. The outcomes found after the surgical intervention included pneumonia, VTE and cardiovascular complications (myocardial infarction, cardiac arrest, pulmonary edema, de novo arrhythmias, and cerebrovascular disease). Postoperative follow up was carried out through outpatient consults with the respective surgical service and/or by telephone, assessing for the presence of the previously mentioned morbidities, for up to 30 days.
Data analysis
Continuous variables were summarized using means and standard deviation ifthe distribution was normal or medians and interquartile ranges if the distribution was not normal. Categorical variables were summarized using frequencies and percentages. The calculator's ability to distinguish between patients with or without the respec tive complications was summarized using the area under a receiver operating characteristic curve (AUC). The AUC may range from 0.5-1.0, with higher values indicat ing better predictive ability or discrimination. Statistical analyses were performed using SPSS 22. P values <0.05 were considered statistically significant. The results were reported in tables and figures. The sample was intentional and data imputation was used if underreporting was less than 20%, to mitigate this effect.
Results
Epidemiological data and medical conditions of patients with noncardiac surgeries
Ninety-eight patients were selected (Figure 1) with an average age of 55 years ± 14, and females accounting for 54.1% (n = 53). A total of 62.2% (n = 61) of the patients had a normal BMI. In terms of surgical service distribu tion, general surgery predominated with 73.5% (n = 72), and most of the surgeries were elective, with 60.2% (n = 59). With regard to preoperative risk scales, the ASA categorized 59.2 % (n = 72) as class II. The most frequent range on the Lee index was II, with 67.3% (n = 66), and 53% of the patients (n = 52) were classified as very high risk for thromboembolic disease according to the Caprini scale. On the ACP pneumonia risk scale used to assess the risk of respiratory complications, class II predominated with 40.8% (n = 40) (Table 1).
Figure 1 Flowchart of the selection of noncardiac surgery patients at Hospital del IVSS Dr. Miguel Pérez Carreño
Table 1 Sociodemographic characteristics of noncardiac surgical patients at Hospital del IVSS "Dr. Miguel Pérez Carreño
| Variables | |
|---|---|
| N | 98 (%) |
| Age (years) (*) | 55 ± 14 |
| Sex | |
| Female | 53 (54.1) |
| Male | 45 (45.9) |
| Body mass index (BMI) | |
| Underweight | 2 (2) |
| Normal | 61 (62.2) |
| Overweight | 21 (21.4) |
| Obesity | 14 (14.3) |
| Surgical service | |
| General surgery | 72 (73.5) |
| Trauma surgery | 16 (16.3) |
| Neurosurgery | 4 (4.1) |
| Urology | 4 (4.1) |
| Obstetrics and gynecology | 2 (2) |
| Emergency surgery | |
| Yes | 39 (39.8) |
| No | 59 (60.2) |
| ASA classification | |
| I (healthy patient) | 25(255) |
| II (mild systemic disease) | 58 (59.2) |
| III (severe systemic disease) | 15 (15.3) |
| Lee cardiac index | |
| Class I | 28 (28.6) |
| Class II | 66 (67.3) |
| Class III | 4 (4.1) |
| Caprini scale | |
| Low | 6 (6.1) |
| Moderate | 8 (8.2) |
| High | 32 (32.7) |
| Very high | 52 (53.1) |
| ACP scale | |
| Class I | 33 (33.7) |
| Class II | 40 (40.8) |
| Class III | 25 (25.5) |
| IVSS: Instituto Venezolano de los Seguros Sociales [Venezuelan Social Security Institute]. American College of Physicians (ACP) scale. (*) mean ± standard deviation. Source: prepared by the authors based on the study findings. | |
With regard to functional status, 91.8% (n = 90) of the patients were dependent. The three most frequently found comorbidities were hypertension 36.7% (n = 36), smoking 17.3% (n = 17) and diabetes mellitus 10.2% (n = 10) (Table 2).
Table 2 Medical conditions of noncardiac surgical patients at Hospital del IVSS "Dr. Miguel Pérez Carreño".
| Medical conditions | n | % |
|---|---|---|
| Functional status | ||
| Independent | 90 | 91.8 |
| Partially dependent | 7 | 7.1 |
| Dependent | 1 | 1.0 |
| Hypertension | 36 | 36.7 |
| Smoker t | 17 | 17.3 |
| Diabetes mellitus | 10 | 10.2 |
| Dyspnea | 5 | 5.1 |
| Steroids* | 2 | 2.0 |
| Ascites* | 2 | 2.0 |
| Disseminated cancer | 2 | 2.0 |
| Heart failure* | 1 | 1.0 |
| COPD | 1 | 1.0 |
| Acute renal failure II | 1 | 1.0 |
| *In the last 30 days. t In the last year. II >3mg/dLof creatinine. Source: prepared by the authors based on the study results. | ||
Assessment of postoperative complications
Postoperative complications related to the type of surgery were reported in 23.4% (n = 23), with pneumonia being the most frequent at 14.2% (n = 14). Most of the complications occurred in general surgery patients, ac counting for 20.4% (n = 20). With regard to the time of onset of postoperative complications, 78.2% (n = 18) of the cases occurred in the first 15 days, with pneumonia accounting for 50% (n=9), and were related to the group of patients undergoing emergency surgery (52.1% [n = 12]) (Table 3).
Table 3 Report of postoperative complications in noncardiac surgery patients by type of surgery and time of onset.
| Pneumonia | CV | DVT | Total | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Surgery | 11 | 55.0 | 7 | 35.0 | 2 | 10.0 | 20 | 100.0 |
| Neurosurgery | 2 | 100 | 0 | 0.0 | 0 | 0.0 | 2 | 100.0 |
| Urology | 1 | 100 | 0 | 0.0 | 0 | 0.0 | 1 | 100.0 |
| Total | 14 | 60.9 | 7 | 30.4 | 2 | 8.7 | 23 | 100.0 |
| Less than 15 days after surgery | 9 | 50.0 | 7 | 38.9 | 2 | 11.1 | 18 | 100.0 |
| 15 days or more after surgery | 5 | 100.0 | 0 | 0.0 | 0 | 0.0 | 5 | 100.0 |
| Total | 14 | 60.9 | 7 | 30.4 | 2 | 8.7 | 23 | 100.0 |
| Cases out of the total population (n=98) | 14 | 14.2 | 7 | 7.1 | 2 | 2.0 | 23 | 23.4 |
| Abbreviations: CV= cardiovascular; DVT = deep vein thrombosis. Source: prepared by the authors based on the study results. | ||||||||
Assessment of the ACS-NSQIP calculator's performance
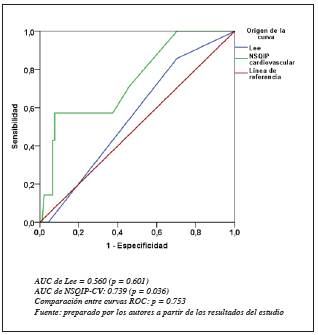
Receiver operating characteristic (ROC) curves were created for each type of complication. In the general analysis, only the ROC curves for pneumonia (ABC: 0.695 95%CI [0.54-0.85], p = 0.017) and cardiac complications (ABC: 0.739 IC 95% [0.55-0.93], p = 0.036) were significant. The Lee and ACP standards did not have statistical significance in the ROC risk estimate of cardiovascular complications or pneumonia, with ABC values of 0.560 95%CI [0.37-0.75], p = 0.601 and ABC: 0.624 95%CI [0.48-0.77], p = 0.140, respectively (Figures 2-4). The ROC curve for the Lee standard is not included in the cited figures. Of these, only VTE had a narrow confidence inter val; however, it was not ultimately statistically significant for the ABC.
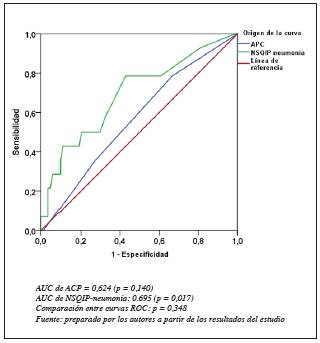
Figure 2 NSQIP receiver operating characteristic (ROC) curves for pneumonia and pneumonia complications.
Discussion
In this study, the ACS-NSQIP calculator was compared with the Lee, Caprini and ACP scales. The sample was characterized by being largely female, in the sixth decade of life, and predominantly from the general surgery service, which coincides with the study 12 carried out in Caracas at the Hospital del IVSS Dr. Domingo Luciani. However, these studies are not consistent with the age and sex of the patients described by Müller et al. 13.
In the study by Contreras M 14, most of the patients were in ASA class I, and the top three medical conditions reported were dyslipidemia, cavities and obesity. These findings differ from the results of the current study, in which we showed that the greatest number of cases were in ASA class II, and hypertension, smoking and diabetes were the three most frequent entities under patient medical condi tions. These results could be related to the higher average age in our study.
The main postoperative complication was pneumonia, with 60.9%, which is in line with the study by Gupta S. et al. 15 in which 48 (81.3%) of 59 patients with postopera tive respiratory complications had pneumonia. However, its epidemiology varies widely, as shown by Chughtai M et al. who reported an incidence of 0.97% 13. The study by Fernández E. et al. reported that cases with pulmonary complications had smoking, chronic obstructive pulmonary disease, diabetes, longer surgeries, intraoperative hypoten sion, greater administration of fluid therapy, and transfusions as risk factors. It should be noted that our patients coincided with the presence of several of these factors. Cardiovascular complications occurred in 7.2% of the cohort, a similar find ing to that described in previous analyses which estimated its occurrence at 5.8% 16. Furthermore, epidemiological studies show that the incidence of symptomatic postopera tive DVT is approximately 2% after high-risk interventions 17, a fact which is comparable with our outcome.
With regard to the calculator's performance, the analy sis found statistical relationships between risk estimations and the occurrence of events for the categories of cardiac complications and pneumonia which were even higher than the respective Lee and ACP indices. This is comparable to the results of Edelstein et al.'s 18 study in which the ACS-NSQIP calculator predicted cardiac complications (p<0.001) and pneumonia (p <0.001). The opposite occurred with VTE, in which the Caprini scale was superior with an ROC of 0.620 (p = 0.735) compared to the calculator ROC of 0.586 (p = 0.631); this was not significant, probably due to the scant number of events. This result is also comparable with the conclusions of Yap et al. 19 who showed that the ACS-NSQIP calculator had good predictive ability for pneumonia (AUC 0.93), all-cause mortality (AUC 0.89) and morbidity (AUC 0.88). However, its prediction was poor to average for kidney failure, return to surgery, surgical site infection, urinary tract infection and VTE.
This study is limited by its sample size, a result of the problems faced by the Venezuelan healthcare system which affect this type of health care and may also have led to the low number of events which probably limited the perfor mance of the ACS-NSQIP calculator.
Conclusion
We believe that the calculator (ACS-NSQIP) is a useful risk tool for predicting postoperative complications like pneumonia and cardiovascular events. However, another study with a greater number of patients must be performed to detect more events and further validate the predictive ability of the calculator in these entities and even in venous thromboembolic disease. A weakness of this study is that sample size calculation was not performed.











 text in
text in