Introduction
Leiomyosarcoma (LMS) is an aggressive malignant neo plasm with a poor prognosis which may arise from smooth muscle cells in any part of the body, with soft tissues and organs like the uterus and gastrointestinal tract being the most frequent sites 1. It is one of the most common soft tissue sarcomas, after liposarcoma, with a prevalence close to 14%). It tends to appear in adulthood, with incidence peaks between the sixth and seventh decades of life 1. Although it is rare in young people, it is typically related to Epstein Barr virus infection in immunosuppressed states 3-6.
Today, soft tissue LMS is classified according to the site where it presents: skin, vascular and deep soft tissue 7,8. Somatic or peripheral and retroperitoneal LMSs fall into the deep soft tissue group, have the worst prognosis, and make up the largest group with over 50% of the cases 7,9.
Somatic or peripheral LMSs predominate in men and have a more favorable course, with a 64% five-year survival, compared with retroperitoneal LMSs which generally do not exceed 50%. In addition, their local recurrence and distant metastasis rates over an almost four-year follow up period are 8 and 45% respectively 10-13. Their occurrence in eye structures is unusual, with only a few LMS cases published in the literature, 11 of which are primary orbital tumors 14-25.
Leiomyosarcoma is diagnosed through histopathological and immunohistochemical studies 14-24. Its usual characteristics include interlacing cell fascicles; abundant eosino philic cytoplasm; pleomorphism; elongated, hyperchromatic nuclei; and, in most cases, smooth muscle actin, desmin and h-caldesmon positivity 3. Nuclear atypia together with necrosis and mitotic figures help differenciate it from leiomyoma 14,26.
Having received written authorization from the patient to publish this article and its accompanying images, we pres ent the case of a man with primary orbital LMS, along with his clinical, imaging, intraoperative and histopathological findings.
Case presentation
A 72-year-old male patient from Sabana de Torres, with no significant medical history, consulted due to eight months of progressive growth of the left frontotemporal region along with dysarthria, vision loss, headache, initially painless ipsilateral proptosis, and no other symptoms (Figure 1).

Figure 1 Left eye proptosis along with inflammatory changes and two satellite supraciliary adenopathies.
On physical exam, he was hemodynamically stable with anthropometric measurements suggestive of type 1 obesity. No other abnormalities were found, except for what was seen on head and neck examination, where a significant anterior, axial nonreducible displacement of the left eye was noted, with inflammatory changes, no excrescenses, and inability to move the eye, along with two ipsilateral, supraciliary, round, rubbery, painless, non-mobile masses approximately 4x3 and 2x2 cm.
Computerized axial tomography (CAT) showed an extensive hyperdense image concordant with an osteolytic lesion involving the bone table and soft parts of the left or bital frontal region, together with eyeball displacement, an enlarged lacrimal gland and frontal encephalomalacia (Fig ure 2A). The nuclear magnetic resonance (NMR) showed a hyperintense area on T2 and isointense to the extraocular muscles on T1, with a neoplastic appearance, invading the temporal fossa and adjacent soft tissues, with evident compression, and extending intraorbitally and intracranially (Figure 2B-C).

Figure 2 A. Simple head CAT showing clear invasion of the well-defined tumor mass towards the orbit, soft tissues and bone destruction in the left temporal region. B. T1 sequence nuclear magnetic resonance showing a heterogenous mass extending to the orbit and soft tissues in the temporal region. C. T2 sequence nuclear magnetic resonance from a coronal view showing a hyperintense, heterogenous lesion in the supratemporal orbit causing inferior displacement of the eyeball and frontal-zygomatic bone destruction.
Due to a suspected metastatic origin, extension studies were performed which did not reveal any abnormalities. Therefore, an incisional biopsy was carried out, which suggested a high-grade mesenchymal malignant tumor with extensive necrosis due to tumor coagulation and hemorrhage. On the immunohistochemical analysis, the sample was strongly positive to smooth-muscle specific actin (SMA) and desmin, with no reactivity for CK7, CK20, HMB45, CD34, CK AE1/AE3, S.100, SOX10 or TTF-1. The Ki-67 cellular proliferation index was 90%. The previous findings were compatible with a diagnosis of high-grade leiomyosarcoma (Figure 3).
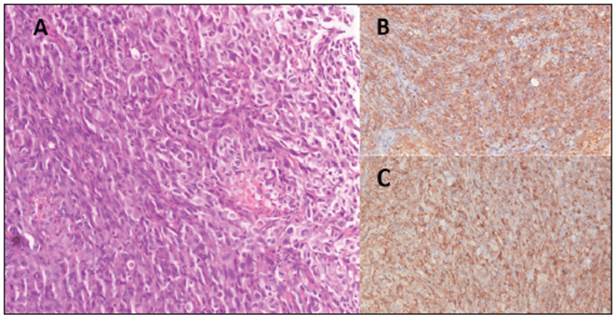
Figure 3 A. 200x microscopy (H&E) showing a fusicellular lesion with an infiltrative pattern made up of cells with elongated, oval, hyper chromatic, pleomorphic nuclei with visible nucleoli. Bizarre cells and more than 10 atypical mitoses in 10 fields can be seen. B-C. Immuno histochemistry showing positivity in the tumor population for desmin and AML.
A frontal, temporal and left orbital craniotomy was subsequently performed, finding an approximately 8x8 cm intra-axial frontal basal tumor which was moderately vascularized with high infiltration of the dura mater and bone, and extended to the eyeball and subtemporal region. Total resection of the mass was performed, with negative margins, extending to the base of the skull and medial orbital wall, followed by reconstruction with a temporal neurovascular flap, achieving coverage of the orbital and frontal and maxillary sinus defect (Figure 4A). No com plications were reported during the procedure, and the patient had immediate resolution of his speech difficulty while recovering in the hospital.

Figure 4 A. Block resection of the orbital tumor and reconstruction with a temporal island flap and a neurovascular flap. B. Post-surgical status of the patient with a large defect due to left lateral craniofacial resection.
Finally, radiation was begun and had a favorable course, with no signs of recurrence or metastasis after 10 months of follow up (Figure 4B).
Discussion
The most common presentation of peripheral LMS is in the extremities and trunk, with a very low incidence in the head and neck structures, amounting to 4% of the sarcomas in these areas 11,27,28. Its origin may be primary or secondary to metastasis, mainly from the uterus and retroperitoneum. It may even occur in immunocompromised patients or as a sequela of radiation therapy for other types of cancer 29-31.
In their systematic review, Saluja T. et al. found that 58% of primary head and neck LMSs are found in extraoral areas, with the thyroid, larynx and paranasal areas being the most common, followed by intracranial and auricular regions9. These tumors are said to have a significantly better prognosis than those that are secondary to metastasis, due to the relationship between the site of origin and the determination of the behavior and biological characteristics of this type of neoplasms7 , 29.
To date, 11 cases of primary orbital LMS have been published, of which only two have been in men. The most commonly reported signs and symptoms were painless proptosis, followed by decreased eye movements, diplopia, the presence of a mass, and reduced visual acuity. As with our patient, imaging was used in most cases to describe the le sion and evaluate its extent, and the diagnosis was also made through histopathology and immunohistochemistry 14-24.
Orbital LMS is often located in the posterior portion of the eye, with its origin considered to be the smooth muscle of the blood vessels. When it is found in the anterior portion of the eye, as in this case, it is associated with Müller's muscle or its equivalent in the lower eyelid 17.
The differential diagnoses considered both in this and the reported cases were rhabdomyosarcoma, lymphoma, fibrosarcoma, orbital pseudotumor, metastases and benign conditions like cavernous hemangioma 17,22,32. Lymphatic involvement, as seen in our patient, is an unusual finding, occurring in fewer than 10% 28.
Given LMS's aggressiveness for local recurrence and distant metastases to organs like the brain, lung, bone and liver, the recommended first line treatment is total resec tion of the lesion with negative margins, with or without adjunct treatment 1,28. The known prognostic factors for this type of tumors are the site of origin, histological grade, both bone and neurovascular involvement, and size, with the latter ruled out in Saluja T. et al's study, as they found that patients with 2-4 cm tumors had better survival than those with smaller ones. In addition, the importance of adjunct treatment in reducing morbidity and mortality rates for people with LMS should be highlighted29,33.
In the published cases, three died 12-15 months after sur gery, one due to causes unrelated to the tumor and the other two due to distant metastases 15,18. Our patient, after 10 months of follow up, had had a favorable evolution with no evidence of tumor activity; however, knowing how the tumor behaves, it was decided to continue monitoring to detect any indication of metastasis or local recurrence promptly.
Conclusions
Leiomyosarcoma in the head and neck is very rare, with orbital presentation being one of the least reported. Histopathology and immunohistochemistry studies in addition to clinical suspicion are fundamental for its correct diagnosis and prompt treatment. Therefore, total resection of the lesion together with adjunct treatment is an effective treatment in light of the aggressiveness and poor prognosis of this type of cancer.











 texto em
texto em 


