Introduction
In December 2019, an acute adult respiratory syndrome caused by a novel coronavirus (SARS-CoV2) appeared in Wuhan, China, quickly reaching pandemic levels 1,2. To date, more than five million people infected in 188 countries and 340,000 deaths 3 have forced governments to implement strict social isolation measures 4. Educational institutions, including universities, closed their doors to decrease the risk of contagion 5. At this point, the SARS-CoV2 pandemic has dominated the educational and clinical settings and is the biggest disrupter of all aspects of life 6,7.
Hospitals are among the places with the highest risk of contagion, and there is a lack of personal protective equipment to decrease the risk of contagion for healthcare personnel 8. In light of this, clinical rotations in much of the world were suspended and theory courses were transferred to virtual modalities, in most cases hastily 9. In addition, some countries decided to graduate their last-year medical students early, to cover the deficit of professionals needed to care for infected patients 9-14.
Currently, the focus of the pandemic is in Latin America, and there is still no effective treatment or vaccination which would predict a return to life as we knew it. Likewise, the possibility of new outbreaks has been theorized, which would lead to it becoming an endemic disease; therefore, it is important to determine long-term strategies to give continuity to medical education programs. The objective of this study was to systematically review the literature to determine which strategies have been implemented by medical education institutions during the current SARS-CoV2 pandemic to maintain their training activities.
Methods
A systematic review of the literature was performed. Articles with titles or abstracts containing educational strategies during the SARS-CoV2 pandemic were included, with no restrictions regarding the type of research. Articles which during the full text review were found not to contain clear and implementable strategies were excluded.
Data sources and search strategy
The search was performed on the MEDLINE, Taylor and Francis, Lilacs, ERIC, EMBASE, SAGE, SCOPUS and SPRINGER databases using the key words: ('medical education'/exp OR 'medical education') AND ('coronaviridae'/exp OR 'coronaviridae' OR 'covid 19'/exp OR 'covid 19' OR 'sars-related coronavirus'/exp OR 'sars-related coronavirus') for articles published from 2010 through May 2020 in English, Spanish, French, and Portuguese. A search was also performed on the Google Scholar platform, the MedEdPublish platform 15, and in the tables of contents of the five main medical education journals, according to the Scimago ranking 16.
Study selection and data extraction
No specific type of article was established, since the research question is not related to a specific research method. The author was responsible for selecting the studies and extracting the data. Since a large number of opinion articles was expected, conducting a meta-analysis was not considered. The information was divided into undergraduate and graduate study strategies. The search was performed by the author.
The author first reviewed the titles found in the search to determine their relationship with the topic. The following data was extracted from each article: date of publication, type of article, journal, country of correspondence, level of training being addressed, main topic and type of strategies described (administrative, curricular, didactic, clinical rotation, professionalism and mental health) (Table 1).
Table 1 Strategy categories.
| Name | Description |
|---|---|
| Administrative | Development of policies, administrative or professional organization. |
| Curriculum | Adjustments to study plans, changes in teaching modalities, learning models |
| Didactic | Strategies used to present the the curriculum to the students |
| Clinical rotations | Direct adjustments in the clinical practice sites |
| Professionalism | Aspects related to ethics or the behavior of teachers and students during the pandemic |
| Mental health | Aspects related to psychological wellbeing or the prevention and detection of mental health problems |
| Others | Those not included in the previous categories |
Risk of bias assessment
For editorials, commentaries and correspondence, a risk of bias assessment was not performed, as these publications are considered to have a high risk of bias. The quality of analytical studies was evaluated using the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies17.
The information was collated in a Google Sheets® database, and frequencies for each of the previously defined variables were determined. The report was carried out according to the PRISMA guidelines 18. Being a secondary data source study, review by a research ethics committee was not considered. The author was responsible for developing the protocol, collecting the data, and drafting the final manuscript.
Results
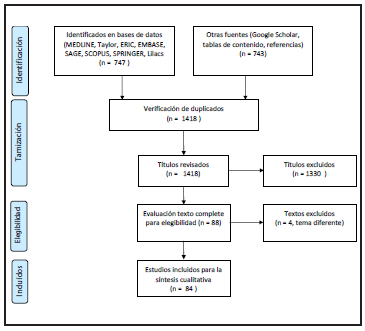
The literature search yielded 1,490 articles (Figure 1). Of these articles, 1,418 (95%) were reviewed, of which 1,330 were excluded after reading the titles and abstracts, and four after the full text review. Eighty-four articles were part of the final qualitative review.
Study description
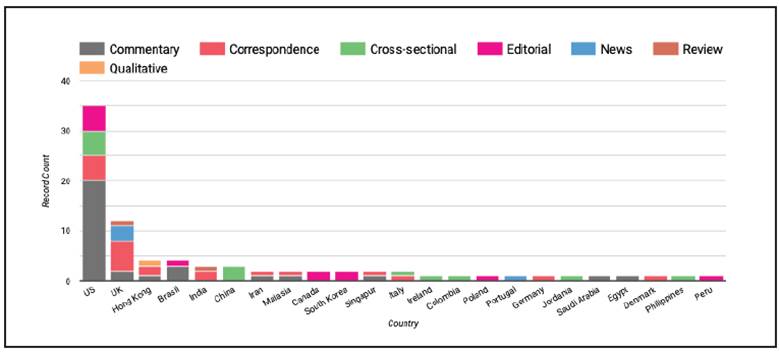
Most of the studies were commentaries (n=31), followed by letters to the editor (n=22). The country which has produced the most articles is the United States (n=35), followed by the United Kingdom (n=13). Five articles (5%) were written in developing countries and six were written on the American continent, outside of the United States (Figure 2). In addition, 57 (67.8%) focused on undergraduate training (medicine, nursing and dentistry), 22 on medical residencies (n=7 medical residencies, n=13 surgical residencies, n=2 medical-surgical residencies), and three on both.
The most frequent category was didactic (n=26; 29.5%), followed by administrative (n=24; 27.2%) and curricular (n=13; 14.7%) strategies. Only five articles were specifically devoted to clinical rotations (Table 2).
Pandemic challenges
The difficulties found in the different countries are similar and include: limitations of gatherings of more than 10 people, restrictions for clinical rotations in various practice sites due to the risk of contagion, the development of electives, the cancellation of office visits, the lack of personal protective elements 19, transportation of foreign students 5, and the institution's decision to only maintain essential personnel in the hospital clinical rotations 20,21.
As a consequence, for example, in Italy, the urology residency had a 41% reduction in shifts, 81% reduction in ambulatory procedures, 75% in diagnostic aids and 62% in endoscopic surgery, with a greater impact on those in their final years of residency 22.
Furthermore, delays are reported in medical school final exams, as well as in the selection processes for new residents 23.
Didactic strategies
The didactic strategies described were: flipped classroom 24-26, videoconferencing 27-29 or asynchronous MOOC classes (7-8 minutes by video) 30, the use of social networks 31, podcasts 26, the use of 3D cadaveric and non-cadaveric models 32,33, scheduling of interinstitutional meetings (34), simulation scenarios outside of the hospital 35 including at home 31,36, high definition surgery or consult videos 20,37, the creation of take-home laparoscopic simulators with videoconference supervision 31,36, asynchronous contacts through forums 38, collaborative work with students from other healthcare programs 24, and the development of multi-campus asynchronous platforms 36,39,40.
Amir describes the performance of virtual rounds, a space in which interactive cases are presented once a week with synchronous discussion at the end of the case 41.
Administrative strategies
The ACGME recommends five principles for administrative adjustments during the pandemic: 1) effective communication 42, 2) intercommunication between medical education-related systems, 3) competency-based assessment, 4) confidence in the system, and 5) the development of new ways of seeing the world 43. For this, a centralized governance system must be established 44 with a tolerance for uncertainty and flexibility, as the situation develops, preserving the chain of command and control 45. This governmental body should maintain open communication channels to provide information on the status of the pandemic in the institution and the practice sites 44,46.
For intern training, protocols for their roles are described, including low-risk activities such as: administrative components, care of patients without respiratory symptoms or outpatients with a low risk of contagion, and their use only as a third line for caring for infected patients, if necessary, or through remote monitoring 47,48. This also includes the development of public health and crisis management skills 49, for example, the creation of epidemiological bulletins 50, community education or care for suspect patients through call centers 51.
In terms of assessment, the following strategies were found: canceling exams or giving them through Information and Communication Technologies (ICTs) or a mixed modality 32, rescheduling final exams, using prior averages and canceling final exams, identifying signs on video, remote open book exams 21 and adjustments to the procedure requirements for graduation, according to the past competency assessments of the program director, in the case of residencies 11,31,52.
For new resident selection, the interview processes migrated to a virtual modality 53, as did the quality verification visits to the clinical practice sites 47.
Finally, there were recommendations such as using Kotter crisis management models to determine program adjustments 34 and scheduling large scientific congresses using a mixed modality (on-site and virtual) 54.
Curriculum strategies
With regard to study plan adjustments and the use of previously described didactic strategies, the following was found: reinforcement of autonomous and adaptive learning 25, fostering home research activities (data collection, writing articles, designing protocols) 31,45,55,56, dividing video classes into small units of time (7-8 min.) 24,57, and accelerating national interinstitutional work on developing unified curricula 53. An on-site modality is proposed only for laboratories, small group discussions, simulation exercises and clinical rotations 58.
One strategy for social distancing was to divide the curriculum and students into two groups (on-site and virtual) to serve as a back-up in case of illness 45,59, with appropriate distribution of academic and clinical loads 55.
These curriculum adjustments seek to develop abilities in teamwork coordination 60, continuous training and self-training 61, guidelines for patients with multiple diseases, and the use of artificial intelligence. They also considered the relationship between the life plan of the educational stakeholders and the needs of the healthcare system, curriculum flexibility, skills adjusted to the needs, 62, effort regulation, results orientation, self-monitoring of the learning process, and help-seeking 63.
Finally, for theoretical content during the pandemic, SARS-CoV2 content was rapidly included in lesson plans 59, as well as simulation strategies for the use of personal protective equipment 35,64, basic mechanical ventilation and nursing care 36
For these curriculum adjustments, Taha et al. 65 proposed an algorithm to guide the process. The steps are: forming work groups, adapting the technology, developing the curriculum, communication and rollout.
Professionalism strategies
The following elements were described on this topic: engaging students in a discussion of the life decision implied in being a doctor, including the responsible exposure to risks to develop their altruism, courage and sense of duty 19; explaining the ethical framework of medical practice during pandemics 50; focusing on developing non-clinical skills (for example, communication skills) and building empathy, among others 66.
Another point was organizing students into crisis response teams with four committees: education for the medical community, education for society, activism to support the clinics and community activism 67.
Finally, it was pointed out that, in light of the decision to graduate some students early, it is important to provide increased support for them to help them improve their skills and professionalism 60.
Mental health strategies
Mental health management is important during lock-down. During the previous SARS crisis, Wong et al. 68 found that 73% of the students had negative emotional responses and above-average stress levels, compared with life events such as separation or unemployment.
The following strategies are described: strengthening student wellbeing services at universities 5, using peer mentors for relaxation techniques and stress management, physical activity, on-line contact with friends and family, and time management, among others 24,69,70; strengthening or implementing mentoring 69, constant assessment of residents' mental health 42, and the use of Schwartz Rounds, as they have proven to stabilize emotions, reduce isolation, provide companionship and compassionate care as well as improve patient care, which could be beneficial during times of healthcare collapse as a result of the pandemic 71.
Clinical rotation strategies
According to the ACGME, practice sites should consider four basic conditions: 1) resources and training in the pandemic, 2) direct supervision of students, 3) observing schedules, and 4) in cases of a second specialty, participating in the first specialty only if necessary (up to 20% of the time) 43.
The most frequently described strategy for practice sites is strengthening telemedicine services and having students participate in these services 26,33,37,56, including clinical rounds (telerounds) 47,72. Other established strategies include: organizing practices emphasizing less frequent procedures or those that are most difficult for residents 52, creating cohort wards for suspect and confirmed patients to which staff in training do not have access 73, conducting virtual tutoring during surgery to reduce the number of people in the operating room 74, not entering the operating room during orotracheal intubation, limiting the use of electrocautery 36, and increasing the number of outpatient clinic hours to avoid congestion 75.
Institutions should be classified in three risk stages according to ACGME (Stage 1: Normal conditions, Stage 2: Increased clinical demand, and Stage 3: Pandemic emergency) and keep their affiliated universities apprised of the situation 42. In conclusion, these strategies seek to ensure safe spaces for both patients and students 44,45,55.
Other strategies
The other strategies described are: mandatory creation of national policies for the pandemic 76, scientific journal adjustments to respond to SARS-CoV2 77, assessment of knowledge on the pandemic 78, adjustments to international congresses 54 and accelerated changes to medical education brought on by the pandemic 6.
Cross-sectional studies
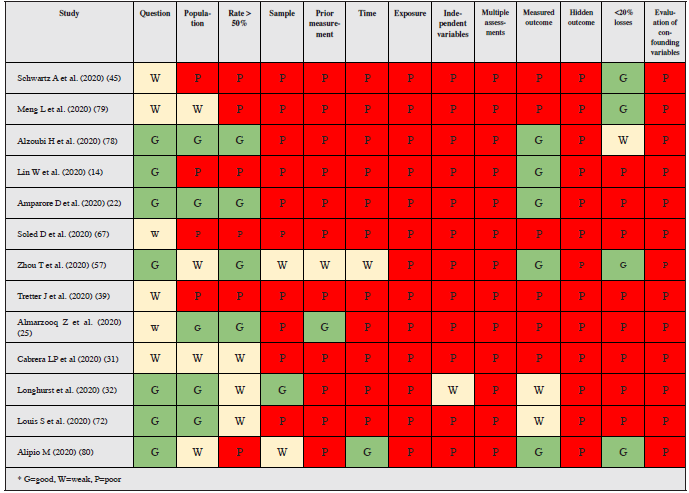
Thirteen studies (15%) were performed using cross-sectional analysis methods (Table 3). An analysis of the studies showed a high risk of bias (Table 4).
Table 3 Summary of cross-sectional studies.
| Date | Authors | Title | Journal | Country | Level | Main topic | Recommendations |
|---|---|---|---|---|---|---|---|
| 2020-03-07 | Schwartz A et al. 45 | Managing Resident Workforce and Education During the COVID-19 Pandemic | The Journal of Bone and Joint Surgery | US | Graduate | Orthopedic residency | Patient and resident safety, providing the necessary care, sustainability of the system, the system's tolerance of uncertainty and flexibility as the situation develops, and preserving the chain of command and control. Establishment of two groups: telework and clinical rotations, two weeks each. Taking advantage of significant cases, given the low volume. Discussing the cases seen after office hours. What is done at home: study, prepare for exams, plan and carry out research, obtain research resources, and make plans for improvement, among others. |
| 2020-03-12 | Meng L et al. 79 | Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral Medicine | Journal of Dental Research | China | Undergraduate | Dentistry | Design of a dental clinic to protect students and teachers. |
| 2020-03-20 | Alzoubi H et al 78 | COVID-19 - Knowledge, Attitude and Practice among Medical and Non-Medical University Students in Jordan | J Pure Appl Microbiol | Jordan | Undergraduate | Knowledge of and attitudes towards the pandemic | Good knowledge, with the primary source being social networks, good adherence to social distancing measures. |
| 2020-04-07 | Lin W et al 28 | Thoughts on Higher Medical Education Under Major Public Health Emergencies: Thinking Ahead After COVID-19 Outbreak | medRxiv | China | Undergraduate | Subject continuity | The use of 5G networks to guarantee connectivity during lectures throughout the pandemic. |
| 2020-04-07 | Amparore D et al 22 | Impact of the COVID-19 pandemic on Urology Residency Training in Italy | Minerva Urologica e Nefrologica | Italy | Undergraduate | Impact on urology residency | A 41% reduction in shifts, 81% ambulatory, 75% diagnostic aids, 62% endoscopic surgery. The greatest impact on more advanced residents. |
| 2020-04-08 | Soled D et al 67 | Medical Student Mobilization During A Crisis: Lessons From A COVID-19 Medical Student Response Team | Academic Medicine | US | Undergraduate | Student organization during the pandemic | A medical student response team with four committees: education for the medical community, education for society, activism to support clinics and activism in the community. |
| 2020-04-09 | Zhou T et al 57 | The Distance Teaching Practice of Combined Mode of Massive Open Online Course Micro-Video for Interns in Emergency Department During the COVID-19 Epidemic Period | Telemedicine and e-Health | China | Undergraduate | MOOCs vs. traditional learning | No theoretical or practical differences, greater satisfaction with MOOCs. |
| 2020-04-13 | Tretter J et al 39 | Heart University: a new online educational forum in paediatric and adult congenital cardiac care. The future of virtual learning in a post-pandemic world? | Cardiology in the Youth | US | Graduate | Pediatric cardiology residency | Description of an open access web platform. |
| 2020-04-15 | Almarzooq Z et al. 25 | Virtual Learning during the COVID-19 Pandemic: A Disruptive Technology in Graduate Medical Education | Journal of the American College of Cardiology | US | Graduate | Didactic methods in cardiology during residency | Student-centered learning, adaptive learning with real situations and feedback, flipped classroom. |
| 2020-04-17 | Cabrera LP et al 31 | Adaptación de la residencia de Cirugía General en Colombia a la pandemia del COVID-19: programa de enseñanza quirúrgica virtual | Revista Colombiana de Cirugía | Colombia | Graduate | Virtual general surgery residency | Lectures and case discussions using ICTs; low-fidelity, homemade simulations for surgery with videoconference tutoring. |
| 2020-04-19 | Longhurst et al. 32 | Strength, Weakness, Opportunity, Threat (SWOT) Analysis of the Adaptations to Anatomical Education in the United Kingdom and Republic of Ireland in Response to the COVID-19 Pandemic. | Medical education | Ireland | Undergraduate | Anatomy | SWOT analysis of ICT-supported anatomy teaching. |
| 2020-04-20 | Louis S et al 72 | Designing Virtual Medical Student Ambulatory Rotations in Light of the Coronavirus Pandemic: A Pilot Project | ResearchGate | US | Undergraduate | Virtual clinical rounds | The design of a telemedicine system which includes students. Two types: students alone and teacher-student participation. |
| 2020-04-25 | Alipio M 80 | Education during COVID-19 era: Are learners in a less-economically developed country ready for e-learning? | SSRN | Phillipines | Undergraduate | Availability of resources for virtual education | Most (54%) lower-middle class people do not have equipment for virtual education. |
Limitations in carrying out strategies
The authors found the following difficulties in carrying out their strategies: connectivity and bandwidth, the quality of transmitted images, inability to carry out laboratory sessions 75, teacher training 20, lack of a teacher-student relationship, limited resources, student motivation 32, poor adherence to asynchronous measures (virtual forums) 24, and a negative perception of goal achievement 81. According to the study in the Philippines, 54% of students have trouble switching to a virtual training modality 80.
As far as professionalism, student participation may increase the use of personal protective items. In addition, students have neither sufficient training nor the obligation to expose themselves to risk, and may only do so for fear of reprisals 19. In this regard, Kam found that nursing students are not willing to expose themselves to risk for others nor to share their personal protective items 73.
Medium-term risks
The following risks are identified in the long term: affected anatomy practices due to decreased cadaver donation 82 and decreased student participation; financial stress for hospitals brought on by the pandemic due to decreased income as a result of closed ambulatory services, decreased consults from noninfected patients due to fear, and increased expenses to acquire personal protective equipment and mechanical ventilators, at higher costs 83; and a potentially reduced employability rate for graduates due to decreased demand in many services 59.
Discussion
This systematic review shows that multiple strategies have been rolled out in a short period of time to adjust medical education to the pandemic. The strategies are mainly aimed at didactic and administrative activities. However, most of these studies are expert opinions and of the 13 analytical studies found, none had a good methodological quality which would allow solid conclusions to be drawn.
The current scenario requires that we weigh the information and deepen our understanding of the impact of the crisis and how we have been training since before the crisis so as not to waste this time 84, maintaining academic rigor and healthcare quality 44. The real impact of the pandemic on undergraduate and graduate training must be determined rapidly to identify which of the implemented strategies were successful 85. This is undoubtedly a priceless opportunity to accelerate the changes in medical education which have been wanted for years 6.
Although bimodal education is usually implemented after considered planning, in collaboration with others and taking existing evidence into account, at this point it is imperative that these processes be accelerated, and teachers and students strengthened in the appropriate use of ICTs 32.
This is not the time to continue the Byzantine discussion of which of the two strategies is better; curricular content should be distributed between them according to the goals being sought. Bimodal education is superior to traditional and virtual modalities separately. For example, considering the average time it takes to develop symptoms, the strategy of dividing into groups to work virtually and on-site for two-week periods facilitates social isolation in case of infection.
Undoubtedly, the uncertainty of this situation triggers the flight instinct in each of us, but this can be overcome with character, education and training. This is the time to teach future generations professionalism and how to take advantage of crises, through our example 19. While many of the strategies found could be considered hasty and disadvantageous, it must be acknowledged that they will need to be implemented long term and will be the new post-pandemic normal.
Strengths and limitations
Despite having carried out an exhaustive search of the literature and a careful selection and quality evaluation of the studies, the findings presented have a few limitations. Most of the reviewed studies were editorials or letters to the editor, and therefore the quality of evidence is low. However, it is understandable that studies with greater methodological rigor cannot be carried out during the pandemic. Another limitation is that the articles were reviewed by a single author, and thus important elements may have been left out in the search. To decrease this risk, the titles found were reviewed twice and other data sources were also searched, including the tables of contents of the highest-impact journals in medical education.
Future research
This review identifies gaps which are very important to resolve in the short term such as: What is the best strategy for expedited implementation of bimodal education? What is the minimum on-site exposure that should be guaranteed for students during their training? How will the didactic strategies recorded during the pandemic be updated? What is the long-term impact of the accelerated changes implemented during the current crisis? How much time is required in a virtual or simulated modality to cover the on-site contents? What is the role of the clinical instructor in this new scenario? 86. Observational, qualitative and pre-post quasi-experimental cohort studies could provide answers to some of these questions.
In conclusion, the medical education world has rapidly adjusted to the pandemic through the implementation of various sequential bimodal didactic strategies (on-site/ virtual) and the strengthening of telemedicine within the framework of professionalism and mental health protection of both teachers and students.











 texto em
texto em