Introduction
Atrial fibrillation (AF) is a complex arrhythmia characterized by a regular R-R interval with no P waves on the electrocardiogram, or lasting more than 30 seconds on other types of registers, in which atrial activity has a cycle length of less than 200 ms between f waves 1. Depending on the clinical presentation, it can be classified as: 1) first episode AF, which has been defined as the first symptomatic debut of the arrhythmia; 2) paroxysmal AF, which is when atrial fibrillation resolves spontaneously or as a result of medical intervention: 3) persistent AF, characterized by the episode lasting more than seven days, ending with electrical or pharmacological cardioversion; 4) very persistent AF, when it lasts form more than one year and frequency control has been considered; and 5) permanent AF, when the decision agreed upon with the patient is to maintain atrial fibrillation and the therapeutic goal is to control the heart rate 2. Valvular AF is a term reserved for the presence of mechanical valves and moderate to severe mitral Cerebrovascular accident risk stratification has been evaluated in diverse scenarios using different scales, with the CHA2DS2-VASc score being the most accepted for non-valvular atrial fibrillation.
Can a CHA2DS2-VASc score of 0 or 1 really rule out the risk of an ischemic cerebrovascular accident?
Clinical case
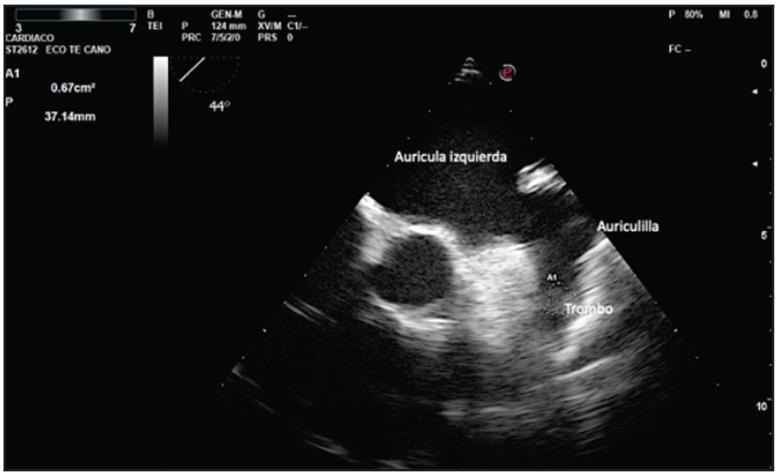
This was a male 64-year-old patient with a family history of atrial fibrillation (two brothers, one having a dual chamber pacemaker). He had a history of arterial hypertension, mild sleep apnea-hypopnea syndrome (apnea index: 12 per hour) and was diagnosed with atrial fibrillation after an immersion in the ocean. Extension studies documented left atrial dilation with a volume of 67 mL/m2, and a "chicken-wing" left atrial appendage. Successful synchronous electrical cardioversion was performed (Figure 1), with subsequent event monitor implantation (Medtronic Reveal LINQ). He remained on amiodarone 200 mg/day, metoprolol succinate 50 mg/day and rivaroxaban 20 mg/day for one year with no atrial fibrillation recorded.
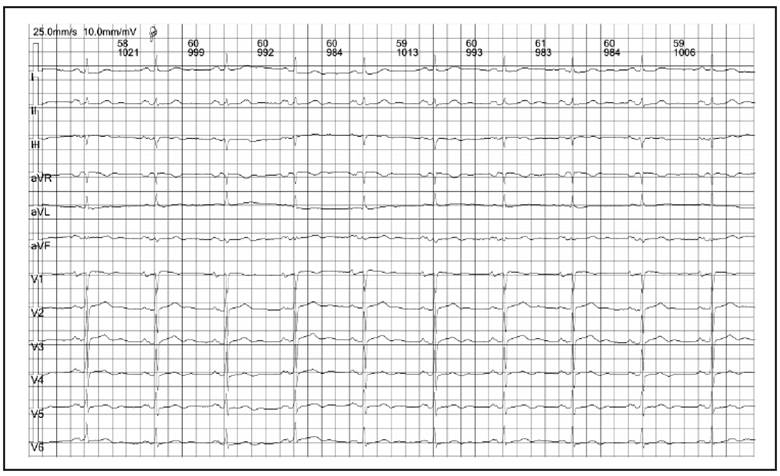
Figure 1 Electrocardiogram with sinus rhythm after electrical cardioversion, where left atrial growth and left antero-superior hemiblock can be seen.
Echocardiograms performed during follow up showed reverse remodeling of the left atrium with a normalized diameter and volume. With an embolic risk of 1 according to the CHA2DS2-VASc scale and a lack of symptoms, the decision was made, with the patient, to discontinue the anti-arrhythmia medication and anticoagulant. He was managed with ASA 100 mg/day, and metoprolol succinate 50 mg/day. After eight months of implanted events monitor interrogation (during the SARS 2 COVID pandemic), he consulted due to the sudden onset of right hemiparesia and aphasia while he was at work. Severe arterial hypertension was found on admission to the emergency room, along with an acute ischemic cerebrovascular accident in the upper and lower branches of the bilateral middle and right anterior cerebral arteries, with signs of hemorrhagic transformation on nuclear magnetic resonance imaging of the brain (Figure 2). Implantable events monitor interrogation showed an increased atrial fibrillation load in the 15 days prior to the ischemic event (Figure 3). A transesophageal echocardiogram was performed 48 hours after the event, which showed a thrombus in the left atrial appendage (Figure 4). Complementary studies showed no carotid disease or positive serology for prothrombotic diseases, including SARS COVID 2 infection.
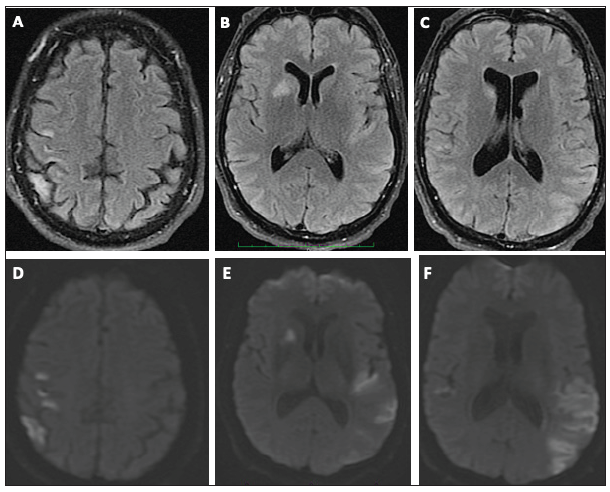
Figure 2 Cerebral magnetic resonance with contrast. A, B and C correspond to flair sequences; D, E and F correspond to diffusion sequences. Multiple circulation and terminal and bilateral basal ganglia infarcts can be seen in various stages of development.
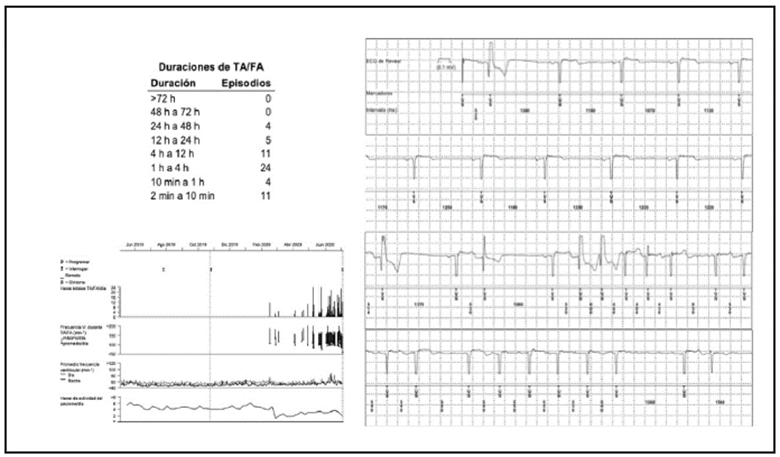
Figure 3 Heart rate histogram taken from the Reveal LINQ Medtronic implantable events monitor showing episodes of paroxysmal atrial fibrillation lasting up to 48 hours, with an increase in episodes in the 15 days prior to the event. The beginning of an atrial fibrillation episode is also shown.
Discussion
This clinical case questions the usefulness of the CHA2DS2-VASc risk scale for ischemic cerebrovascular accidents when the score is 0 or 1: Is CHA2DS2-VASc a useful tool in men with scores of 0 and 1?
The use of statistical models based on risk factors has changed over the last few years with the establishment of the CHA2DS2-VASc scale as a more accurate model than the rest, allowing the one-year risk of ischemic cerebrovascular accident to be determined using clinical information 4. The acronym establishes a score between 0-9 points, in which heart failure (left ventricular dysfunction with an ejection fraction <40%) is worth one point, arterial hypertension: one point, age > 75 years: two points, diabetes mellitus: one point, a history of a transient ischemic cerebrovascular accident or thromboembolism: two points, a history of vascular disease (prior myocardial infarction, peripheral artery disease or aortic atheromatous plaques): one point, age 65-74 years: one point, and female sex: one point. The sum of the points estimates the one-year risk of an ischemic cerebrovascular accident, from a score of two with an annual risk of 2.2%, to a score of nine, with an annual risk of 15.2% 4.
The therapeutic use of the CHA2DS2-VASc score has changed over time, and today, the indication for beginning anticoagulation is accepted to be a score of two or more in men and three or more in women 5. However, factors like the type of atrial fibrillation are not included in the CVA risk assessment scales; the evidence establishes that the risk of ischemic CVA in paroxysmal atrial fibrillation is lower than in permanent atrial fibrillation and the same as that of silent atrial fibrillation 6. The greatest limitations of the CHA2DS2-VASc score are: 1) it does not distinguish between the types of atrial fibrillation; 2) it does not consider aspects related to CVA such as the form of the left atrial appendage and the volume of the left atrium; and 3) it does not take specific ethnic groups into account in assigning the risk of CVA 7.
In patients with a CHA2DS2-VASc score of one, the recommendation is to not anti-coagulate 5; however, ischemic CVAs have been reported in patients with a CHA2DS2-VASc score of one. A meta-analysis which included reports of patients with a CHA2DS2-VASc score of one, but which methodologically had a high heterogeneity index in the analyzed reports, concluded that the decision to use anticoagulation in patients with a CHA2DS2-VASc score of one should be made individually and agreed on with the patients 8.
Patients with cardiac stimulation devices or implantable event recorders, like the one reported in this article, meet the inclusion criteria for the ATRESIA study which is closing in on an answer regarding the use of anticoagulation in asymptomatic patients with atrial fibrillation who have stimulation devices and implantable event monitors; results are expected in 2022 9.
Another type of scenario is that of high-performance athletes in whom cerebrovascular accidents have been reported with CHA2DS2-VASc scores of 0, setting out another topic of discussion related to a disease known as athletic cardiomyopathy 10.
Cerebrovascular accidents are increasingly prevalent, probably due to population aging. It is estimated that there are 610,000 new cases per year in the United States, causing one of every 19 deaths; most of these cases are ischemic cerebrovascular events 7.
The pathophysiology of cardioembolic cerebro-cardiovascular events, 90% of which have concomitant atrial fibrillation, is considered to be the result of the interaction of three factors known as Virchow's triad: increased blood stasis in the left atrial appendage, and the endothelial damage and hypercoagulability needed for thrombus formation 7. There are also non-cardioembolic factors related to ischemic CVA in patients with atrial fibrillation such as: intracranial arterial stenosis, significant carotid stenosis, and complex aortic plaques 11. The body's ability to maintain endothelial vascular integrity against the biological susceptibility to thrombosis, is the result of several local and cellular signaling pathways which may protect against or increase the risk of ischemic CVA 12. In patients with no risk factors and ischemic CVA, increased levels of prothrombin 1 and 2 fragments and P-selectin have been found, as well as increased levels of coagulation factor VIII, von Willebrand factor, platelet factor 4, and B-thrombomodulin, as well as fibrinolysis markers such as D-dimer 13.
Other nontraditional risk factors include: sleep apnea, which is thought to be an independent factor for ischemic CVA even when atrial fibrillation has not been proven in CVA patients 14; the presence of kidney failure, with a direct relationship between a fall in creatinine clearance and increased prevalence of ischemic CVA 7; elevated levels of brain natriuretic peptide (BNP), not only found in patients with ischemic CVA, but also correlated with prolonged hospital stay 15; and specific ethnic groups. Other important risk factors reported are: left atrial dilation, spontaneous echo contrast and a high calcium score on coronary tomography 7.
It should also be considered that atrial fibrillation may be a sign of atrial myopathy. While the presence of atrial fibrillation may be a marker for dilated cardiomyopathy in some cases, in other cases there is only non-valvular atrial fibrillation, and this could be an atrial disease finding 16. Atrial cardiomyopathy markers have been proposed such as: atrial dilation, spontaneous echocardiographic contrast, decreased flow velocity in the left atrial appendage, supra-ventricular tachycardia, increased terminal strength of the P wave in V1 on the electrocardiogram, inter-atrial block, Bayés syndrome, prolonged PR interval, atrial fibrosis documented on cardiac magnetic resonance 16, and left ventricular growth determined by electrocardiography or echocardiography 17.
In patients with atrial fibrillation, the morphology of the left atrial appendage is a risk factor for developing ischemic CVA. The most common morphology is the chicken wing in up to 48%, cactus in 30%, windsock in 19%, and cauliflower in 3%. It was also shown that not having a chicken wing morphology is a risk factor for ischemic CVA; cactus and windsock morphologies, especially, are a risk factor for ischemic CVA 18.
Serological markers like high levels of T-troponin and N-terminal brain natriuretic peptide (pro BNP) in patients with AF have been related to the outcome of ischemic CVA 12.
It was retrospectively estimated that 75% of patients with ischemic CVA had some factor that could have been prevented to avoid the event, which suggests that there is a gap in prevention in patients assessed using the CHA2DS2-VASc scale, according to the study by Dr. Fisher et al. 19.
Risk factors other than those supplied by the CHA2DS2-VASc scale should be considered. However, the risk-benefit ratio must be weighed consensually with the patient, given the importance of the adverse effects caused by anticoagulants. In conclusion, the CHA2DS2-VASc score is the currently used tool, and its use should be adopted in patients with atrial fibrillation, as it estimates the one-year probability of ischemic CVA in non-valvular atrial fibrillation, with scientific support for determining whether to begin anticoagulation in the office.











 texto em
texto em