Introduction
Acute interstitial nephritis is a kidney disease whose existence is rarely thought of, despite its high incidence. The chronic granulomatous form is a rare entity and accounts for only 0.5-0.9% of kidney biopsy findings. It has a broad etiology and has been associated with various medications such as antibiotics and NSAIDs, and infectious diseases like tuberculosis and fungi, as well as polyangiitis and sarcoidosis 1. We describe the case of a patient with rheumatoid arthritis who began biological treatment (adalimumab) and developed progressive and marked deterioration in renal function which self-limited when the medication was stopped, other possible diagnoses being ruled out by clinical and imaging findings.
Case presentation
A 56-year-old female patient with a five-year history of seropositive rheumatoid arthritis and chronic arterial hypertension was sent to nephrology for consultation due to deteriorating renal function, with a gradual and sustained increase in creatinine, going from 1.02 mg/dL to 2.3 mg/dL in the space of nine months (Table 1). She had no significant clinical signs or macroscopic abnormalities on the urine exam. Mild normocytic anemia was detected in other studies. The urinalysis showed no proteins, and there were no cell abnormalities in the urine sediment (Table 2).
Table 1 Creatinine levels throughout the clinical course.
| Date | 4/23/2016 | 5/30/2017 | 8/25/2017 | 12/12/2017 | 2/12/2018 | 3/28/2018 | 5/19/2018 |
|---|---|---|---|---|---|---|---|
| Creatinine (mg/dL) | 0.5 | 1.02 | 1.25 | 1.61 | 2.3 | 2.11 | 2.03 |
| Date | 8/17/2018 | 9/5/2018 | 1/25/2019 | 4/12/2019 | 2/17/2020 | 7/17/2020 | 9/21/2020 |
| Creatinine (mg/dL) | 3 | 2.6 | 2.19 | 2.2 | 1.97 | 1.86 | 1.9 |
Table 2 Other tests.
| Potassium mmol/L | 4.4 |
| Uric acid (mg/dL) | 5.7 |
| Total serum calcium (mg/dL) | 9.8 |
| Albumin gr/dL | 4.2 |
| Anti-HCV | Negative |
| HBsAg | 0.5 |
| HIV Elisa | 0.31 (negative) |
| ANA | 1 in 80 |
| C3 | 133 |
| C4 | 30 |
| 24-hour urine protein (mg) | 156.3 |
| 24-hour urine calcium (mg) | 66 |
| Urine test | |
| Urinalysis | Density: 1.010, pH: 6.0, Protein: negative, Blood: negative, Leukocytes: negative |
| Urine sediment | Leukocytes: not found, Erythrocytes: not found, Epithelial cells: 1-3 HPF, Bacteria: not found |
| PPD (tuberculin) | Zero mm (negative) |
| PPD (tuberculin) | Zero mm (negative) |
| Urine AAFB | Negative |
A kidney ultrasound was ordered which reported kidneys of a normal size and appearance, with adequate cortico-medullary differentiation and no evidence of urinary tract obstruction. A renal artery Doppler showed no abnormalities which would suggest renal artery stenosis. A percutaneous renal biopsy was ordered, but the procedure was only authorized and performed three months after the order by nephrology.
The result was: 65 glomeruli present, 29 with global sclerosis, 2 with segmental sclerosis, and no proliferative glomerular changes. There was ++++ (100%) mononuclear tubulointerstitial inflammation with histiocytes and granulomas, negative staining for acid-alcohol-fast bacilli, +++ (100%) interstitial fibrosis, +++ (100%) tubular atrophy, normal blood vessels, negative immunofluorescence for deposits, and interstitial mononuclear cells on electron microscopy, with a diagnosis of chronic granulomatous interstitial nephritis (Figure 1). Granulomatous conditions such as tuberculosis and sarcoidosis were ruled out through complementary studies and clinical and imaging findings.
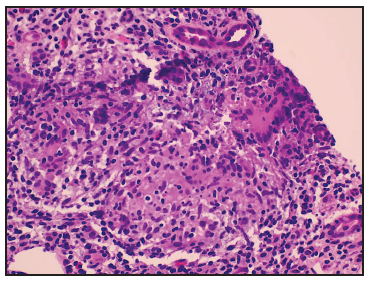
Figure 1 Hematoxylin and eosin 20x. Presence of inflammatory interstitial infiltrate with a tendency to form granulomas, consisting of histiocytoid and longitudinal cells.
The patient's medical history and current list of medications were carefully reviewed: leflunomide, prednisolone, amlodipine, losartan, hydrochlorothiazide, ranitidine and adalimumab 40 mg subcutaneously every 15 days, the latter for the last 12 months. She had been treated for the last three years with chloroquine and methotrexate. A relationship was found between kidney function deterioration and the initiation of biological therapy (adalimumab). With the histological diagnosis, it was decided to discontinue adalimumab and leflunomide, and begin treatment with prednisone 0.5 mg/kg/day and cyclophosphamide 1 mg/kg/ day for six months, after which the patient continued with azathioprine alone, which she continues to take today. The kidney function stopped deteriorating when adalimumab was discontinued.
Discussion
Interstitial nephritis is an injury pattern that may develop due to many etiologies. The term "chronic" is used for some of the various entities which begin acutely, but with persistent exposure to the causative agent, develop into interstitial lymphoplasmacytic infiltrate associated with interstitial fibrosis and tubular atrophy, with glomerular sclerosis in more advanced stages 2. The presence of granulomas is an even rarer pattern of injury, and knowledge of its etiology is derived from case series reports in which the main causes have been drugs, granulomatosis with polyangiitis, sarcoidosis and tuberculosis, with varying frequency according to the study and area in which it was performed 3,4.
The treatment of autoinflammatory diseases has advanced greatly in the last few years. Biological therapy plays a very important role within the so-called disease-modifying anti-rheumatic drugs (DMARDs) 5. The introduction of medications such as tumor necrosis factor antagonists is accompanied by subsequent reports, after several years of follow up, of unusual adverse reactions. Over the last few years, reports have been made of the appearance of noninfectious, noncaseating granulomas on renal or lymph node biopsies of patients receiving medications like adalimumab and etanercept, in whom clinical improvement was seen after suspending the medication and introducing immuno-modulatory therapy like steroids, similar to what occurred with our patient 6.
One of the main differential diagnoses in this clinical case would be sarcoidosis with renal involvement. In this entity, the classic kidney lesion described is noncaseating granulomatous interstitial nephritis associated with hypercalciuria, hypercalcemia, nephrocalcinosis and nephrolithiasis, with frequent involvement of other organs such as the lungs and skin 7. A high-resolution lung tomography was ordered for this patient, and no lesions suggestive of sarcoidosis were found. The serum calcium and 24-hour urine calcium were reported as normal (Table 2).
Tubercular granulomatous infections were also ruled out, given the histological pattern (noncaseating granulomas), negative staining for acid-alcohol-fast bacilli (AAFB) and negative tuberculin test, together with a lack of symptoms (Table 2).
There are few reported cases documenting a direct relationship between adalimumab and granulomatous interstitial nephritis. Sandys et al. reported two cases in which, after beginning treatment with this medication, there was a gradual and sustained increase in creatinine levels over a period of approximately 10 months, which stabilized and began to descend after discontinuing the anti TNF 8. In the last few years, sarcoidosis-like inflammatory phenomena have been reported secondary to the use of anti TNF medications, with all cases having noninfectious and noncaseating granulomas on lymph node or kidney biopsies, which suggests that it may be a class effect, since the effect has been described with drugs like etanercept, infliximab and adalimumab 6. The coexistence of sarcoidosis and rheumatoid arthritis is thought to be extremely rare. The occurrence of a sarcoidosis-like phenomenon with the use of biological therapy is a paradoxical effect, since this type of treatment has been successfully used in case series for the management of sarcoidosis. However, there is biological plausibility given the temporal relationship between the introduction of TNF-a antagonists and the appearance of granulomatosis, with subsequent improvement in the inflammatory pattern after discontinuing the TNF-a antagonists, and clinical relapse of the granulomatosis with a rechallenge using the same TNF-a antagonist 9.
In our patient, the delay between ordering and performing the kidney biopsy (three months) undoubtedly explains the histological findings of fibrosis and tubular atrophy, which may have impacted on the incomplete response to immunosuppressant therapy. Supporting this, Fernández-Juárez et al. reported that acute interstitial nephritis treatment only produces satisfactory results if it is begun early, before there are fibrotic changes 10.
Our recommendation is that, in patients with RA who develop renal function deterioration and are on biological treatment, especially anti TNF, drug-induced interstitial nephritis be included in the differential diagnosis, and that this be confirmed as quickly as possible by renal biopsy and the recommended treatment started, beginning with the immediate suspension of the anti TNF.











 text in
text in 


