Introduction
Remote intracranial bleeding is a rare but potentially fatal complication related to cerebrospinal fluid (CSF) drainage.
During spinal surgery, a durotomy must be performed to remove intradural lesions. Likewise, dural tears may occur accidentally.
Remote intracerebral bleeding may occur secondary to a CSF leak related to spinal surgery 1. The exact etiology of remote intracerebral bleeding is still not entirely clear, but it has been suggested that it is caused by excessive CSF loss which leads to cerebral dehydration, causing stretching and, ultimately, rupture of the bridging vein. On the other hand, the constant drainage and suction at the dural repair site has been associated with sustained cerebral hypotension, fostering an environment conducive to the formation of a subdural hematoma 2,3.
Different studies place the incidence of intracerebral bleeding after spinal surgery between 0.4 and 1.7% 4,5.
In this article, we describe the case of an acute subdural hematoma following the resection of a neurofibroma, with no intraoperative report of cerebrospinal fluid leaks.
Case presentation
A 32-year-old male patient with a history of neurofibromatosis and spastic quadriparesis was admitted to a tertiary care hospital in the city of Pereira, Risaralda, for the scheduled resection of a left intradural extramedullary tumor, possibly a neurofibroma, at L5. A laminectomy and foraminotomy were performed to remove the tumor, with no evident complications during the procedure, and therefore the patient was transferred to the recovery room where he was extubated as scheduled. After approximately two hours, the patient began to show a marked deterioration in his level of consciousness, Glasgow 4/15, along with right anisocoria. A simple computerized axial tomography of the head showed an acute subdural hematoma in the right hemisphere, with a midline shift and signs of uncal herniation (Figure 1). He was once again taken to surgery for subdural hematoma drainage by craniotomy, and meningeal vessel occlusion. He was transferred to the intensive care unit immediately after surgery and there experienced a tonic-clonic seizure of the right side of the body, requiring benzodiazepine treatment. A follow up simple CAT of the head showed post-surgical changes (Figure 1). During his stay in the ICU he had a torpid clinical course and progressive deterioration of oxygenation levels with adult acute respiratory distress syndrome (ARDS), requiring neuromuscular relaxation and protective ventilation. After 12 days in the hospital, the patient died.
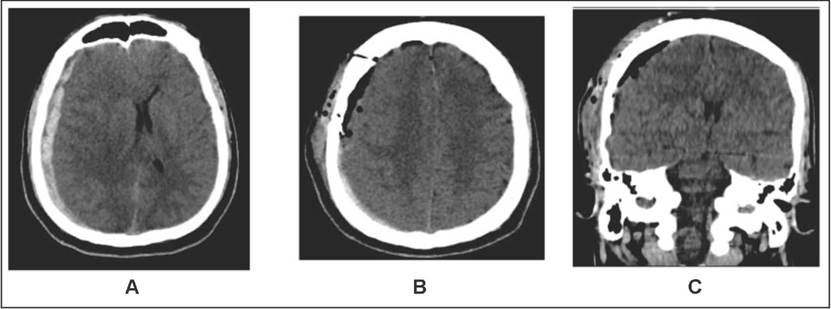
Figure 1 A: An axial section of a simple head CAT immediately after surgical tumor resection; note the subdural hematoma in the right hemisphere, with signs of uncal herniation. B: An axial section of a simple head CAT following craniotomy; postsurgical changes can be seen, with resolution of the subdural hematoma. C: A coronal section of a simple head CAT following craniotomy; postsurgical changes can be seen, with resolution of the subdural hematoma.
Discussion
Remote intracranial hemorrhage (ICH), as has already been mentioned, is a rare complication and is caused by dura mater lesions which lead to cerebrospinal fluid (CSF) leaks. These lesions are usually caused by instrumentation, direct trauma, or even residual bone spicules 2. Early diagnosis, ideally during surgery, could decrease the subsequent associated complications. In the case of our patient, symptoms appeared early with rapid onset neurological deterioration.
However, in other patients, clinical suspicion and a detailed physical exam will be important. It has been reported that a fluctuating subcutaneous collection should lead to a suspicion of cerebrospinal fluid leakage, especially if it grows with increased intramedullary pressure or is accompanied by a postural headache 6.
The etiologies of remote ICH, in addition to the one described in the clinical case, include lumbar puncture, regional anesthesia, ventricular shunt procedures, CSF drainage for aortic aneurysm procedures and spinal cord trauma 7.
Clinically, ICH may present with symptoms, ranging from such nonspecific symptoms as headache, nausea, or vomiting to visual and auditory changes, an altered level of consciousness and even seizures 7.
The location of drainage systems in the surgical site has been one of the variables most commonly associated with ICH following spinal surgery. Another point to keep in mind is the suction systems, which are associated with increased CSF flow through the dura mater, which cannot be completely sealed until the drainage is removed 6. A case series study by Kaloostian et al. found that an average drainage of 221 ml (9.2 ml/h) of serosanguinous fluid was associated with the onset of ICH, even when intraoperative CSF loss was not recorded.
Computerized axial tomography (CAT) provides a diagnostic approach to the etiology of the bleed using characteristic pattern findings. Remote intracranial hemorrhage, for example, is located subcortically, unlike hypertensive cerebral hematomas, which are mostly located close to the dentate nucleus 9.
The treatment of ICH complications depends on its location, its size and the clinical condition of the patient. In patients with a small hemorrhage without significant mass effect and without neurological changes, it may be treated conservatively. On the other hand, patients with a significant hemorrhage and rapid neurological deterioration require surgical treatment to remove the bleed, with or without ventriculostomy implantation to treat the hydrocephaly 3.
Conclusion
Intracranial complications following spinal surgery are rare and require high clinical suspicion to identify and properly treat them. It should always be kept in mind that while they have a low incidence, their complications are potentially fatal, and both the clinician and the spinal surgeon should work together to achieve the best outcome for the patient. Early detection of symptoms and prompt neuroimaging are essential in the diagnostic approach to these patients.











 text in
text in 


