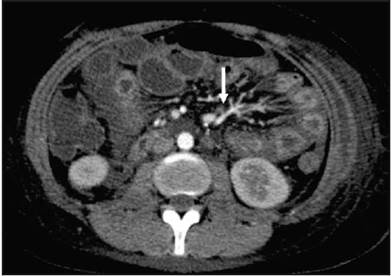
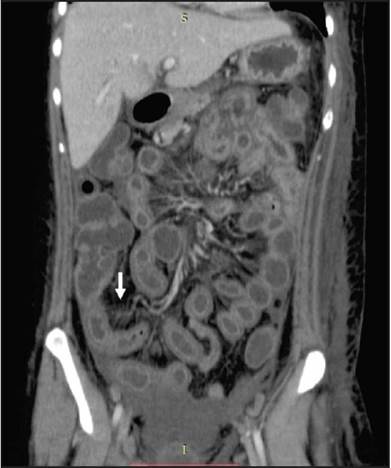
This was a 34-year-old patient with a history of systemic lupus erythematosus diagnosed in 2008, at which time he had hemolytic anemia, arthritis and serositis. Since then, the patient had been in remission, taking only 5 mg of prednisone and 1 mg of folic acid, both once a day. He went to the emergency room for intense abdominal pain along with vomiting and diarrhea. As part of the diagnostic workup, he underwent abdominal tomography with contrast, which is the gold standard for diagnosing lupus enteritis. The tomography showed thickening and abnormal contrast of the vascular wall throughout the intestine (halo sign), an increased number of visible abdominal vessels (comb sign), ascites and pleural effusion. After ruling out other etiologies, methylprednisone pulses were begun with noticeable improvement of the clinical symptoms within six hours.
Abdominal tomography with contrast is the gold standard for diagnosing lupus enteritis. It shows diffuse or focal thickening of the intestinal wall, increased uptake of the intestinal wall (halo sign), mesenteric vessel congestion with a greater number of visible vessels (comb sign), attenuation of mesenteric fat and ascites 1. It is essential to be familiar with the clinical presentation and imaging characteristics for two reasons: first, intestinal diseases like pancreatitis, intestinal obstruction, peritonitis or inflammatory bowel disease may present with similar radiographic findings 2. Second, patients may present with no other markers of SLE activity. Glucocorticoids are the cornerstone for managing these patients, usually with a rapid response 3.











 text in
text in