A 23-year-old man with a history of recurrent sinusitis was admitted for pleuritic pain and fever. His tests showed left empyema, situs inversus, bronchiectasis and sinusitis (Figures 1 and 2). He was diagnosed with Kartagener syndrome, and required antibiotic and surgical treatment for his empyema, with clinical improvement. A nasal ciliary biopsy was compatible with ciliary dyskinesia.
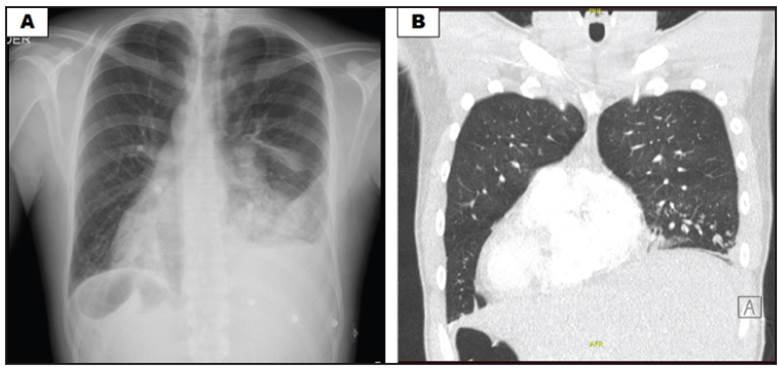
Figure 1 A: anterior-posterior chest x-ray showing alveolar opacity in the left lower lobe, ipsilateral pleural effusion and signs of volume loss with hemidiaphragmatic retraction, dextrocardia and a right-sided gastric chamber. B: chest tomography, coronal plane, showing complete situs inversus: heart and stomach to the right and liver to the left.
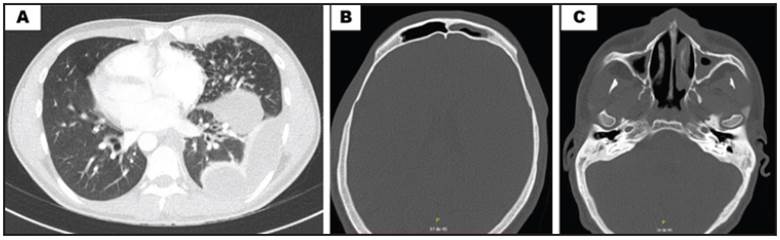
Figure 2 A: chest tomography, axial plane, with left pleural effusion, peribronchial thickening and bilateral bronchiectases, some with a mucous plug. B: paranasal sinus tomography showing frontal sinusitis. C: bilateral ethmoid and maxillary
Kartagener syndrome is an autosomal recessive hereditary disorder, a subset of primary ciliary dyskinesia, characterized by the triad of chronic sinusitis, bronchiectasis and situs inversus1. The recommended diagnostic criteria include a history of chronic bronchial infections and rhinitis since childhood, with one or more of the following: (a) situs inversus or dextrocardia in the patient/ sibling, (b) live but immotile spermatozoa, (c) absent or abnormal tracheobronchial clearance, and (d) a characteristic ciliary ultrastructural defect on electron microscopy 2. Management is multidisciplinary, with physical therapy, antibiotics, vaccinations and lung transplant in advanced disease recommended 1,3.











 text in
text in 


