Introduction
Cardiovascular disease (CVD) continues to be the main cause of death worldwide, and has a significant morbidity burden today, with a high economic impact. Continuous home oxygen therapy (CHOT) is a widely used in patients with chronic pulmonary disease. However, there is scant evidence regarding its indications, benefits and clinical predictors which could affect its requirement in patients with CVD.2
Continuous home oxygen therapy is a longstanding treatment with which there has been much experience. It consists of administering greater oxygen concentrations than those found in room air, in order to treat or prevent the signs and symptoms of hypoxia 1. Hypoxia is defined as a decreased oxygen supply to the tissues, which causes harmful effects on the various body systems. Alveolar hypoxia affects pulmonary circulation, causing increased local pulmonary vascular resistance which will result in pulmonary hypertension and right heart failure. This phenomenon is mediated by blood flow redistribution to pulmonary areas with greater ventilation 2.
The recommendations governing the current guidelines for home oxygen therapy are based on studies of patients with chronic obstructive pulmonary disease (COPD) published in the 80s, which include the Nocturnal Oxygen Therapy Trial (NOTT) and the Medical Research Council (MRC). These studies showed a clear benefit in terms of survival, quality of life and pulmonary hemodynamics in people with COPD and severe resting hypoxemia, defined as a resting partial pressure of oxygen (PaO2) < 60 mmHg at sea level 3,4.
The current indications for CHOT in patients with COPD include a resting PaO2 ≤55 mmHg or a resting PaO2 between 56-59 mmHg and evidence of hypoxic organ damage (pulmonary hypertension, cor pulmonale, or polycythemia), or a resting oxygen saturation (SpO2) <90% 5. The goal of administering supplementary oxygen is to maintain the resting PaO2 above 60 mmHg and resting oxygen saturation above 90% at sea level. Oxygen should be administered for at least 15 hours a day, including during sleep.
Regarding heart disease and CHOT, there are no randomized studies showing improvement in functional class or survival. The indications for CHOT derived from pulmonary patients are generally extrapolated to cardiac patients 10.
Untreatable dyspnea is one of the main reasons for prescribing CHOT in patients with palliative heart failure, even though the studies do not show that it provides any additional benefit 20.
The objective of this study is to describe the patients hospitalized at Fundación Cardioinfantil.
Materials and methods
This was an observational, descriptive, cross-sectional, retrospective study. The study universe was all individuals over the age of 18 hospitalized at Fundación Cardioinfantil from January 1, 2018 to December 31, 2018, with a diagnosis of cardiovascular disease as the main reason for hospitalization and home oxygen ordered for the first time. The definition of cardiovascular disease was based on the one used by the World Health Organization (WHO) in June 2021. It is defined as a group of heart and blood vessel disorders and includes coronary disease, cerebrovascular disease, rheumatic heart disease and other conditions 24. Individuals with a prior prescription for and use of home oxygen, those with orders for home oxygen not recorded in the available data systems, and those whose home oxygen order was cancelled for any reason were excluded.
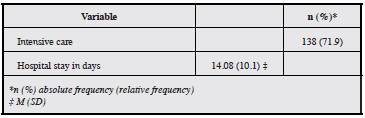
The following variables were reviewed in the medical chart: sociodemographics (age, sex and type of social security), comorbidities, anthropometric variables such as body mass index (BMI), admission vital signs (heart rate, blood pressure and SpO2), lab tests (complete blood count, arterial gases, brain natriuretic peptide [BNP]), imaging tests with left ventricular ejection fraction (LVEF) and pulmonary artery systolic pressure (PASP) calculated by echocardiogram, need for intensive care unit (ICU) treatment and days of hospital stay.
The univariate analysis was carried out using descriptive statistics of the selected population, determining absolute and relative frequencies. Measures of central tendency (mean, median) and dispersion (standard deviation and interquartile range) were calculated for quantitative variables. The database was recorded in Microsoft® 365 MSO Excel®, and the EPIDAT version 4.2 program was used to analyze the variables. Based on Resolution 8430 of 1993, this was considered to be a no-risk study. Permission for the chart review was obtained from the Fundación Cardioinfantil ethics committee in Bogotá, Colombia. The ethical principles of autonomy, beneficence, non-maleficence and data confidentiality established by the Declaration of Helsinki were respected.
Results
Population characteristics
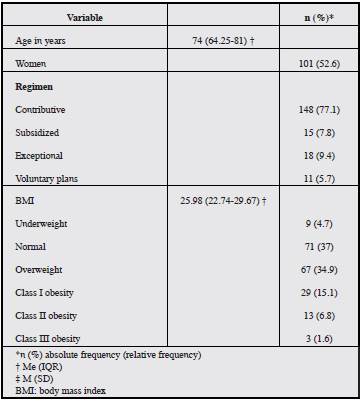
Data were obtained from 192 patients for whom home oxygen was ordered during 2018. The median age was 74 years (IQR: 64.25-81), and 52.6% of the study population were women. Regarding health insurance, 77.1% belonged to the contributive regimen, 7.8% to the subsidized regimen, 9.4% to exceptional regimens, and 5.7% to voluntary plans. The median body mass index was 25.98 kg/m2 (IQR: 22.7429.67). According to the WHO body mass index classification, 4.7% were underweight, 37% had a normal weight, 15.1% had Class I obesity, 6.8% had Class II obesity, and 1.6% had Class III obesity, as shown in Table 1.
Comorbidities
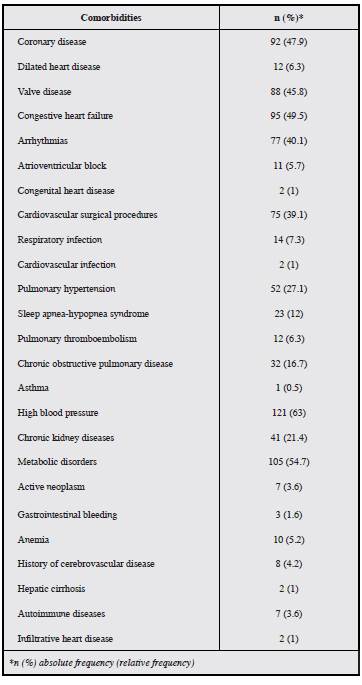
Altogether, 47.9% of the population had coronary disease, including unstable angina and acute myocardial infarction, among others. Dilated cardiomyopathy was found in 12 of the 192 patients. Valvular diseases were grouped together, with 45.8% found to have one of these disorders. Congestive heart failure was found in 49.5% and arrhythmias in 40.1%, atrial fibrillation and supraventricular tachycardia being among the most common, while 5.7% had some type of atrioventricular block. Only 1% had congenital heart disease.
Of all the patients, 14 were diagnosed with respiratory infections (bronchitis and pneumonia) and two with bacterial endocarditis. Seventy-five patients underwent cardiovascular procedures such as myocardial revascularization and valve replacements.
In addition, 27.1% had pulmonary hypertension, 23% had sleep apnea-hypopnea syndrome, 6.3% had pulmonary thromboembolism, 16.7% had chronic obstructive pulmonary disease and 0.5% had asthma (Table 2).
Vital signs on admission
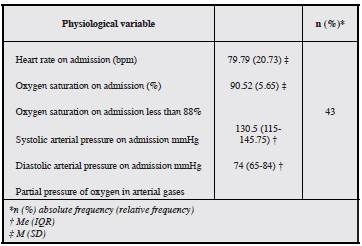
The admitting heart rate was 79.79 bpm, SD 20.73 bpm; and oxygen saturation on admission was 90.52%, SD 5.65%. On admission, 43 of all the patients had less than 88% oxygen saturation on room air and 149 had a higher saturation. The systolic blood pressure recorded on admission was 130.5 mmHg (IQR 115 -145.75 mmHg), and the admission diastolic blood pressure was 74 mmHg (IQR 65-84 mmHg). The partial pressure of inspired oxygen on admission was 0.21 for 60.4% of the patients, 0.24 for 6.3%, 0.28 for 14.6%, 0.32 for 6.3%, 0.35 for 1%, 0.40 for 1%, 0.45 for 0.5%, 0.5 for 1.6% and 0.99 for 0.5%.
Laboratory tests and imaging
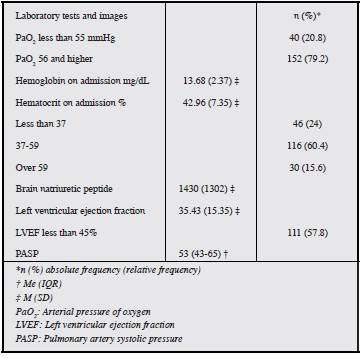
The admission complete blood count recorded a hemoglobin of 13.68, SD 2.37, and hematocrit of 42.96, SD 7.35; 30 patients, accounting for 15.6%, had a hematocrit greater than 49, and 46 patients (24%) had levels under 37. The brain natriuretic peptide level was 1,430 (SD 1,302). The echocardiogram showed a left ventricular ejection fraction of 35.43%, SD 15.35, and 57.8% of the patients had an LVEF less than 45%. The median pulmonary artery systolic pressure was 53 mmHg (IQR 43-65).
Arterial gases showed a partial pressure of oxygen of 64 mmHg (IQR 52.95-78.8 mmHg), and 20.8% of the patients had a PaO2 less than 55 mmHg; arterial blood bicarbonate was 23.47, SD 5. The partial pressure of CO2 in arterial blood was 33.97, SD 9.7.
Discussion
The main reason for beginning oxygen therapy is to manage tissue hypoxia and its effects 1,6,23. Hypoxemia is defined as a PaO2 less than 80 mmHg at sea level 1. It is important to keep in mind that physiological compensatory mechanisms develop for both pulmonary as well as cardiac diseases, depending on the duration of the hypoxemia 1. These changes include increased cardiac output, as well as an increase in the number of arrhythmias due to involvement of the heart's excitation-conduction system 1,18. Our study found that 40.1% of the patients had some type of arrhythmia. Pulmonary hypertension may occur secondary to increased pulmonary vascular resistance due to alveolar hypoxia present in 27.1% of the study patients 1,10. The use of supplementary oxygen may reduce pulmonary artery pressure with long-term use, with a resulting decrease in mortality 10. Kidney hypoxia causes greater erythropoietin production which may be correlated with the finding of hematocrits greater than 48% in 15.6% of the people 1,10.
Altogether, 79.2% of the patients were admitted with a heart rate above 90 beats per minute, which could reflect the effect of hypoxia on the peripheral vascular beds and the need to increase cardiac output to improve the supply of oxygen 11.
The indications for beginning home oxygen therapy are based on studies performed in the 80s: the NOTT and the MRC 5,7,8,10,12,21. However, one of the main problems with these studies is the oxygen concentration cut-off point selected during study design 7. The prescription of home oxygen is based on a resting arterial oxygen pressure less than 55 mmHg or 56-59 mmHg with cor pulmonale or target organ damage due to hypoxia 5,8,9,11,12, and a hematocrit greater than 55% 5,11. Only 40 patients, accounting for 20.8% of the sample, were found to have a PaO2 less than 55 mmHg, for whom, based on the foregoing, oxygen therapy would be indicated.
Cardiovascular diseases currently cover about half of the noncommunicable diseases 16. In this study, we found that almost half of the patients had documented coronary disease; 45.8% had some sort of heart valve disease and 40% had arrhythmias.
Chronic heart failure includes biological, structural and functional disorders which affect cardiac function; 49.5% of the study subjects had a diagnosis of heart failure 18.
We found that 42.7% of the study participants were active smokers on admission, and 7.8% had been smokers at some time. Smoking is known to cause several disorders, especially of the lungs, which lead to the need for supplemental oxygen 5. Wick et al. 21 found that up to 90% of COPD patients were active smokers or had quit smoking.
It has been reported that up to 70% of oxygen prescriptions do not have a clear indication, and up to 26-30% of patients do not have a clear follow up plan 5,10,22. However, given that data were included from individuals who were admitted to the hospital and were given an order for oxygen therapy, data regarding response, adherence or results following this intervention were not available. It should be noted that the positive effects of oxygen therapy require adequate adherence by the patient, as well as optimized medical management 5,6,9 and smoking cessation 1,7,21 and, as shown previously, some patients were active smokers.
In the study by Collado et al. 6, the patients were able to be grouped according to the most frequent diseases for data analysis. However, most of the patients in this study had multiple comorbidities which could cause hypoxia; for example, 16.7% had chronic obstructive pulmonary disease, 5.8% had pulmonary thromboembolism and 0.7% had a history of asthma.
Globally, the prevalence of obesity has tripled since 1975 16. In 2016, more than 1.9 billion adults 18 years old or older were overweight, of whom more than 650 million were obese. Thirty-nine percent of adults 18 or older were overweight and 13% were obese 16. A total of 58.4% of the study subjects were found to have a body mass index over 25 kg/m2, and 8.4% had a BMI over 35 kg/m2.
Approximately 40% of those over the age of 25 have high blood pressure, going from 600 million in 1980 to one billion in 2008. High blood pressure causes 50% of the deaths from cerebrovascular events and 45% of the deaths from coronary disease 16. Of the 192 individuals included in the study, 121 had a diagnosis of high blood pressure.
The objective of this study is to determine the characteristics of patients with cardiovascular disease and the need for home oxygen over a period of three years. Being a descriptive study, a causal relationship cannot be established between the disease and the use of CHOT. Likewise, the patients' physiological and social variables were not acted on or manipulated and the quality of the information may be affected by incomplete data.
Conclusions
We found that only a minority of the study patients for whom CHOT was ordered met the currently accepted criteria. New studies should be performed to evaluate the indications for supplementary oxygen therapy in cardiovascular disease, as well as the results on the biological variables and the impact on the patients' quality of life. The result of physiological conditions as well as of diagnostic aids could be included to create a model for predicting which patients may require oxygen supplementation upon discharge.
Healthcare programs for chronic patients must be reinforced to regularly verify the need for ongoing oxygen supplementation based on diagnostic or laboratory tests and thus decrease costs and optimize resources. All the healthcare system actors must be integrated and staff trained on the types of devices and their respective indications, meshing these activities with the insurance companies in order to achieve the treatment objectives, since the healthcare system's structure is a barrier to follow up at a single institution. The patients and their families should be empowered to participate in decision making and be aware of the importance of adherence to treatment and lifestyle changes in order to control the disease.