Introduction
Thyroid cancer is the most common endocrine cancer, accounting for 1.9% of all malignant tumors diagnosed annually in the United States 1. According to information reported by GLOBOCAN, Colombia has an incidence of 9.1 cases per 100,000 inhabitants, being the seventh most common cancer 3. Its prognosis is generally good, and it has a 90% 10-year survival rate 2. Distant metastasis usually involves lung and bone parenchyma and visceral organs such as the liver. Pleural involvement in thyroid cancer is uncommon: secondary pleural involvement is reported less than 1% of all patients 4, but it may develop 61-132 months after the initial diagnosis 5. We present two cases of papillary thyroid cancer with pleural metastases.
Case 1
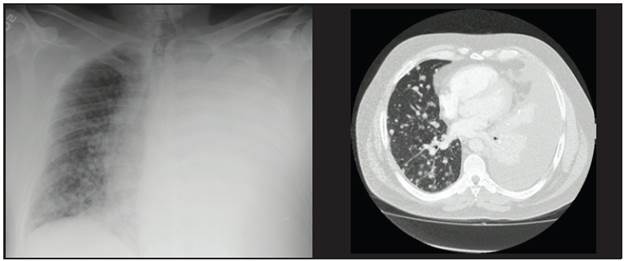
This was a 57-year-old patient with papillary thyroid carcinoma (initial stage IVB, T3bmN1bM1), treated initially with a total thyroidectomy along with central lymph node compartment and left modified radical emptying. The pathology showed 10 lymph nodes from the central emptying and 13 lymph nodes from the left modified radical emptying affected by the tumor, with no extracapsular extension, and a postoperative thyroglobulin of 8,557 ng/mL. A high-resolution chest CT was therefore ordered, which corroborated metastatic lung involvement in both lung fields. He received adjuvant therapy with 200 mCi of radioactive iodine (I-131), with no uptake on tracing, and it was therefore diagnosed as non-iodine-avid disease. Five months later he developed progressive dyspnea with radiological confirmation of a massive left pleural effusion which required thoracentesis on multiple occasions.
A cytochemical study of the pleural fluid was compatible with lymphocytic exudate, and the cytological study suggested papillary thyroid carcinoma involvement. The thyroglobulin level in the pleural fluid was markedly elevated at 7,046 ng/mL, confirming pleural involvement due to papillary thyroid carcinoma. At this point he had a serum thyroglobulin of 4,009 ng/mL, negative antithyroglobulin antibodies at 0.83 IU/mL (reference value < 4.11 IU/mL) and a TSH of 0.05 uIU/mL. A new tomography showed pulmonary disease progression according to the Response Evaluation Criteria in Solid Tumors (RECIST). He was considered to be a candidate for treatment with tyrosine kinase inhibitors. However, the patient developed severe SARS-CoV-2 pneumonia with acute respiratory distress syndrome (ARDS), requiring prolonged mechanical ventilation, and is currently at ECOG 3 with severe physical deconditioning syndrome, which has delayed the initiation of sorafenib.
Case 2
This was a 63-year-old patient with the classical variant and follicular infiltrative variant of papillary thyroid carcinoma, initially stage IVB, T2mN1bM, who underwent total thyroidectomy with central compartment and left modified radical emptying. She had one positive lymph node in the central emptying and three affected lymph nodes in the left modified radical emptying, none with extracapsular extension. The postoperative thyroglobulin was 130.6 ng/mL and antithyroglobulin antibodies were negative. Therefore, a high-resolution chest tomography was performed showing micronodular involvement in both lung fields. Adjuvant therapy with I-131 was administered, with a total of 300 mCi received and post-therapy tracing showing no pulmonary uptake. It was decided to administer TSH suppression treatment with levothyroxine, and the patient showed clinical stability for the following three years. In the fourth year, she developed dyspnea and right-sided pleuritic chest pain with a chest x-ray showing right pleural effusion. She underwent thoracentesis, with a cytochemical study of the pleural fluid compatible with lymphocytic exudate and an immunohistochemical study of the pleural fluid positive for PAX8 and calretinin and negative for WT-1, D2-40, TTF-1 and thyroglobulin. These findings are highly suggestive of metastasis from a papillary thyroid carcinoma. The patient had a recurrent pleural effusion, and therefore it was decided to perform talc pleurodesis. To date, she has had no further episodes of pleural effusion. The proper time for beginning tyrosine kinase inhibitors will be determined with the patient based on the results of new tomographic studies.
Discussion
Pleural involvement in well-differentiated thyroid carcinoma is extremely rare; it is estimated to occur in less than 1% of patients with papillary thyroid cancer. According to an extensive review conducted at the MD Anderson Cancer Center of 1,772 patients with differentiated thyroid cancer, only 0.6% of the patients developed pleural metastases 3, and there are currently only about 50 cases reported in the literature 4.
Despite being an unusual manifestation of differentiated thyroid carcinoma, its presence has been proven to dramatically worsen the prognosis in people with papillary thyroid cancer, with reported median survival rates between 10 and 15 months 3-5.
As in our two cases, the 10 cases reported by MD Anderson already had pulmonary involvement before developing pleural involvement 3 and this is something which has been seen in the vast majority of cases previously reported in the literature 6-9.
In Case 1, we based the diagnosis on the cytopathological findings and markedly elevated thyroglobulin levels in the pleural fluid. In Case 2 we had immunohistochemistry studies which supported the diagnosis. In the literature, the most common cytological findings in differentiated thyroid carcinoma pleural metastases are ovoid nuclei, irregular nuclear edges, psammoma calcifications and moderate amounts of vacuolated cytoplasm within the tumor cells. However, a precise diagnosis may be difficult with the cytological study alone, and therefore immunohistochemical studies are recommended which, if positive for CK7, CK9, TTF-1, PAX8 and thyroglobulin, would support the diagnosis of pleural metastasis of papillary thyroid carcinoma 10,11. The patient in Case 1 also had markedly elevated thyroglobulin levels in the pleural fluid; this finding has been suggested by some authors as a possible marker of pleural involvement in thyroid cancer. However, its cut-off points have not been determined and it is not universally accepted, in part because of its rarity 12.
Regarding treatment, there is no consensus on the management of pleural involvement in differentiated thyroid cancer. Historically, it has been proposed that treatment aim at improving symptoms such as dyspnea using thoracentesis as needed or pleurodesis in selected cases 4. Our belief is that this should be performed as soon as possible, considering pleural effusion to be evidence of disease progression. Within the last decade, tyrosine kinase inhibitors (TKIs), like sorafenib and lenvatinib, have become a treatment option in patients with iodine-refractory differentiated thyroid cancer with local or metastatic progression, improving progression-free survival when compared with placebo 13,14. As in the two cases we presented, the vast majority of patients with pleural involvement already have pulmonary metastases, which could facilitate RECIST follow up to evaluate the response to treatment, given that the response of pleural effusion is difficult to evaluate objectively beyond a measurement of volume. There are case reports in which both sorafenib and lenvatinib have led to a noticeable decrease in pleural effusion in patients with thyroid carcinoma 15,16. To date, we have found no reports of NTRK fusion uses, such as larotrectinib. Due to the prognostic implications of pleural effusion, this type of medications could be the promising systemic therapy in patients with thyroid carcinoma even without documented pulmonary progression.
Conclusions
Pleural involvement in differentiated thyroid carcinoma is a rare manifestation; however, it dramatically worsens the survival of patients who develop it. It should be considered as disease progression, although it is hard to objectively quantify it (beyond imaging data such as ultrasound) and evaluate the response to any treatment instated. It is important to encourage evacuating thoracentesis and the measurement of thyroglobulin in the pleural fluid to determine its definitive role in the disease. Pleurodesis should be recommended early in these cases. Tyrosine kinase inhibitors appear to be a promising treatment option for this group of patients.











 text in
text in