Introduction
Thrombotic microangiopathy (TMA) is a microcirculation disorder characterized by endothelial inflammation and microthromboses mainly involving capillaries and arterioles. It can be systemic, characterized by Coombs-negative microangiopathic hemolytic anemia affecting multiple organs, or may also be localized in organs such as the kidneys, the latter being more difficult to diagnose 1. Thrombotic microangiopathy is classified as: thrombotic thrombocytopenic purpura when it is associated with deficient ADAMTS13 enzyme activity; typical hemolytic-uremic syndrome when it is caused by the Shiga toxin associated with gastrointestinal infections caused by bacteria which produce this toxin; primary atypical hemolytic-uremic syndrome which is associated with genetic problems in complement regulation; and secondary atypical hemolytic-uremic syndrome which has several causes such as autoimmune disease, malignant neoplasms, gestational disorders, hemodynamic problems, metabolic disorders, transplant rejection, and exposure to toxins or medications that are detrimental to the endothelium, including gemcitabine, etc. 2-4. Causes secondary to toxins or medications are the ones most associated with localized chronic forms of thrombotic microangiopathy. However, there is always a high risk that a localized form will become systemic, with high morbidity and mortality, and therefore it is important to identify it in order to discontinue the offending agent 5. Below we present the case of a patient with inoperable pancreatic adenocarcinoma who developed progressive chronic kidney disease associated with localized thrombotic microangiopathy in the kidneys, secondary to gemcitabine.
Case report
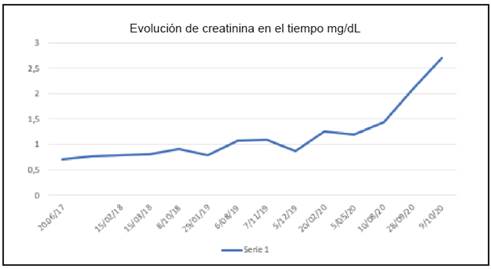
The patient was a 59-year-old female heavy ex-smoker with a history of hypothyroidism. In June 2017, she was diagnosed with well-differentiated T4NxM0 pancreatic carcinoma (histology documented), which was inoperable due to vascular involvement. Therefore, in June 2017, she was started on chemotherapy with gemcitabine plus nab-paclitaxel on days 1, 8 and 15 every 28 days, with no complications and with controlled disease throughout the process. Her creatinine at the beginning of treatment was 0.7 mg/dL with a completely normal urinalysis. Beginning in February 2020, a mild, progressive increase in creatinine was documented, associated with anemia and thrombocytopenia (which improved with adjustments of the chemotherapy dose). She was also found to have high blood pressure, which was treated medically, and chemotherapy was continued (Figure 1). Due to persistent pancytopenia and a greater creatinine increase, chemotherapy was discontinued in September 2020. The patient was hospitalized in October 2020 for accelerated kidney function deterioration, edema and respiratory difficulty. Imaging studies showed stable, localized pancreatic cancer. Her creatinine rose to 2.7 mg/ dL, and she had glomerular proteinuria and hematuria. Her CBC showed pancytopenia and elevated LDH; there were no schistocytes on the peripheral blood smear. She had normal-sized kidneys on ultrasound, and an echocardiogram showed adequate ventricular function (Table 1). A possible chemotherapy-induced renal-limited thrombotic microangiopathy was suspected, versus glomerular disease secondary to a malignant neoplasm (membranous or focal segmental glomerulosclerosis with associated tubular damage). A kidney biopsy was performed, revealing chronic TMA (Figure 2). Due to this biopsy finding, which was clearly related to gemcitabine, it was recommended that this medication be discontinued. The patient was evaluated again by oncology in November 2020; in light of her deteriorated kidney function, pathology findings and condition, the antineoplastic treatment was discontinued, and a consult was requested with radiotherapy/radiosurgery to assess the option of local control and redefine systemic antineoplastic treatment options based on her progress. The patient continued under observation and in January 2021 her creatinine levels improved (1.74 mg/dL), the anemia and leukopenia resolved, and mild thrombocytopenia persisted (139,000), with no edema or dyspnea. Imaging showed a stable pancreatic lesion with vascular involvement but no systemic involvement. She is awaiting a decision on the radiosurgery option.
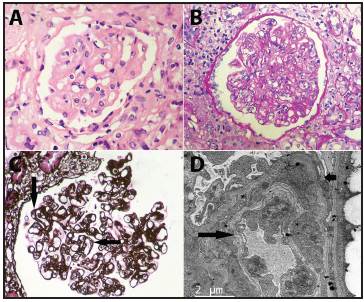
Figure 2 A: solidified glomerulus, loss of capillary lumens in some segments, where the capillary walls are thickened due to endothelial edema (hematoxylin-eosin, 400X). B: only a few capillary lumens can be seen in this glomerulus; there are increased endothelial and mesangial cells and capillary wall thickening (PAS, 400X). C: the double edges of the capillary walls (some marked with arrows) indicate a response to endothelial or subendothelial assault; in this case, in which immunofluorescence was negative for immune complexes and complement, it is an indirect sign of thrombotic microangiopathy (methenamine silver 400X). D: this capillary has evident wall damage; the short arrow points to a podocyte which has lost pedicels, underlying which is the basement membrane, inside, laminated material (long arrow) can be seen, corresponding to a double edge. Between this and the basement membrane there is heterogenous material which may correspond to cell detritus and cytoplasm. The endothelium has lost its normal fenestrations (transmission electron microscopy, original magnification, 400X).
Table 1 Laboratory tests and diagnostic imaging.
| Test | Result |
|---|---|
| Urinalysis | Erythrocytes 11-20/HPF, dysmorphic; leukocytes 0-5/ HPF, hyaline casts 0-5/HPF, granular casts 0-5/HPF, protein 75 mg/dL, density 1.015 |
| 24-hour urine protein | 670 mg/24 hours |
| Complete blood count | Hemoglobin: 8.1 g/dL, MCV 96.7 fL, MCH 31.6, hematocrit 24.8%, leukocytes (mm3): 2,100, neutrophils 819, lymphocytes 462, platelets 107,000 |
| Peripheral blood smear | Anisocytosis +, microcytosis+, macrocytosis+, hypochromia +, polychromatophilia. No schistocytes |
| Ferritin | 929 ng/mL |
| LDH | 484 UI/L |
| Bilirubins | Direct bilirubin: 0.12 mg/dL, total bilirubin: 0. 53 mg/dL |
| PTH | 385 pg/mL |
| Creatinine | 2.7 mg/dL |
| BUN | 35.9 mg/dL |
| Haptoglobin | 70 mg/dL |
| Direct Coombs | Negative |
| ADAMTS 13 | 66% |
| Partial thromboplastin time | 35 seconds |
| INR | 1.1 |
| Fibrinogen | 388 mg/dL |
| Urinary tract ultrasound | Normal-sized kidneys with no hydronephrosis, adequate corticomedullary differentiation. |
| Echocardiogram | LVEF: 59% with mild pericardial effusion, no chamber dilation or indirect signs of pulmonary hypertension. |
Discussion
Thrombotic microangiopathy is characterized by diffuse endothelial damage with a great deal of inflammation and microvascular occlusion, leading to localized kidney damage or multiple organ damage indicated by Coombs-negative microangiopathic hemolytic anemia with multiple organs affected such as the kidneys, central nervous system, cardiovascular system and gastrointestinal tract 1. It is classified as thrombotic thrombocytopenic purpura (TTP) associated with decreased ADAMTS13 enzyme activity of < 10%, and as hemolytic-uremic syndrome (HUS), which may be typical (due to Shiga toxin-producing bacteria) or atypical (related to genetic or secondary causes: autoimmune, neoplastic, hemodynamic, metabolic, gestational, toxic, drug-induced).
Both neoplasms as well as antineoplastic drugs have been associated with secondary HUS. The most common malignant neoplasms which can cause TMA include stomach, colorectal, breast, lung, prostate and pancreatic adenocarcinomas 6,7. Generally, its association with an underlying malignancy indicates a very poor prognosis and an advanced and/or metastatic state of the malignancy. The antineoplastic drugs reported include gemcitabine, mitomycin C, bleomycin, cisplatin, sunitinib, imatinib, and 5-fluorouracil 6. It may occasionally be difficult to differentiate between cancer-associated and chemotherapy-associated TMA. However, cancer-associated TMA typically occurs during widespread untreated metastatic disease, while the chemotherapy-induced type occurs more frequently when the patient has received several treatment cycles or is even in disease remission. The difficulty occurs when a specific cancer does not respond to chemotherapy, progresses, and the patient presents with TMA. In this case, either of the two situations could explain the TMA 8,9.
Gemcitabine is an antineoplastic agent widely used in oncology. It is a pyrimidine antimetabolite whose mechanism of action is to inhibit DNA synthesis. It is indicated for bladder, pancreas, lung, ovarian and breast cancer. The most common adverse effects of gemcitabine are hematologic and gastrointestinal toxicity. Pulmonary toxicity (interstitial pneumonitis) has also been reported, as well as cases of TMA which, if not detected, may lead to greater complications such as acute or chronic kidney failure with a need for dialysis, or even to the patients' death from multisystemic damage 5,14. The first case of gemcitabine-induced TMA was reported in 1994, during a phase II study of patients with metastatic pancreatic carcinoma 10. Since then, this agent has been clearly associated with TMA, and should be suspected immediately in the event of unexplained kidney failure or unclear anemia with thrombocytopenia. Elevated LDH, low haptoglobin and schistocytes can facilitate the diagnostic suspicion; however, in localized cases, only a kidney biopsy can confirm TMA 6.
The incidence of gemcitabine-induced TMA ranges from 0.015 to 1.4% 8. However, this incidence is probably underestimated due to underreporting, scant recognition of the disorder or not diagnosing mild symptoms 6. The risk of gemcitabine-induced TMA increases with a cumulative drug dose of more than 20,000 mg/m2 or more than 18 cycles administered. The condition rarely occurs before seven months of treatment 9.
The pathophysiology of gemcitabine-induced TMA is unclear. It is believed to be an immune-mediated response or a direct toxic effect in which endothelial injury is the main event 7. Chemotherapy-induced TMA can be divided into type I and type II. Type I develops in a dose-dependent fashion, typically six or more months after beginning treatment, and is usually permanent and irreversible (it may be caused by mitomycin C, gemcitabine and oxaliplatin). It tends to be associated with acute or chronic kidney failure. The pathological finding is arteriolar and glomerular capillary thrombosis. On the other hand, type II is not dose-related, may occur at any time after beginning treatment and during treatment (from one dose up to 29 months later) and has a high probability of recovering once the drug is discontinued. The renal-limited involvement is characterized by glomeru-lar capillary thrombosis 6.
The pillar of drug-induced TMA treatment is withdrawal of the implicated agent. When there is hematological and multisystemic involvement, plasma exchange has been reported to play a role in its control 10,11. Other treatments such as glucocorticoids, doxycycline, rituximab and eculizumab have been reported to be successful, but no benefits have been found in others 7,12,13.
In conclusion, it is difficult to distinguish between chemotherapy-induced TMA and that caused by a malignant neoplasm. However, it is important to suspect it, as it is associated with high morbidity and mortality. Although there is no specific recommendation for diagnosing and treating chemotherapy-associated renal-limited TMA, the implicated drug should clearly be discontinued, and another alternative sought to control the malignant neoplasm. The reported patient had progressively worsening kidney function of unclear origin, along with anemia and thrombocytopenia (which was initially thought to be secondary to chemotherapy), and the kidney biopsy documented type II chronic TMA, clearly associated with the chronic use of gemcitabine since, while her cancer continued to be active, it had not progressed. Gemcitabine was discontinued in this patient and, as we reported above, her kidney function, blood disorders and clinical condition have improved. Local radiotherapy was chosen to treat her underlying disease, which is still localized, and this is still pending.











 text in
text in