Introduction
Venous thromboembolic disease (VTED) is a systemic disorder which includes deep vein thrombosis (DVT) and pulmonary thromboembolism (PTE). It is the third most frequent cardiovascular disease, but has a higher mortal ity than acute myocardial infarction 1. The incidence of VTED has been estimated to be one to two cases per 1,000 inhabitants per year 2,3, and fatalities could range from 6% to 12.9% for DVT or PTE, respectively 4,5. In addition, between 42 and 64% of institutionalized patients are at medium to high risk of developing it, a proportion that could increase to 72% in surgical patients 6.
There are limitations in the estimates of incidence, at tributable mortality, complications and the costs of VTED for the healthcare system. One of these is the variable in cidence and mortality according to the geographic regions studied, probably due to differences in the sociodemographic characteristics and risk factors of the cases 7, the technical ability to detect it, and clinical management in each region. In addition, the characteristics of the disease itself make it difficult to detect, as some cases show no initial symptoms. For example, a meta-analysis found that the prevalence of incidental PTE was 2.6% (95% CI: 1.9; 3.4) 9. Furthermore, its diagnosis requires a high degree of clinical suspicion and specialized tests, making it difficult and costly to carry out population and field studies 3,10. Thus, there is limited epidemiological information available on the subject 3,8. The combination of these factors appears to justify an underestimate of the epidemiological indices such as PTE incidence and mortality.
Despite the possible underestimation of the incidence of VTED, this disease is the first cause of disability-adjusted life years lost. A total of 7,681,000 (between 3,115,000 and 14,034,000) years of life lost have been reported, which are 2.4 times greater in low and middle-income countries 11 and explain part of the disease's high cost 7. Dennis et al. carried out a study in 1996 in various cities in the country, finding that 7% of hospitalized patients had VTED and 2.4% were diagnosed with APTE 12. A multicenter registry based on information from four cities found that the inpa tient mortality for APTE reached 14.8% (95% CI 11-19%) in a cohort of hospitalized patients. The factors associated with a fatal outcome were hypotension (RR=2.57; 95% CI 1.4-4.73) and hip fractures (RR=2.55; 95% CI 1.34-4.83). This registry, however, does not present data disaggregated by city or participating center 13.
All of this indicates that there is very limited information available to estimate the regional or national burden of PTE in Colombia. The objective of this study was to analyze the incident cases of symptomatic acute pulmonary thromboem bolism (APTE) in the department of Santander which required inpatient treatment, their geographic location and the estimate of attributable mortality, based on a data search of the large administrative databases which code hospital discharges in the various provinces of the department of Santander.
Methods
Context
The information available in the Comprehensive Social Protection Information System of Colombia (SISPRO) and the Public Health Observatory of Santander, along with the information provided by the statistical departments of nine tertiary and quaternary healthcare institutions in Santander (Fundación Cardiovascular de Colombia, Hospital Univer sitario de Santander, Fundación Oftalmológica de Santander Carlos Ardilla Lülle -Foscal, Clínica Materno-Infantil San Luis, Clínica Chicamocha, Instituto del Corazón de Bucaramanga, Clínica Bucaramanga, Hospital Universitario Los Comuneros, Saludcoop and Instituto Neumológico del Oriente), as well as information provided by the quality of fice of the Departmental Secretariat of Health was used to identify PTE cases.
Participants
Patients with an ICD10 diagnosis of pulmonary embolism in the participating sources' registries (restricted to the period between January 2010 and December 2014) were included in the analysis.
Variables
The demographic variables, place of origin, place of referral, type of care, medical treatment required, condition at discharge and readmission records were analyzed.
Statistical analysis
All data were analyzed as the number of points of care. A descriptive analysis of all reported points of care was per formed by information source, identifying duplicate data and reporting the median and minimum and maximum values when the data distribution did not approximate normality. Absolute frequencies and percentages were also presented for categorical variables. In addition, the incidence rates were estimated using the population reported by the National and Statistical Administrative Department (DANE) for each municipality. Finally, logistic and linear regression were applied, as appropriate, to determine associations between the study variables. All analyses were performed using authorized STATA 9.0 software.
Biases
In order to overcome the limitation of not being able to identify duplicate points of care, an analysis was performed which looked at the frequency of the number of points of care per patient, to generate intervals under different care frequencies per patient.
Ethical considerations
This study adheres to Resolution 8430 from 1993 and is considered a no-risk study as it uses secondary informa tion. The investigators analyzed all the data provided under strict confidentiality measures such that, once the data was cleaned, the identification variables for each patient were eliminated.
Results
Record of incident APTE cases in the department of Santander, 2010-2014
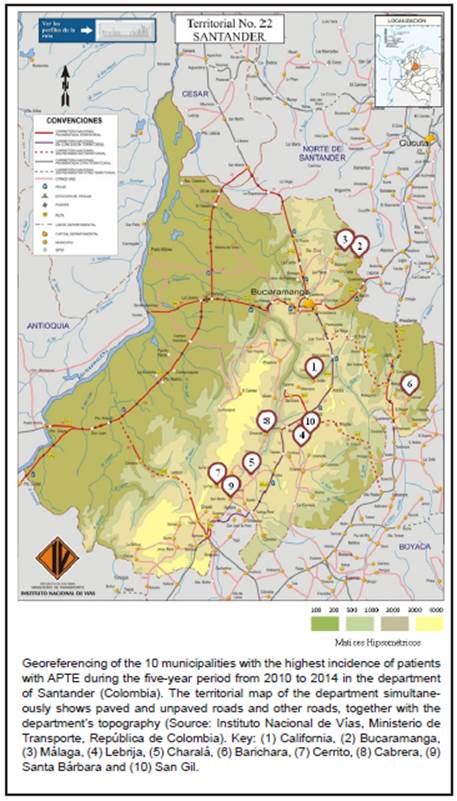
A total of 2,879 points of care for APTE (576 cases with an identification number) were recorded. These were adults (61±18 years) with a 1.3 M:F ratio (Table 1), mostly (78%) from the municipalities of Bucaramanga, Floridablanca, Piedecuesta, Girón and Lebrija. The municipalities with the highest incidence were California (1,093 per 100,000 inhab.), Bucaramanga (278 per 100,000 inhab.) and Málaga (257 per 100,000 inhab.). Figure 1 shows the incidence of PTE for Santander (149 cases per 100,000 inhab.) as well as the simulated incidence if every case had been simultaneously reported in more than one institution for the same event, in order to see how much the incidence might vary if there were simultaneous reporting. Figure 2a shows the incidence distribution by municipality in Santander. Similarly, Figure 3a shows the location of the 10 municipalities with the highest incidence, highlighting that most of these are found in the mountainous region of the eastern mountain range.
Table 1 Demographic and general descriptive characteristics of acute pulmonary thromboembolism (APTE) cases in the department of Santander, 2010-2014.
| n | % | |
|---|---|---|
| Total points of care | 2,879 | |
| Sex (male) | 1,188 | 41% |
| Age | 63* | 18-97** |
| Type of care | ||
| Emergency room | 2,088 | 73% |
| Hospital ward | 527 | 18% |
| ICU | 102 | 4% |
| Surgery | 61 | 2% |
| Hemodynamics | 101 | 4% |
| Length of stay (days) | 4 | 1-140 |
| Readmission+ | 72 | 17.40% |
| *Median; **minimum -maximum; + Only for FCV patients. | ||
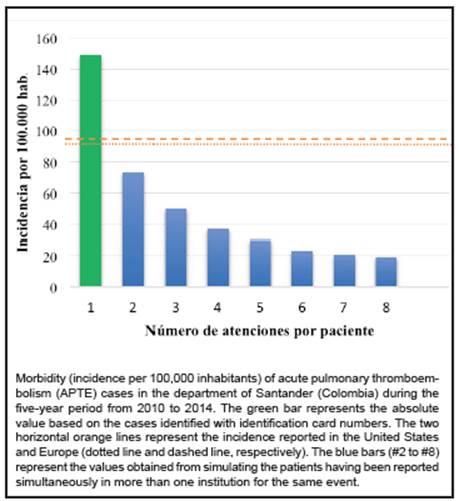
Figure 1 Morbidity due to acute pulmonary thromboembolism in the department of Santander (Colombia), 2010-2014.
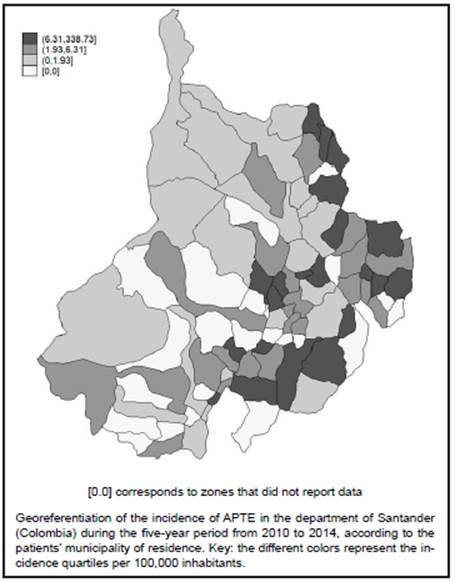
Figure 2a Morbidity per 100,000 inhabitants for acute pulmonary thromboembolism in the department of Santander (Colombia), 2010-2014.
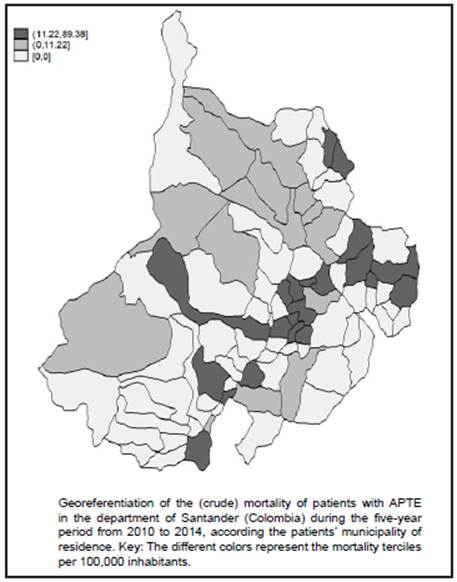
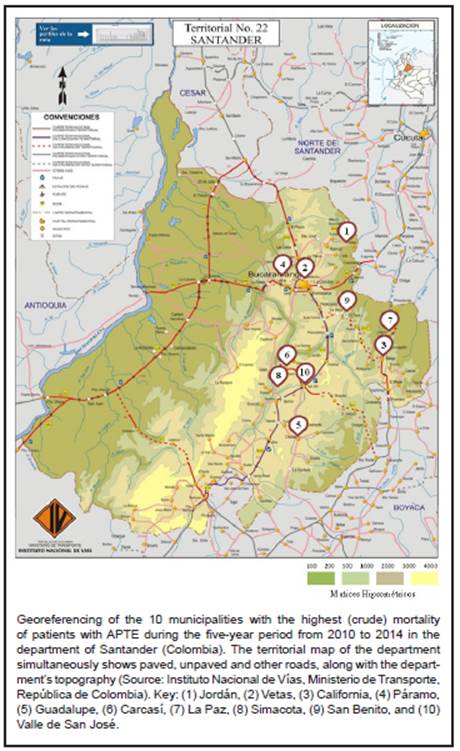
Figure 2b Mortality in patients with acute pulmonary thromboembolism in the department of Santander (Colombia), 2010-2014.
APTE mortality
The APTE mortality rate was 8.03 deaths per 100,000 inhab. The attributable mortality could not be estimated due to insufficient data. Only 0.7% of the referrals were made through the Emergency Control Center. On another note, 79 patients (17.52%) had to be admitted to the intensive care unit. Figure 2b presents the mortality distribution by municipality in the department of Santander. Figure 3b shows the location of the 10 municipalities with the greatest mortality, with the peculiarity that they are found in the mountainous zone of the eastern mountain range and are spread out from the reference city, which is Bucaramanga.
Associations with the geographical location of APTE cases
A review of the geographical location of the cases showed a tendency for cases to increase with increased altitude (meters above sea level [MASL]) of the case's place of residence. Therefore, the correlation between altitude and the incidence of APTE was evaluated, finding that the incidence of APTE increased by 4.1 per 100,000 inhab. for every 100 meters increase in altitude (p= 0.01; 95% CI 1.90-6.33). The incidence of APTE was inversely related to the time required to reach the reference city, such that for every minute more required to access the reference site, the incidence of APTE decreased by 0.4 cases per 100,000 inhab. (p= 0.021; 95% CI -0.67-0.057). The APTE mortality was correlated with the altitude above sea level of the city of residence, finding that mortality increased by 1.0 per 100,000 inhab. for every 100 meters of increased altitude (p= 0.035; 95% CI 0.08-2.0). The land travel time from the residence sites to the reference city, which is the city of Bucaramanga, was also analyzed. The median was 60 minutes. When the cases resided more than 60 minutes away, APTE mortality increased by eight units (adjusted for age). It is worth noting that information on the number of institutions and days between the initial consult and admission to the final treatment institution was not available.
Discussion
To our knowledge, this study is the first to analyze incident cases of symptomatic APTE requiring hospital treatment, their geographic location and regional attributable mortal ity. The main findings can be summarized in two groups of evidence. First, we noted that some municipalities like California or the capital city, Bucaramanga, have an APTE incidence up to 10 times greater (1,093 and 278 cases per 100,000 inhab., respectively) than expected based on what is reported in Europe (95 per 100,000 inhab.) 14, France (110 per 100,000 inhab.) 2 or the United States (112.3 per 100,000 inhab.) 15. Second, in addition to presenting the data in terms of the magnitude of the APTE incidence and mortality, the current study identifies a correlation between the altitude of the municipality and incidence of APTE (p= 0.01). Other authors have mentioned that exposure to high altitudes, whether through airplane travel or climbing to mountainous zones, may cause a hypercoagulable state which predisposes to venous thromboembolism 19,20. In addition, marked differences have been found in the occur rence of thromboembolism as a postoperative complication when surgeries are performed at higher altitudes 21. How ever, there is controversy regarding the pathophysiology of altitude as a risk factor for APTE, since it could be caused by one or more factors like hypoxemia, hemoconcentration, using tighter clothing, forced stasis due to severe weather, and/or the convergence of Virchow's triad (venous stasis, hypercoagulability and endothelial damage) 21,22.
The current study ratifies the importance of conducting local and regional studies seeking factors associated with elevated incidences in certain cities or specific municipali ties, inquiring about individual genetic, epigenetic and social factors. Some observational studies have found an associa tion between air pollution, the distance to roads or highways, and cardiovascular and cardiopulmonary mortality 23,24; therefore, it would be worthwhile for future studies to take the assessment of environmental pollution into account. It is notable that California was the municipality with the high est incidence in this study. It is located at a medium-high elevation (2,005 MASL) and its main economic activity is to metal mining. Whether this convergence of factors represents a particularly elevated risk for the inhabitants of this region is a matter for study.
The current study has also estimated the crude inpatient mortality rate for APTE at 8.03 per 100,000 inhab. This figure is higher than the mortality reported in a multinational European study (6.4 per 100,000 inhab.) 16, a Brazilian study (2.1 per 100,000 inhab.) 17, a North American study (4.0% inpatient; 9.4% at 30 days and 24.1% at one year), or an Italian study (10%) 18. The reason for these differences cannot be clearly deduced. Thirty-day or 12-month mortal ity data is not available. However, the current study found a correlation between the inpatient mortality rate of patients with APTE and the distance from the place of origin to the reference center for medical care. This correlation allows us to think that delayed care could be involved in the region's PTE mortality.
An additional point having to do with possible post-APTE sequelae is that there was insufficient information in most of the participating institutions to estimate the cost of hospital care and the mid- to long-term outcomes of the study patients. One of the long-term complications, perhaps the most serious and debilitating one, is chronic thromboembolic pulmonary hypertension, previously thought to be a rare complication in 0.1-0.5% of patients who survived an APTE event. Recent studies have reported that the incidence of pulmonary hypertension may be considerably greater (0.4 to 8.8%), mainly in those with large thrombi in pul monary arteries and those classified as having intermediate risk 25. While this was not the subject of this study, the high incidence of the disease in the Santander population justifies a methodical and systematic search for pulmonary hypertension in these patients.
This is an initial scientific look at the issue of APTE in a regional context. However, its limitations should be mentioned. Descriptive studies based on records may have biases due to lack of information. For APTE, underreporting could be considered quantitatively relevant. However, the incidence detected in some municipalities in the department is much higher than what has been reported in other coun tries, which leads us to suspect two possibilities contrary to underreporting. The first is that this diagnosis may be overreported, but if this is the case, it would be very perti nent to identify the reasons for it. The second is that cases may be duplicated in the database. However, this potential bias was avoided by including non-duplicated cases with an available identification number. Neither of these limita tions would appear to account for the statistically significant relationship between altitude and APTE mortality. The third possibility is that the higher-than-expected incidence in certain municipalities is really expressing the existence of unidentified regional risk factors. The study shows a significant association between APTE and elevation above sea level. This data amply justifies performing new studies with a complementary epidemiological design to determine the actual association between the study variables. It should be noted that the current study includes the analysis of data collected for the five years prior to 2014, and therefore we recommend that similar analyses be performed with recent data to allow comparability between periods, identify inci dence and mortality trends and evaluate changes in the treat ment guidelines for these cases. Another limitation of this study is the impossibility of determining the care route each patient followed prior to reaching the center which reported the case. Methodologically, we believe that a simulation to calculate the incidence and mortality when the patient has consulted at more than one institution could be useful for complementing the analysis.
The logical progression for tackling the issue detected in this study is the creation of a multicenter APTE registry. A good registry is a relatively economical tool for understanding the epidemiological situation of APTE in the region. The in formation obtained allows population groups with outstanding rates to be identified within the general population and aims at identifying risk factors through the detection of individuals with specific exposures or populations with a high rate of APTE. This information is essential for providing basic decision-making elements for planning and evaluating thromboembolic disease control programs in the region. However, its clinical importance is perhaps greater, due to the impact of understanding the course of treated APTE cases, whose outcomes could be radically altered by a good diagnostic and treatment approach, considering that APTE has a considerable impact on the inpatient and outpatient morbidity and mortal ity of the affected individuals, increasing hospital care costs within a healthcare system in crisis 6,12,13.
Despite the detection and intervention of multiple risk factors carried out in the country, APTE continues to be one of the most feared and, occasionally, difficult to diag nose complications in patients receiving medical care in a healthcare institution, especially at basic care levels or in rural areas 3,7,8. Due to the poor specificity of some APTE signs and symptoms, and the high cost of confirma tory tests, it is diagnosed less frequently in low complexity centers, with a high proportion of mistaken diagnoses and barriers to anticoagulant therapy related to difficulties for monitoring in remote areas. These variables could explain an increased APTE mortality rate.
Conclusions
This study sought, for the first time, to estimate the inci dence and mortality of acute pulmonary thromboembolism in Santander, one of Colombia's Andean regions. Both epidemiological indicators are very high in some of the region's municipalities, when compared to what developed countries have reported. Altitude was associated with the incidence of the disease. This information is valuable in approaching the epidemiology of the disease and display ing the real importance of the problem, identifying funda mental differences which could eventually be useful for determining preventive policies for the disease, designing local diagnostic algorithms and improving the allocation of healthcare resources.











 text in
text in