Introduction
Due to the current COVID-19 pandemic, pneumomedi astinum cases have increased in various parts of the world 1, and our country is no exception. Pneumomediastinum cases caused by the new SARS-CoV-2 coronavirus infec tion have been termed "spontaneous." We believe that this assessment is incorrect. The current classification labels the group with the greatest triggering cause as "spontaneous;" therefore, it cannot be spontaneous, but rather secondary. We believe the classification should become more precise, and that the real definition of pneumomediastinum is not consistent with what has been published.
We propose a classification which will not only consider the etiology of the pneumomediastinum, but also help pro vide an accurate diagnosis and be useful in guiding selective treatment strategies for better care, as well as be easy to remember and useful for teaching.
We believe these are the first SARS-CoV-2 pneumomedi astinum cases reported in the country with positive outcomes using conservative treatment.
Case presentations
All were males between 28 and 74 years old who were admitted in poor general condition. The first three had no significant medical history; they were previously healthy, nonsmokers and did not use psychoactive drugs. They were regular athletes with an athletic build. The fifth patient began to experience respiratory symptoms 14 days prior to admission and had intense chest pain the day before, after a coughing fit. Various degrees of subcutaneous emphysema were found on palpation of the chest, supraclavicular fossae and neck in all but the fourth patient. Auscultation revealed diminished breath sounds and crackles in both lung bases, except in the fifth patient who had tympany and absent breath sounds over the left chest. All had a positive reverse transcriptase polymerase chain reaction (RT-PCR).
Table 1 presents some of the patients' demographic char acteristics and their main clinical and laboratory findings on admission. Figures 1-3 show the chest tomographies (CTs) without contrast.
Table 1 Some of the patients' demographic characteristics and their main clinical and laboratory findings on admission.
| Patient | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Age (years) | 36 | 28 | 28 | 70 | 74 |
| Sex | M | M | M | M | M |
| Comorbidities | None | None | None | COPD + HTN | COPD |
| Days with symptoms prior to admission | 8 | 10 | 7 | 12 | 14 |
| Temperature (°C) | 38.6 | 37.9 | 36.8 | 37.4 | 36.7 |
| Dyspnea | Yes | Yes | Yes | Yes | Yes |
| Coughing fits | Severe | Severe | Moderate | Moderate | Severe |
| Chest pain | Yes | Yes | Yes | Yes | Yes |
| General malaise | Yes | Yes | No | Yes | No |
| Chills | Yes | Yes | No | No | No |
| Heart rate (HR) | 114 | 122 | 110 | 128 | 136 |
| Respiratory rate (RR) | 36 | 32 | 38 | 44 | 56 |
| Blood pressure (BP) | 106/68 | 112/74 | 110/72 | 122/86 | 156/88 |
| O2 saturation on room air | 87% | 84% | 90% | 78% | 80% |
| PaFi | 96 | 102 | 89 | 78 | 75 |
| D-dimer (ng/mL) | 5498 | 4322 | 2225 | 4780 | 6745 |
| Ferritin (ng/mL) | 1765 | 2300 | 986 | 3787 | 1795 |
| Pneumomediastinum | Yes | Yes | Yes | Yes | Yes |
| Pneumothorax | No | No | No | Yes | Yes |
| Subcutaneous emphysema | Yes | Yes | Yes | Yes | Yes |
| Days to PM resolution | 4 | 9 | 6 | 12 | 14 |
| SARS-CoV-2 molecular test | Positive | Positive | Positive | Positive | Positive |
| M=male. HR and RR=per minute. HTN=hypertension. BP= mmHg. PaFi: PaO 2 /FiO 2 ratio. D-dimer, reference: 0-500ng/mL. Ferritin, reference for men 30-440 ng/mL. PM=pneumomediastinum. | |||||
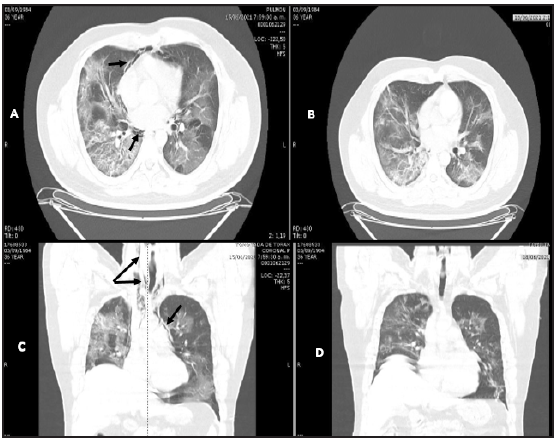
Figure 1 Patient 1. A and C: Simple chest CT. Axial and coronal planes. Air surrounding the vascular structures (black arrows) with bilateral ground glass, cobblestone, consolidated alveolar infiltrate areas extending to the neck. B and D: air reabsorption four days later.
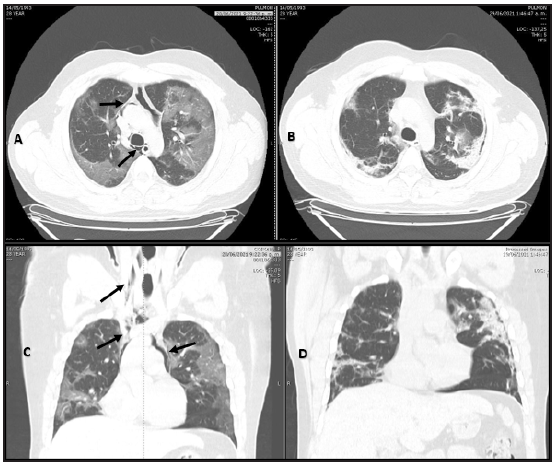
Figure 2 Patient 2. A and C: Simple chest CT. Axial and coronal planes. Air in the mediastinum extending towards the upper chest and lower neck. Black arrows. B and D: no air is seen nine days later.
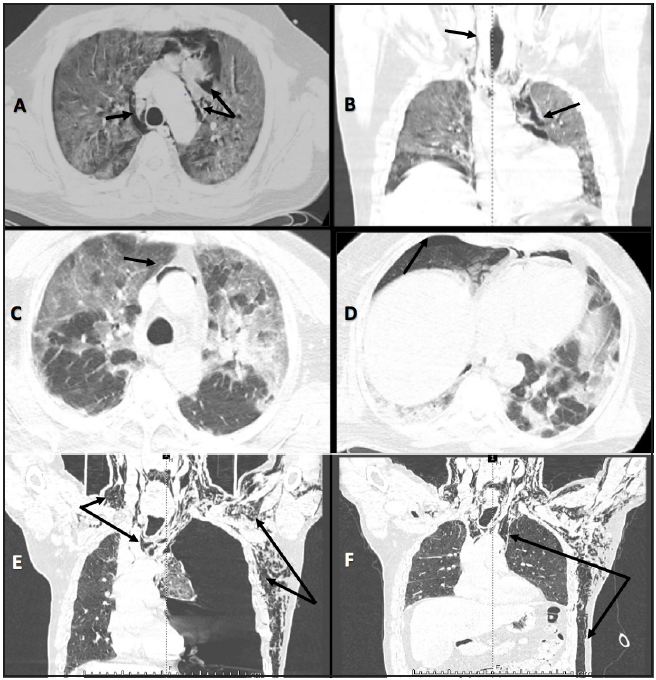
Figure 3 Patient 3. A and B: Simple chest CT. Axial and coronal planes. Air in the mediastinal and neck structures. Black arrows. Patient 4. C and D: axial plane. Air surrounding the vascular structures and a small concomitant right pneumothorax. Black arrows. Patient 5. E: Simple chest CT. Coronal plane. Large left tension pneumothorax displacing the mediastinal structures (blue arrows), extensive pneumomediastinum and subcutaneous emphysema extending to the ipsilateral neck, shoulder and arm, as well as to the anterior chest wall and abdomen. Black arrows. F: resolved pneumothorax with chest tube placement. Ongoing pneumomediastinum and subcutaneous emphysema. Black arrows.
The patients were given analgesics, steroids, antico agulants, empiric antibiotics and supplementary oxygen, as needed. The third patient also received tocilizumab, and the fourth one required six days of invasive mechanical ventila tion. The pneumomediastinum was treated conservatively. The fifth patient's pneumothorax resolved with a chest tube (Figures 3-E and 3-F). This is the only patient who is still hospitalized. All showed a favorable progression of the pneumomediastinum.
Discussion
The serious manifestations of SARS-CoV-2 infection are associated with an exaggerated immune response stimulated by interleukin-6, tumor necrosis factor a and other cytokines, in a pattern known as "cytokine storm" 2. The probable cause of pneumomediastinum in our patients, as in others with COVID-19, is diffuse underlying alveolar damage coupled with intense and repetitive dry cough episodes 3. Coughing fits have been known to cause a sudden increase in distal air pressure which leads to alveolar rupture with a secondary air leak to the peribronchovascular pulmonary interstitium, subsequently dissecting proximally up to the mediastinum 4.
In our cases, we opted for tomography over a chest x-ray because it is highly sensitive and has a high negative predic tive value for identifying COVID-19 patients 5. Typically, imaging in patients with SARS-CoV-2 pneumonia shows bilateral pulmonary opacities (ground glass and consolida tions) with a peripheral/subpleural distribution, and often the posterior regions of both lungs are especially affected 4, with fibrotic areas in more prolonged cases. We found these images in our cases. The patients ' clinical presentation, chemistries and blood gases were no different from what has been published, and therefore will not be discussed. What we will discuss here is the onset of pneumomediastinum as a complication, which medical literature classifies as "spon taneous," an assessment we do not consider to be correct. Likewise, subcutaneous emphysema and pneumomediasti num in COVID-19 patients have been reported to be poor prognostic indicators 6; however, we believe that these complications, as well as pneumothorax, do not appear to be independent markers of a poor prognosis.
COVID-19 associated pneumomediastinum and pneu mothorax are little reported in the medical literature 7. In our institution, from the first case detected on April 27, 2020, and up to June 28, 2021 (when we finished writing this presentation), 5,578 confirmed SARS-CoV-2 pneumonia cases in patients over the age of 18 had been seen, and only five cases of pneumomediastinum had been found, two of which had concomitant pneumothorax. The frequency of pneumomediastinum was 0.089%, a truly low frequency for this complication in our cases. All the patients were male, in line with what has been published 8. It is interesting that they all occurred within one month, and we do not know if this is related to the recent circulation of the Epsilon (B.1.427) and Gamma (P.1) lineages in Caquetá 9.
The following definition of spontaneous pneumomedias tinum, which is, in fact, old, continues to be used: "referring to the presence of air in the mediastinum of healthy subjects with no evident causal factors such as surgery, air following a viscous perforation, infection or trauma" 8. Histori cally, it has been divided into two groups: spontaneous and secondary. When there is no triggering cause, it is called "spontaneous," and it is secondary when there is a triggering traumatic event. In other words, whatever is not traumatic is "spontaneous." This definition is not consistent with the currently reported cases, and, over time, the classification has become nonspecific and inadequate. Using terms based on old definitions or nomenclatures may inadvertently dis seminate ambiguities in understanding true spontaneous, or better, primary, pneumomediastinum. The current medical literature calls the group with the greatest triggering cause "spontaneous." We believe that the classification should become more precise.
The "spontaneous" and "secondary" classification of pneumomediastinum should be avoided due to several predisposing factors and triggering events which are pres ent in what is currently called "spontaneous." Therefore, this term is confusing, inappropriate and nonspecific. We prefer a terminology which not only takes into account the etiology of the pneumomediastinum, but also helps guide selective management strategies for better care, and is easy to remember and useful for teaching.
Definitions and classifications, in general, are human interpretations of biological phenomena and may be true for some reasons while false for others. Clinically, they should be useful when they help provide a correct diag nosis, treatment or management. But sometimes medicine clings to norms, protocols, definitions and classifications as though they were dogmas, and therefore we cannot change or modify them. This should not be the case.
The definition given states that spontaneous pneumomediastinum occurs "in healthy subjects with no evident causal factor." This is true, but incorrectly used; "spontaneous pneumomediastinum," as in the currently published cases, would not be "spontaneous" but rather secondary to various factors (predisposing or triggering or both). Therefore, if it is secondary, it cannot be "spontaneous;" these are mutually exclusive. True "spontaneous" (primary) pneumomediastinum, by definition, cannot have an evident causal factor, as opposed to secondary pneumomediastinum which can be triggered by several different factors.
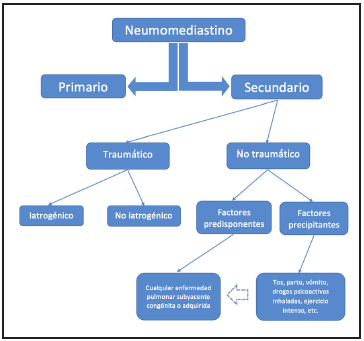
For us, if a pneumomediastinum has a predisposing factor involving the lung structure, whether congenital, hereditary or genetic (bronchiectasis, cystic fibrosis, surfactant disorders, etc.) or acquired (asthma, COPD, interstitial lung dis ease, COVID-19 pneumonia, etc.), it cannot be spontaneous because there is a predisposing underlying disease. Likewise, a pneumomediastinum caused by a precipitating factor (a coughing fit, labor, intense exercise, use of inhalants, me chanical ventilation, etc.) in a healthy person or someone with underlying lung disease, cannot be spontaneous either, because there is an immediate triggering event which causes it. Figure 3 modified by the same author of 10 an 11 to be simpler and more specific.
From this perspective, our cases are not spontaneous, but rather secondary, pneumomediastina, first because there is an underlying lung disease acting as a predisposing factor (SARS-CoV-2 pneumonia), and second because there is a precipitating factor which causes it (a coughing fit).
Pneumomediastinum is not a disease, but rather occurs in most cases as a complication of various predisposing and precipitating factors (including trauma). As we mentioned, these factors may occur simultaneously and cause a pneumomediastinum; for example, coughing or vomiting and acquired lung diseases. This type of pneumomediastinum is secondary. A pneumomediastinum which occurs in a healthy person without these factors is a true primary pneumomediastinum, which is a very rare and little-reported event in the global medical literature 12-14. In Colombia, there is one reported case of primary pneumomediastinum which was classified as "idiopathic spontaneous pneumomediastinum" 15. It is important to clarify that primary pneumomediastinum is the same as spontaneous or idiopathic pneumomediastinum, mediastinal emphysema or Hamman's syndrome. It is preferable to avoid using synonyms and eponyms. We prefer the term "primary" to differentiate it from the second ary type and avoid confusion. Sometimes, and especially when in doubt, secondary causes should be sought and ruled out through complementary studies to determine that a pneumomediastinum is primary.
The treatment of pneumomediastinum depends on the cause. The treatment for true primary pneumomediastinum is the same as for secondary, except that in secondary cases any trauma (iatrogenic or noniatrogenic) should be ruled out. Excluding the trauma subgroup, the rest are treated with careful conservative treatment, have a good prognosis and are usually self-limited and benign, which is what we observed in our patients.
Conclusions
The true definition and classification of pneumomediastinum are not in line with what has been published, which therefore causes confusion with the terminology and conceptual difficulties. The definition is incorrectly used.
The term "spontaneous" pneumomediastinum should be dropped and it should be called primary pneumomediastinum.
A primary pneumomediastinum is one which occurs without any evident causal factor (predisposing or precipitat ing); it should occur without any apparent explicable cause.
A secondary pneumomediastinum is one which occurs with an evident causal factor (predisposing or precipitating or both).
Under these conditions, primary pneumomediastinum is an extremely rare condition.
Secondary pneumomediastinum is the most frequently reported disorder.
The predisposing or precipitating factors may act alone or together; they are not exclusive.
Both types of pneumomediastinum are treated the same, except for the trauma subgroup.
Finally, a consensus would be interesting.











 text in
text in