Introduction
Twenty-eight percent of all anaphylaxis cases during medical care are mainly related to medications, the most common being antibiotics, nonsteroidal anti-inflammatory drugs (NSAIDs), opioids and contrast media, while in the ambulatory setting, the most common etiologies are foods, drugs and insect bites 1.
One of the main complications of anaphylaxis is Kounis syndrome (KS), which was described by Dr. Nicholas Kounis as an "allergic angina" in 1991, referring to an acute coronary syndrome caused by anaphylaxis due to exposure or allergenic factors, with ensuing coronary and systemic mastocyte degranulation favoring the release of histamine, leukotrienes and serotonin, leading to coronary artery spasms and potential infarction or coronary throm bosis 2,3.
Epidemiologically, the incidence of anaphylaxis and cardiovascular events has been reported to be eight to nine cases per 100,000 inhabitants per year 2. Its incidence has been estimated to range from 0.002-3.4% 3-5. This condition occurs more frequently in men (3 to 1), with those between 40-70 years old being the most vulnerable (68%), and causes an approximate mortality of 7% 4,5.
Kounis syndrome is classified in three types. Type 1 corresponds to coronary artery spasm without prior coro nary disease, type II is atheroma plaque rupture with prior coronary disease, and type III is related to stent thrombosis 3,4,6. Clinically, symptoms may range from anaphylaxis with skin involvement to sudden cardiac death; however, out of this broad range of clinical expression, chest pain occurs in 86% of cases 5. On the other hand, there is no expected pattern or specific change on the electrocardio gram, but anything may be found from sinus tachycardia or bradycardia to ST segment elevation or depression, T-wave flattening or inversion, prolonged QT interval, widened QRS, ventricular ectopy, or fatal arrhythmias like ventricular fibrillation 7. Anterior or inferior lead ST seg ment elevation has been most frequently reported; thus, the most frequently affected arteries are the anterior descending and right coronary arteries, although the reason for this is unknown 8,9. Troponin elevation is not as marked as in the usual coronary syndromes, and the echocardiogram may show dilated heart chambers and contractility disorders or generalized hypokinesia 3,7,8.
The objective of this article is to present the case of a patient with type I Kounis syndrome.
Clinical case
A 62-year-old woman consulted due to a two-day his tory of colicky abdominal pain in the right upper quadrant associated with nausea and repeated vomiting. She reported a history of essential hypertension being treated with losartan 50 mg/day and hydrochlorothiazide 25 mg/day, and a hysterectomy five years prior without complications, and denied any allergies. On physical exam, her vital signs were normal, she was alert and oriented, and Murphy's sign was positive. The ultrasound studies reported cholelithiasis plus acute cholecystitis, and she therefore underwent open cholecystectomy.
During surgery, she received prophylactic cephazolin and anesthesia was induced with fentanyl, midazolam, propofol and rocuronium, following which she developed sustained hypotension unresponsive to intravenous fluids or ethylephrine, and vasopressor support with norepinephrine was added. Towards the end of the surgical procedure, she developed a generalized rash, eyelid and facial edema, and severe bronchospasm which progressed to anaphylactic shock. She was given emergency treatment with a dose of epinephrine, corticosteroids and antihistamines, with clinical improvement and hemodynamic recovery.
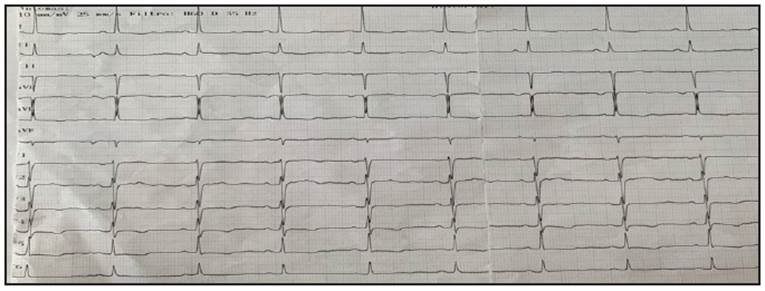
After extubation, the patient experienced oppressive chest pain along with nausea and dyspnea at rest, which did not radiate, had no aggravating or exacerbating factors and lasted approximately five minutes. Tests ruled out pleural effusion, pneumothorax, aspiration pneumonia or pulmonary embolism, and an electrocardiogram showed diffuse repolar ization changes (Figure 1). Therefore, treatment was begun with one ampule of tavegyl, 100 mg IV of hydrocortisone and 100 mg/day of acetylsalicylic acid. Futher laboratory tests were run to rule out acute coronary syndrome.
The first ultrasensitive troponin T was positive (0.002-control 0.056) with a significant delta (Table 1). No dynamic changes were found on follow up EKGs, and the echocardiogram reported a preserved ejection fraction and left ventricular hypertrophy with no contractility disorders or hypokinesia. In view of a possible type I vs. type II Kounis syndrome, invasive coronary stratification was performed with arteriography which reported healthy coronary arter ies with no atheromatosis or ulcerated plaques (Figure 2).
Table 1 Laboratory tests run during hospitalization.
| Diagnostic tests | Results | Reference |
|---|---|---|
| Creatinine (mg/dL) | 0.52 | 0.3-1.1 |
| Blood urea nitrogen BUN (mg/dL) | 10 | 8.0-20 |
| Sodium (mEq/L) | 144 | 146-157 |
| Potassium (mEq/L) | 3.21 | 3.7-5.5 |
| Plasma glucose (mg/dL) | 170 | 74-106 |
| Leukocytes (x10 3/uL) | 10.78 | 4.5-11.0 |
| Neutrophils (%) | 91 | 50-70 |
| Hemoglobin (g/dL) | 16 | 11.0-16 |
| Platelets (x10 3/uL) | 291 | 150-450 |
| Troponin 1 (ng/mL) | 0.024 | 0.0-0.3 |
| Troponin 2 (ng/mL) | 0.056 | 0.0-0.3 |
| D-dimer | 1,490 | >500 |
Type I Kounis syndrome was confirmed, probably sec ondary to the use of rocuronium; the oxygen was able to be withdrawn.
Discussion
There are no guidelines for KS at this time, and much of the data and information has been gathered from case reports. The use of nitroglycerine should be avoided be cause it can trigger tachycardia and hypotension which may further worsen the anaphylaxis 11. The recommendations are aimed at the usual treatment of an ACS, in addition to steroids and antihistamines, but it is worth noting that special care should be taken with the use of beta blockers. While these may be beneficial in an ACS, they may decrease the effectiveness of adrenaline for anaphylaxis, and therefore it may be challenging to use them 8,10,11.
Type I KS has proven to have a better prognosis than type II; the magnitude of the initial allergic response, the patient's sensitivity, comorbidities, the site of the antigen-antibody reaction and the type of allergen should be considered. The prognosis for patients with KS is very good, with complete left ventricular function recovery over the space of three days to several weeks. Death is very rare in the acute phase and is related to complications like arrhythmias, pulmonary edema and, rarely, thrombotic events. Short-term follow up with an echocardiogram at four weeks confirms the good prognosis with a low incidence of heart failure and normalized left ventricular function. No recurrences of KS have been reported, but uncontrolled, repetitive exposure to allergens may cause similar allergic reactions and allergic myocardial infarction 12.
Kounis syndrome is a low-incidence condition which is underdiagnosed due to its wide variety of symptoms with no specific clinical findings. Its inpatient mortality is not negligible, but it has a good overall prognosis. Up to 25% of patients with KS have a history of some known allergy, but as seen in most patients, and as occurred in our patient, there may be no history of allergies 14. Kounis syndrome occurs mainly in middle aged and older adults, especially those between 40 and 70 years old, with age itself being a risk factor for a greater incidence of allergic reactions due to comorbidities and cardiovascular diseases which increase with age, as well as changes in the immune system and pos sible deregulation of pro and anti-inflammatory substances which accompany aging 5,15.
Regarding the diagnosis of this syndrome, some authors recommend measuring serum tryptase levels, this being the most useful test for confirming or diagnosing anaphy laxis, together with histamine levels 9. Serum tryptase can be detected 30 minutes after the onset of anaphylaxis and reaches its highest levels within one to two hours. Therefore, serial measurements are recommended, normal levels do not rule out anaphylaxis and the clinical definition endorsed by the European Academy of Allergy and Clinical Immunology should always be used 17.
Most bibliographic sources and case series agree that a large proportion of the patients have some degree of sys tolic dysfunction and regional movement abnormalities in some heart walls, with subsequent normalization of these abnormalities. However, recovery from motility disorders may begin 72 hours after the allergic episode is identified 12,20. These changes were not found in our case, possibly due to the timing of the echocardiogram.
Conclusions
Kounis syndrome should be suspected in patients with chest pain, anaphylaxis, electrocardiographic changes and elevated cardiac enzymes. An echocardiogram and arteriog-raphy are essential for ruling out alternative diagnoses and/ or classifying the syndrome correctly. A thorough history should be taken in patients with KS, looking for the allergen or medication responsible for the allergic reaction. A his tory of allergies should be emphasized given the risk of a repeat event. The prognosis for patients with KS is good, with recovery of the systolic function and ventricular wall motility abnormalities.











 text in
text in