Introduction
Thunderclap headaches (THs) are described as sudden-onset headaches which reach their maximum intensity in less than a minute 1. They have an estimated annual incidence of 43 per 100,000 adults in developed countries 2.
Many etiologies have been identified, with the most common being spontaneous subarachnoid hemorrhage (SAH) due to aneurysm rupture. However, other less com mon causes can be found such as cervical artery dissection, venous sinus thrombosis, and pituitary apoplexy (PA), among others 1.
Pituitary apoplexy is classically described as the sudden onset of a headache accompanied by neurological and/or endocrinological impairment, commonly attributed to hem orrhage or ischemia in a pituitary adenoma 2,3.
Thunderclap headaches are highlighted among the main manifestations of PA, occurring in in approximately 73% of cases 4,5. Decreased visual acuity (68%), visual field losses (49%), and oculoparesis (48%) occur concomitantly, and up to 17% may develop altered consciousness or coma 4.
A high degree of clinical suspicion is required to diagnose it, as this condition is rare and rapidly progressive over hours or days. Thus, it should always be considered in patients with a first episode of a sudden onset or thunderclap headache 6.
Below, we discuss the case of a patient who was admitted to the emergency room for a TH as a manifestation of PA.
Clinical case
A 49-year-old male patient with no significant medical history was admitted to the emergency room for a sudden onset holocranial stabbing headache which woke him. It had a 10/10 intensity on the visual analog pain scale (VAS) and was associated with multiple episodes of vomiting food content. On admission, the patient reported that it was "the worst headache of his life." He had no visual or motor abnormalities or any other symptoms.
On the admission physical exam, his vital signs were: blood pressure: 116/68 mmHg, heart rate: 88 beats per minute, respiratory rate: 18 breaths per minute, temperature: 36.7°C, oxygen saturation 98%; no focal neurological signs, and a normal fundus exam. A simple cranial computed axial tomography (CAT) ruled out intra or extra-parenchymal hemorrhage, but showed increased pituitary tissue in the sella turcica, with a 17.5 x 17 x 16.9 mm diameter heterog enous content. A brain magnetic resonance angiography with contrast showed no evidence of vascular malformations, aneurysms or venous sinus thrombosis. Symptomatic treat ment was begun with dipirone 1 g/8 hours, metoclopramide 10 mg/12 hours, magnesium sulfate 1 g/8 hours and dexamethasone 8 mg/8 hours.
After 48 hours of analgesic treatment, the headache persisted with the same characteristics, along with myalgias and paresthesias in upper and lower limbs, and the patient became bradypsychic and hypoprosexic; all other parameters were within normal limits. Blood tests were run showing blood sugar, kidney function and albumin within normal limits, with severe hyponatremia and hyperkalemia (Table 1). Magnetic resonance imaging (MRI) of the sella turcica and base of the skull was done to study the sellar lesion, showing increased pituitary tissue volume with deepening of the sellar floor, extending to the suprasellar region, contacting and exerting mild compression on the optic chiasm and optic nerves. Signal iso and hypointensity was also documented in the T1 sequences, with nonhomogenous signal hyperintensity in T2 sequences and nonhomogenous enhancement in the contrast phase (Figure 1).
Table 1 Initial tests.
| Variables | Result | Parameter |
|---|---|---|
| Creatinine | 1.03 | 0.7-1.2 mg/dL |
| Serum sodium | 123 | 135-145 mmol/L |
| Potassium | 5.2 | 3.5-5.1 mmol/L |
| Ionized calcium | 1.03 | 1.16-1.32 mmol/L |
| Phosphorus | 3.87 | 2.5-4.5 mg/dL |
| Albumin | 4.5 | 3.5-5.2 g/dL |
| Random blood sugar | 126 | < 200 mg/dL |
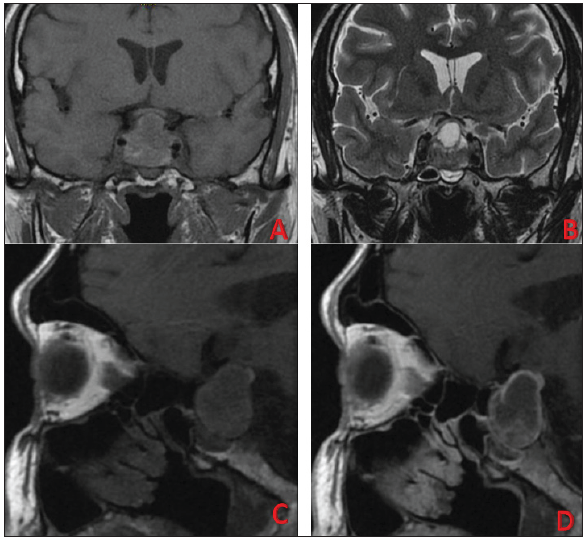
Figure 1 A. Magnetic resonance imaging, Tl sequence coronal plane, showing a heterogenous isointense suprasellar lesion with subtle internal hypointensity. B. Magnetic resonance imaging, T2 sequence coronal plane, showing a heterogenous suprasellar and sellar lesion which is mostly hyperintense but has a hypointense partitioned interior and basal portion. C. Magnetic resonance imaging, medial sagittal plane, Tl sequence, showing a heterogeneous lesion on the sella turcica which is mostly isointense with subtle interior hypointensity. D. Magnetic resonance imaging, medial sagittal plane, Tl sequence with contrast showing a heterogenous lesion over the sella turcica which is mostly isointense with subtle interior hypointensity and non-homogenous enhancement.
In light of the TH associated with enlarged pituitary tissue and abnormal neuroimages suggestive of PA, the hypothalamic-pituitary axis was assessed, finding the following: thyrotropic, corticotropic, somatotropic and gonadotropic axis hormone deficiency (Table 2). Therefore, treatment was begun with intravenous steroids at 100 mg/8 hours and hormone replacement with levothyroxine 50 mg/day, with improvement of the headache, alertness and fluid-electrolyte imbalance. The patient was discharged on levothyroxine 50 mg/day, prednisolone 7.5 mg/day and testosterone 1 gram.
Table 2 Hormone profile report. 0
| Variable | Result | Parameter |
|---|---|---|
| Testosterone | 0.39 | 4.81-22.42 pg/mL |
| Luteinizing hormone (LH) | 1.82 | 1.7-8.6 mIU/mL |
| Follicle stimulating hormone (FSH) | 1.9 | 1.5-12.4 mIU/mL |
| Somatomedin C | 54 | 74-196 ng/mL |
| Thyroid stimulating hormone (TSH) | 0.223 | 0.2-4.4 uIU/mL |
| Free thyroxine (FT4) | 0.7 | 0.9-1.7 ng/dL |
| Growth hormone | 0.219 | 0-3 ng/mL |
| Prolactin | 9.76 | 4.04-15.2 ng/dL |
| AM cortisol | 3.0 | 6.2-19.4 uIU/dL |
Two months later, a follow up MRI of the sella turcica showed a reduction in the size of the sellar lesion.
Discussion
A TH is considered to be an intolerable headache which occurs suddenly like a "thunderclap," reaches its maximum point in less than a minute, and should be considered a medi cal emergency 7,8.
It has many potential etiologies, including reversible cere bral vessel constriction syndrome, venous sinus thrombosis, cervical artery dissection, cerebral ischemia and pituitary apoplexy; however, it is mainly associated with SAH 1. In our case, the patient debuted with a headache which met the criteria for TH, and therefore a simple head CAT was performed which ruled out SAH as a possible etiology.
In the initial approach, after taking an adequate history and performing a physical and neurological exam, all pa tients with TH should have neuroimaging, initially a head CAT without contrast, given its high sensitivity for finding SAH 1.
If SAH is not found, angiographic imaging would be indicated and, based on the clinical suspicion, resonance imaging 1. In our patient's case, the angiographic images showed no arterial or venous lesions, but did show a pituitary adenoma not previously reported in the history.
Due to a high clinical suspicion of PA, an MRI of the sella turcica was ordered which, together with pituitary hormone function tests, confirmed the clinical suspicion.
Pituitary apoplexy is a rare disorder with a global inci dence ranging from 0.6-7% and increasing from 2 to 12% in patients with a known pituitary adenoma 6.
This clinical syndrome is defined by the appearance of cardinal symptoms like headache, which is probably caused by dural stretching due to mass effect, blood extravasation and necrotic tissue in the subarachnoid space causing men ingeal irritation 6. Concomitantly, there may be vomiting, visual impairment and/or a reduced level of consciousness, due to rapid expansion of the contents of the sella turcica caused by hemorrhage or infarction of the pituitary gland 9. This tends to be spontaneous, but predisposing factors can be identified in 10-40% of cases, among which high blood pressure, surgical procedures, radiation therapy and the use of anticoagulants are very important 9. In our patient, no history or predisposing factors were identified.
In addition to the cardinal symptoms, another important and potentially devastating manifestation is hypopituitarism, probably secondary to the acute increase in intrasellar pressure which constricts the circulation, the pituitary stalk and the pituitary gland itself 10. Given that the event can change rapidly from being benign to catastrophic, we highlight the importance of considering this disorder in the emergency room as a cause of THs 11.
As mentioned previously, a high clinical inference is needed along with appropriate neuroimaging, an ophthalmological exam and a complete hormone panel (with serum cortisol and thyroid hormones being especially important) 3.
ACTH deficiency has been reported to be the most impor tant due to the risk of developing adrenal insufficiency and hemodynamic instability. This occurs in more than 70% of patients, followed by growth hormone (GH) (80%), luteinizing/follicle stimulating hormone (LH/FSH) (75%), and thyroid stimulating hormone (TSH) (60%) deficiency 12.
In our patient's case, there were decreased levels of cortisol, along with ACTH deficiency and thyrotropic, gonadotropic and somatotropic axis disorders.
Due to its sudden onset, neuroimages are essential in the initial approach. It should be noted that CAT can differentiate PA in only 25-28% of cases. Magnetic resonance of the sella turcica is more sensitive and detects PA in almost 100% of the patients 3. As in our case, the CAT images ruled out hemorrhagic lesions, but sella turcica MRI documented a pituitary gland lesion with a heterogenous signal on T1 weighted images and hypointensity on T2 with a narrow peripheral border, characteristics which suggest PA as the first option 13.
For treatment, the United Kingdom Consensus recom mends that immediate transphenoidal surgery only be proposed if the patient has serious neuro-ophthalmological signs and/or a persistently altered level of consciousness. Patients with PA who do not have any of these signs and are hemodynamically stable may be considered for conservative treatment with close follow up 14.
The immediate administration of high-dose glucocorticoids may be ordered, as this covers the increased risk of hypocortisolism. In milder cases, glucocorticoid ad ministration should only be considered if the (9:00 a.m.) serum cortisol is below 550 nmol/L 10. In our patient, an initial intravenous steroid dose was ordered because he had marked hypocortisolism, and it was then continued by mouth. Hormone replacement therapy with levothyroxine was begun concomitantly. He was not considered to be a candidate for surgery since he did not have serious neuro-ophthalmological signs or altered consciousness.
During his hospitalization, the patient showed great clini cal improvement on glucocorticoids coupled with hormone supplements. He did not require surgery and, on follow up, his hormone levels had normalized and the sellar mass had decreased in size.
In conclusion, PA is a highly devastating disorder if not diagnosed early. Despite having been described more than 70 years ago, its diagnosis continues to be challenging due to its heterogeneous signs and symptoms and the fact that most patients do not have a previously diagnosed adenoma 15. It requires a high clinical suspicion for its diagnosis, and should always be considered as a potentially fatal cause of THs. This condition should be recognized together with other etiologies including SAH 2.











 texto en
texto en 


