Introduction
SARS-CoV-2 is a single-stranded RNA virus which enters the human cell by binding its surface protein to the host's angiotensin-2 converting enzyme, especially present in organs like the lungs, brain, heart, kidneys and intestine 1. The disease caused by this coronavirus is known as COVID-19, with signs and symptoms ranging from a common cold to serious manifestations characterized by a severe acute respiratory syndrome with extrapulmonary involvement caused by multisystemic vascular inflammation and endothelial damage with a high morbidity and mortality rate.
Declared a pandemic on March 11, 2020, it has caused approximately 100,382 deaths to date in Colombia, and more than three million worldwide, directly or indirectly. Its clinical significance lies not only in its high transmissibility, fostered by asymptomatic but infectious patients which account for up to 19% 2, but also in its high extrapulmonary impact, being associated with coagulation disorders, endothelial disorders, angiogenesis defects, and thromboembolic complications 3 which may manifest simultaneously, increasing the risk of fatal complications.
Several articles have shown case reports of thromboses in patients with COVID-19 infection; however, most are limited to single but not simultaneous venous or arterial thromboses. In this article, we present three different cases in which simultaneous thromboses involving both veins and arteries were documented in patients with confirmed SARS-CoV-2 infection.
Case reports
Case 1
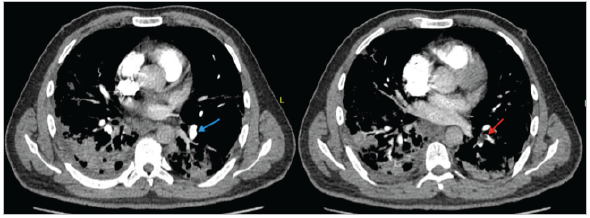
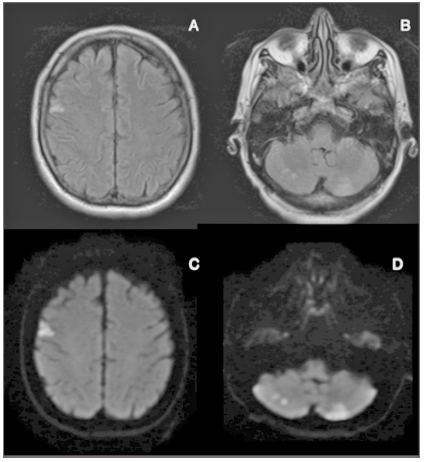
A 50-year-old man with a history of hypertension was admitted to the emergency room after two hours of right hemiparesis and dysarthria, with an admission NIHSS of eight and the following vital signs: blood pressure 190/100 mmHg, heart rate 80 bpm, respiratory rate 23 bpm, SaO2 83% and blood glucose 382 mg/dL. He underwent a simple brain MRI with evidence of right thalamic and left frontal restricted diffusion not evident on Flair (Figure 1). Treatment was begun with labetolol, which controlled his blood pressure, and thrombolysis was performed with rTPA/alteplase, with an NIHSS of one at 24 hours. The admission chest x-ray showed diffuse infiltrates in both lung fields compatible with COVID-19 infection. The initial SARS-CoV-2 RT-PCR was negative, and therefore, due to the high clinical suspicion, a confirmatory test was run the following day with a positive result. He was diagnosed with diabetes mellitus due to an HbA1C of 10%. Neurovascular examination included a Doppler of the neck vessels, an electrocardiogram and an echocardiogram, all within normal limits. After five days in the hospital, he developed pleuritic chest pain along with diaphoresis and desaturation, so an electrocardiogram was taken which showed sinus tachycardia. He had a negative troponin and the angioCT showed acute bilateral pulmonary thromboembolism in the left lower and right upper lobes (Figure 2). He was discharged after 18 days in the hospital with only mono hypoesthesia of the right upper limb as a neurological sequela, and on two liters of oxygen via nasal cannula.
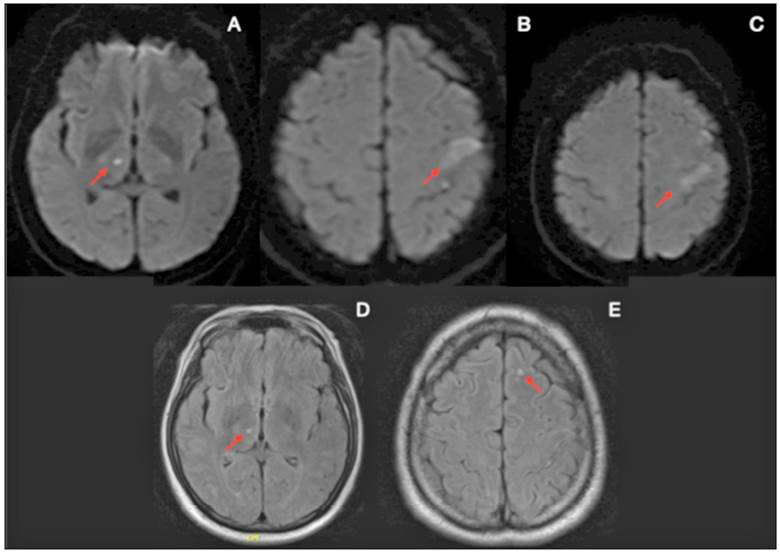
Figure 1 Case 1. Simple brain magnetic resonance in the DWI (A, B and C) and T2 FLAIR (D and E) windows showing hyperacute infarction areas in the left frontal lobe and right thalamic lacuna.
Case 2
A 47-year-old man with a history of hypertension and non-insulin dependent diabetes mellitus was admitted to the emergency room two hours after having experienced a tonic-clonic seizure with partial recovery of consciousness and de novo left hemiplegia. Vital signs on admission were: BP 153/90 mmhg, HR 100 bpm, RR 30 bpm, SaO2 70% and blood glucose 250 mg/dL. A simple head CT showed focal cortical and subcortical high left frontal and ipsilateral occipital hypodensities related to acute ischemic events, without bleeding. Therefore, a simple brain MRI was performed showing evidence of hyperacute fragmented cortical-subcortical infarcts in multiple arterial territories (Figure 3). The admission NIHSS was 23 points, and therefore thrombolysis was carried out with rTP alteplase, with a subsequent NIHSS of 21, determined to be failed thrombolysis. A COVID RT-PCR was positive.
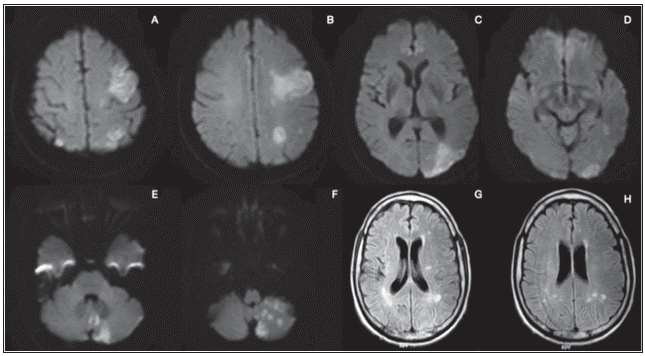
Figure 3 Case 2. Simple brain MRI in the DWI window (A - F) showing predominantly left and cerebellar cortical-subcortical hyperacute fragmented infarctions. T2 window (G and H) showing bilateral involvement with no hemorrhagic component.
After seven days in the hospital, the patient developed distal coolness in his left lower limb, diminished tibial and pedal pulses with decreased pulse amplitude and mottling of the big toe, and fourth and fifth toes of the left foot. In light of signs of microembolism, he was evaluated by peripheral vascular surgery, with no surgical or endovascular procedure ordered.
Twenty-six days after admission the patient died from respiratory failure.
Case 3
A 62-year-old male patient with no significant medical history was admitted two hours after being found with dysarthria, labial commissure deviation and difficulty standing and walking. His admission vital signs were: blood pressure 104/65, heart rate 114 bpm, temperature 36.5°C, and 77% saturation on room air. On physical exam, he had generalized rales, pain and edema in the lower limbs, and the neurological exam showed facial asymmetry due to right central paralysis and monoparesis of the left upper limb, with 4/5 strength, and an admission NIHSS of 2. A simple brain MRI showed multiple hyperacute infarcts in various vascular territories involving more than 1 cm of the cerebellum as well (Figure 4). A venous Doppler of the lower limbs showed bilateral infrapopliteal deep vein thromboses and a simple chest CT revealed severe bilateral multilobar pneumonia. One week after admission the patient had no neurological impairment and had progressively decreased his oxygen requirement to a nasal cannula.
Discussion
In its severe form, COVID-19 is a disease which causes systemic hypercoagulability which has been related to a higher chance of thrombotic events compared to other viruses which also cause ARDS in adults, such as influenza A 4. The most common complication is pulmonary thromboembolism (PTE) despite thromboprophylaxis, reaching an incidence of up to 20% documented in life, according to Fatimah et al.'s review 5, and rising to 58% in autopsies, even in patients with no prior clinical suspicion 6. Microscopic evaluations of series of autopsies have documented diffuse alveolar damage with thromboses and hemorrhage, associated with a higher risk of death 7.
The neurological signs of SARs-CoV-2 infection range from peripheral involvement through hyposmia to polyneuropathies and central involvement from headaches and dizziness to ischemic and hemorrhagic cerebrovascular events. Pathophysiologically, this infection has been associated with a viral neurotropism which fosters vascular endothelial dysfunction and degeneration 8.
Rey J et al. 9 described the case of a patient with COVID-19 with thromboses in two coronary arteries. While these were two simultaneous thromboses, they were only arterial thromboses and in a single territory: the coronary tree. Guillan et al. 10 also reported a case with multiple cerebral thrombotic episodes. The unusual thing about the cases we published in this article is that our patients had simultaneous arterial and venous thromboses: a cerebrovascular accident and pulmonary embolism in Case One, and cerebrovascular disease plus deep vein thrombosis in Case Three, which is very rare in SARS-CoV-2 infections. In addition, in Case Two we documented cerebrovascular disease and peripheral artery thrombosis. Therefore, while these are both arterial thrombotic phenomena, they are in different territories, which is completely different than the behavior of the cases published by Rey J and Guillan M.
Chakir et al. 11 reported a case of a patient with COVID-19, acute myocardial infarction, pulmonary throm-boembolism and a cerebrovascular accident. This case is similar to ours in that the thrombotic phenomena occurred in different territories, both arterial and venous. However, our patients had acute COVID-19; in the case presented by Chakir et al., the patient had a negative RT-PCR with a positive IgG and negative IgM for COVID-19, which suggests that he had had the disease previously and did not have an active infection at the time, raising doubts as to whether it was really related to the novel coronavirus infection.
In our first two cases, the initial presentation was a cerebrovascular accident. In fact, in both, thrombolysis was performed due to the patients' significant neurological involvement. Afterward, secondary prevention was provided with acetylsalicylic acid and thromboprophylaxis with low-molecular-weight heparin, with the subsequent development of new thrombotic episodes, which suggests a high thrombogenic effect of SARS-CoV-2, with a possible benefit of anticoagulation in these patients.
One patient out of the three published cases died. Although he had a cerebrovascular accident and peripheral artery thrombosis, the cause of death was linked to pulmonary complications of COVID-19 and not to complications of his thrombotic phenomena. The other two patients were discharged. The cases have been followed up and they have had no new thrombotic phenomena.
There are no specific recommendations for anticoagulation in patients with SARS-CoV-2. In the context of venous embolism, ambulatory anticoagulation was ordered with direct anticoagulants. It is worth noting that there is no evidence in patients with COVID-19 comparing vitamin K antagonists with direct anticoagulants in terms of efficacy and safety, this being an interesting point for future research.
Finally, it is important to keep in mind that all causes other than SARS-CoV-2 infection were ruled out as a causal mechanism of the thrombotic phenomena. Our patients did not have any type of thrombophilia, or any other conditions which would increase their thrombotic risk like medications, atrial fibrillation, carotid disease, patent foramen ovale or a post-vaccination status.
Conclusion
SARS-CoV-2 infection has impacted health conditions worldwide, constituting one of the main causes of morbidity and mortality in all countries. While the main COVID-19 disorder is respiratory, there is no doubt that it causes endothelial disease, leading to both arterial and venous thrombotic phenomena.
Thromboses in different vascular territories are uncommon in COVID-19 infections, with very few reports in the literature to date. However, this condition must be kept in mind and marks a starting point for future research on the potential impact of anticoagulation in patients with novel coronavirus infection who have a first episode of thrombosis, to prevent its recurrence.











 text in
text in