Introduction
According to the World Health Organization (WHO), cardiovascular diseases are the main cause of death world wide. Of these, ischemic heart disease is the most frequent, with approximately 8.92 million deaths in 2015, especially in those over the age of 55 with risk factors like hyperten sion, sedentarism, obesity and smoking, constituting a public health problem with economic ramifications for healthcare systems 1-4.
This highlights the importance of understanding the main demographic and clinical characteristics of the local popula tion with a diagnostic suspicion of this disease.
Methods
This was a descriptive, cross-sectional observational study carried out at a tertiary care hospital in Bogotá from January 2017 through December 2019, including all patients over the age of 18 who were admitted to the institution during this period with a presumptive diagnosis of acute coronary syndrome (ST-elevation acute myocardial infarction, non-ST-elevation acute myocardial infarction, unstable angina) or who had signs and symptoms suggestive of an acute coronary event while hospitalized on a general ward or in the intensive care unit, and had at least on serum troponin measurement.
The variables evaluated were age, sex, clinical symp toms, electrocardiographic abnormalities, underlying diseases, a history of exposure such as to smoking, laboratory tests (troponin, creatinine and hemoglobin), echocardiography findings (left ventricular ejection frac tion, contractility disorders), noninvasive test results sug gestive of ischemia, coronary arteriography findings and in-hospital mortality. These were selected considering the information they would provide on cardiovascular risk and the defining variables included in the universal definition of infarction 5.
Patients who were unable to undergo coronary arteriogra-phy due to their clinical condition and those who died before the invasive stratification procedure could be performed were excluded from the study.
STATA software was used for statistical analysis. The descriptive analysis was done using absolute frequencies and proportions, also employing measures of central tendency and dispersion, according to their distribution. Patients were classified according to the fourth universal definition of infarction, taking into account the classical concept of unstable angina, as defined in Table 1 5,6.
Table 1 Definition of diagnostic categories.
| Type I infarction | Clinical symptoms of ischemia, with or without electrocardiographic changes, at least one tropo nin value > p99 and delta > 20% with coronary arteriography findings of > 50% stenosis in any vessel. |
| Unstable angina | Symptoms of angina and coronary vessel obstruction, but a negative troponin value. |
| Unstable angina and a myocardial lesion A | Patients with symptoms of angina and positive troponins according to the reference value, but without a delta > 20% and evidence of coronary obstruction on coronary arteriography. |
| MINOCA (Myocardial infarction with non -obstructive coronary arteries) | Symptoms of ischemia, at least one troponin value > p99 and delta > 20%, without significant obstruction on coronary arteriography and without a trigger or evidence of oxygen supply-demand imbalance. |
| Type II infarction | Defining characteristics of type I infarction, but without obstructive findings on coronary arteriography and a triggering factor for oxygen supply-demand imbalance. |
| Myocardial injury | Patients with positive troponins, without a delta > 20% and without obstructive coronary disease findings. |
| Others | Patients with symptoms of angina, negative troponins and/or imaging findings suggestive of ischemia (TT echocardiogram, stress echocardiogram, stress test), with no obstructive lesions on coronary arteriography. |
This study was approved by the respective ethics com mittee and due to the nature of the study, informed consent was not required.
Results
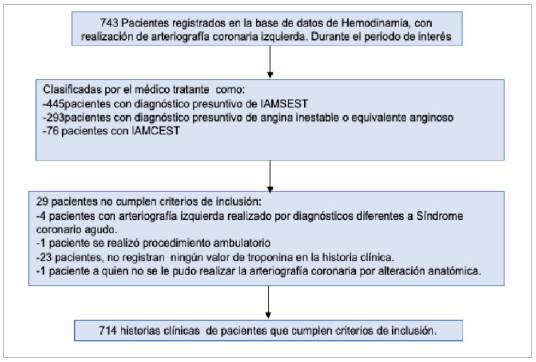
A total of 743 medical charts gathered during the period of interest were analyzed, 714 of which met the inclusion criteria. There were 459 male patients with a median age of 66 years (IQR 56-75), and 255 females with a median age of 69 years (IQR 60-77) (Figure 1).
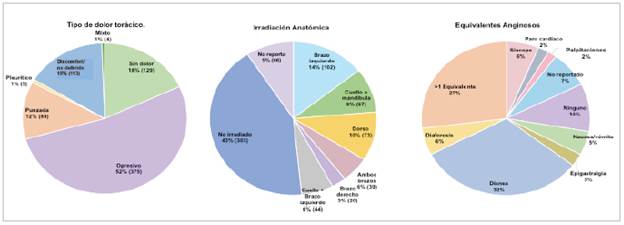
The initial clinical presentation was chest pain in 586 patients (82.1%), which was oppressive in 52.5%, followed by a feeling of chest discomfort or undefined pain in 15.8%. A total of 48.32% of patients reported radiating pain, mainly to the left arm, followed by the back and neck or jaw; 18.1% of the patients did not report chest pain as the initial symptom. In 43.7% of the cases, the duration of the pain was not reported, and for 20.3% of the patients the duration was reported to be more than 30 minutes but less than 24 hours.
Symptoms categorized as anginal equivalents or which accompanied the chest pain were mainly dyspnea in 31.8% of the patients followed by a combination of one or more of the following: dyspnea, diaphoresis, nausea or vomiting and epigastric pain (27.0%); a lower proportion only had syn cope (6%), diaphoresis (5.7%), nausea or vomiting (5.0%), epigastric pain (2.7%) and palpitations (1.7%) (Figure 2).
The most commonly found morbidities for the whole population were hypertension (64.9%), dyslipidemia (38.5%), diabetes mellitus (28.0%), prior coronary disease (24.9%) and hypothyroidism (20.6%) (Table 2).
Table 2 General characteristics of the population.
| Age | Median | IQR (p25-p75) |
|---|---|---|
| Male | 66 | 56-75 |
| Female | 69 | 60-77 |
| Sex | Frequency | % |
| Male | 459 | 64.3% |
| Female | 255 | 35.7% |
| Clinical characteristics | n | % |
| Chest pain as the initial symptom | 586 | 82.1% |
| Anatomical pain radiation | 346 | 48.5% |
| Anginal equivalents or symptoms concomitant with chest pain | 588 | 82.4% |
| Associated pathological conditions | ||
| Hypertension | 463 | 64.8% |
| Dyslipidemia | 275 | 38.5% |
| Diabetes mellitus | 200 | 28.0% |
| Electrocardiogram | ||
| Electrocardiographic abnormalities | 485 | 68.9 % |
| Normal electrocardiogram | 222 | 31.0% |
| No EKG report | 7 | 0.9% |
| Troponins | ||
| Positive first troponin | 517 | 72.4% |
| Positive second troponin | 440 | 61.6% |
| Delta > 20% | 218 | 30.5% |
| Laboratory characteristics | ||
| eGFR (mL<min/1.73 m2) stage 1 and 2 | 523 | 73.2% |
| eGFR (mL<min/1.73 m2) stage 3 - 5 | 188 | 26.3% |
| No GFR data | 3 | 0.4% |
| Echocardiogram | ||
| Contractility disorders | 357 | 50.00 |
| LVEF | ||
| > 50% | 436 | 61.1% |
| 40-49% | 126 | 17.6% |
| < 40% | 111 | 15.5% |
| Initial clinical diagnosis | ||
| NSTEMI | 445 | 62.3% |
| Unstable angina | 193 | 27.0% |
| STEMI | 76 | 10.6% |
| Artériographie findings | ||
| Obstructive lesions | 313 | 46.2% |
| Not significant | 270 | 37.8% |
| Healthy epicardial arteries | 113 | 15.8% |
| Other | 18 | 2.5% |
| Mortality | 18 | 2.5% |
| IQR: interquartile range. EKG: electrocardiogram. eGFR: estimated glomerular filtration rate. LVEF: left ventricular ejection fraction. NSTEMI: non-ST elevation myocardial infarction, STEMI: ST elevation myocardial infarction. | ||
For the obesity variable, while a frequency of 21.6% was found, body mass index was not located for 61.1% (472) of the patients, and therefore its prevalence could have been higher.
Altogether, 106 patients (14.9%) reported a history of active smoking; however, no record of length of exposure or rate of packs/year was found in 5.7% of the medical charts (41 patients).
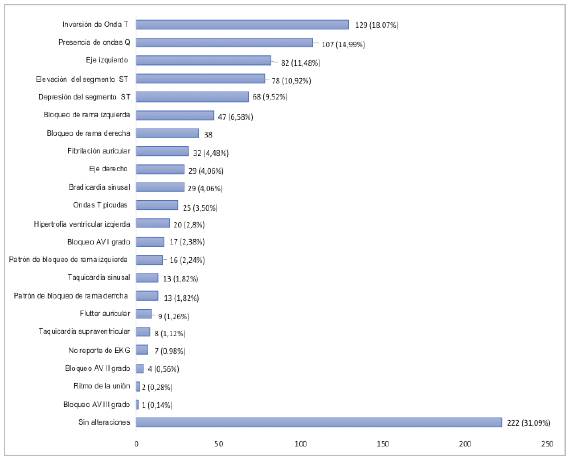
The electrocardiographic findings included symmetrical T-wave inversion in 18.1% of the patients, followed by Q waves in 15.0% and left axis in 11.5%; ST segment elevation was reported in 10.9% of the cases, 31.1% of the patients had electrocardiographic tracings interpreted as normal, and the rest of the findings are described in Figure 3.
Serum troponin was classified qualitatively (positive or negative), and delta (greater than or less than 20%) was calculated for patients with two quantitative troponin values from the same laboratory. A troponin delta >20% with an ascendent pattern was found in 22.9% of the patients and a descendent pattern in 7.6% and, since the rest of the recorded troponin values were from different laboratories, each with their own cut-off points, or only one troponin value was reported in the medical chart, delta could not be calculated for 310 patients (43.4%). Eighty-eight patients (12.3%) had negative troponin values on both draws.
The median creatinine was 0.96 mg/dL (IQR 0.79- 1.16), estimating a glomerular filtration rate of < 60 mL/ min/1.73 m2 (calculated using CKD-EPI) in 188 patients (26.3%), and documenting possible stage 5 chronic kidney disease in 24 patients (3.4%). The median hemoglobin was 14.5 g/ dL (IQR 13-15.9), finding anemia (according to the WHO classification) in 17.6% of the patients of both sexes (81 of 459 men and 45 of 255 women).
The echocardiogram reported an LVEF >50% in 436 pa tients (61.1%), and contractility disorders were found in 357 patients (50.0%). Non-invasive tests (pharmacological stress echocardiogram, exercise stress test, myocardial perfusion) were reported for 14.0% of the subjects (100 patients) prior to coronary arteriography, with 77 being positive for isch emia (77.0%) and three (3.0%) indeterminate. Since most of these tests were not performed at the institution, only the report included in the electronic medical chart was available.
The GRACE score was > 140 in 16% (115 patients), 0.07% of whom were STEMI cases. The 58.5% of the cases, and the remaining 25.4% had no score recorded in their charts. A total of 18 in-hospital deaths were found (2.5%), half attributable to type I infarctions, with the main direct cause being cardiogenic shock.
Coronary arteriography findings included the following:
Obstructive lesions (obstruction of >50% of the vessel lumen) in 313 patients (43.8%), disaggregated as follows: single-vessel involvement in 186 patients, mainly of the anterior descending artery. Double-vessel involvement in 66 patients with a predominance of the right coronary ar tery and anterior descending artery. Triple vessel involve ment in 52 patients with simultaneous obstructive lesions in the anterior descending, circumflex and right coronary arteries. Trunk disease was found in nine patients.
Non-significant lesions were found in 270 patients (37.8%).
Classification of patisnts with suspictsd acutí coronary syndroRi
Healthy epicardial arteries were found in 15.7% (113 patients).
Eighteen patients (2.5%) had other findings, mainly ecta sia, slow flow disease and non-atherosclerotic thrombotic disease.
Frequency of the different types of infarction and other diagnostic categories
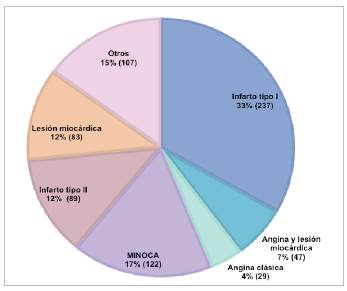
According to the criteria of the universal definition of infarction 5, the frequency of the types of infarction was as follows:
A prevalence of 33.2% (237 patients) for the type I infarction group, with 184 cases of NSTEMI (25.7%), followed by STEMI in 53 patients (7.4%). Most of the patients were men (181 vs. 56 women). Type II infarctions had a frequency of 12.5% and no cases of type III, IV or V infarctions were found. The MINOCA category had a prevalence of 17%, made up of 59 men and 63 women, followed by a 12% prevalence for the myocardial injury group. The unstable angina subgroup, according to its clas sical definition which includes negative troponins, had a prevalence of 4.1%.
Interestingly, after applying the defining concepts for the previously mentioned categories, a group of patients with anginal symptoms and elevated cardiac biomarkers without a significant delta was found, with obstructive lesions on arteriography. This group was made up of 47 patients (7%) and was termed by investigator consensus as "unstable angina and myocardial injury," without rul ing out that, due to the kinetic behavior of troponins, this group could belong to the type I infarction group, with troponins measured at a point in which the delta was less than 20% (Figure 4).
On the other hand, 107 patients (14.9%) could not be classified according to the universal definition. However, in light of their risk factors and imaging or non-invasive test findings, the clinician felt that coronary arteriography was pertinent.
Electrocardiographic abnormalities and arteriographic findings
Obstructive lesions were found on coronary arteriography in 45.2% of the 485 patients with abnormal electrocardiographic findings. Likewise obstructive lesions were found in 91 (41.0%) of the 222 patients with electrocardiograms interpreted as normal by the clinician (Figure 5). Of the 76 patients with ST elevation reported on their electrocardiograms, only 53 (69.7%) had documented obstructive coronary disease on arteriography; the remaining 23 patients belong to the MINOCA category or were not able to be clas sified according to the universal definition.

Figure 5 Electrocardiographic findings and coronary arteriography results. Relationship between the electrocardiographic tracing and coronary arteriography: of the 485patients with abnormal electrocardiographic findings, obstructive lesions were found on arteriography in 219 (45.2%). Likewise, of the 222 patients with electrocardiograms interpreted by the clinicians as normal, obstructive lesions were found in 91 (41.0%).
Troponins and arteriographic findings
Figure 6 shows the arteriographic findings according to the first troponin level: patients with a negative initial tro ponin level were more often associated with non-significant coronary tree lesions, as well as healthy epicardial arteries. Patients with a positive initial troponin one to three times above the upper limit of normal (ULN) were mostly as sociated with non-significant obstructive lesions on arteri ography, with a smaller proportion of obstructive lesions. Patients with a positive initial troponin more than three times the ULN were most often associated with significant obstructive lesions, as were patients with indeterminate positive troponin values.
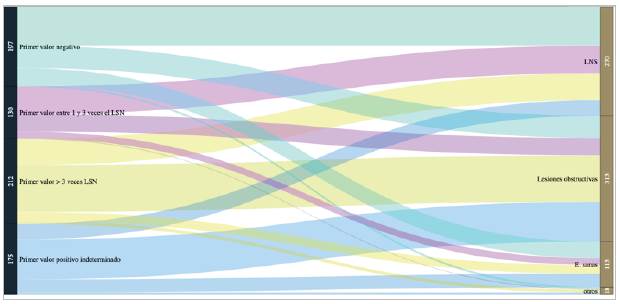
Figure 6 First troponin and coronary arteriography results. Patients with a negative first troponin level were most often associated with non-significant lesions (NSLs) of the coronary tree, as well as healthy epicardial arteries (healthy e.). Patients with a positive initial troponin one to three times the ULN were mostly related to non-significant lesions on arteriography, with a smaller proportion having obstructive lesions. Patients with an initial positive troponin more than three times the ULN and patients with an indeterminate positive troponin were mostly related with significant obstructive lesions.
Pathological conditions associated with non-ischemic troponin elevation
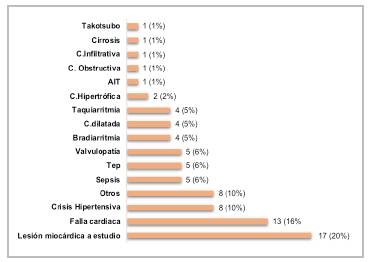
The most common etiologies of myocardial injury (elevated troponin with a delta less than 20%) were heart failure (16%), hypertensive crisis (10%), sepsis, pulmonary thromboembolism and valve disease (with a 6% frequency for each); no specific cause was found in 17 patients (20%). The rest of the findings are described in Figure 7.
The main triggers of oxygen supply-demand imbalance found for the type II infarction group were tachyarrhythmias (31.5%), sepsis (16.8%) and hypertensive crises (13.4%).
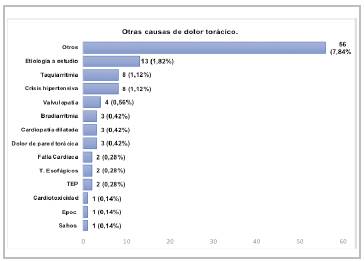
Other possible causes of chest pain
After ruling out acute ischemic diseases in 7.84% of the patients, the etiologies of chest pain included neoplasms, suspected microvascular disease, or anginal syndromes not classified in the other categories. Hypertensive crises and tachyarrhythmias triggered symptoms in 1.12% of the cases, and the causes associated with extra-cardiac disorders included chest wall pain in 0.42% of the patients, esophageal disorders in 0.28% and neuropathies in 0.28% (Figure 8).
Discussion
Acute coronary syndrome covers a group of disorders with a pathophysiological basis in endothelial inflammation which, together with arteriosclerosis, leads to coronary blood flow obstruction, causing symptoms along with biochemi cal and imaging abnormalities. Given the variety of clinical presentations, the need for early intervention in patients with hemodynamic instability, and the lack of a gold standard, international consensuses over the years have proposed different criteria for diagnosing acute myocardial infarction and its various types (as is the case of the fourth definition of infarction).
In this study, 714 medical charts of patients with a presumptive diagnosis of acute coronary syndrome over a period of three years were analyzed to identify the frequency of the different types of infarction, according to the universal definition 5. While 85.1% of the patients were able to be classified with the criteria described in this definition, 14.9% of the patients with an initial diagnostic suspicion could not be assigned to any category, which indicates the difficulty in classifying cases, due to their varied presentation.
Most of the study population consisted of men (64.3%), with a lower median age than women (66 vs. 69 years), and hypertension, dyslipidemia and diabetes as their most frequent comorbidities, as described in the Latin American epidemiology of acute coronary syndrome 7. The age dif ference has been related to the protective effect of estrogens on the vascular endothelium, with an increased incidence of infarctions in postmenopausal women 8.
Concerning the relevance of signs and symptoms within the diagnostic approach to acute coronary events, oppressive chest pain continues to be the main symptom. This study did not report anatomical pain radiation related to a higher frequency of obstructive lesions on coronary arteriography and, on the contrary, highlights the presence of symptoms interpreted as anginal equivalents in most of the patients.
The electrocardiogram was interpreted as abnormal in 68.9% of the records, with no proportional relationship found on coronary arteriography, indicating the need to consider other criteria and diagnostic aids in dealing with acute coro nary syndromes, as well as possible differential diagnoses.
Regarding the record of cardiac biomarkers, the troponin delta could not be calculated in 43.4% of the patients, as the institution is a referral center for other entities within the city and the initial results with which a patient arrives come from different laboratories, or only one troponin value is available, without a reference value. Most of the patients with obstructive lesions on arteriography were those with troponin deltas greater than 20%, indeterminate deltas, or those with an initial troponin more than three times the ULN, remembering here the importance of comparing the result with the respective cut-off point and highlighting the presence of non-ischemic etiologies in patients with mild elevations of cardiac biomarkers.
Altogether, 43.8% of the patients had obstructive lesions on coronary arteriography, of which only 33.2% were type I infarctions (mostly non-ST elevation myocardial infarc tions), with men being most affected. This finding contrasts with the data published previously by Prieto et al. in Bogotá in 2017 9, with an 82.5% prevalence, according to the third universal definition of infarctions.
Likewise, the finding of obstructive coronary disease in only 69% of the patients with ST segment elevation contrasts with the known pathophysiological principle of complete coronary artery obstruction causing these changes on the electrocardiographic tracing. This poses the need to carry out local studies to evaluate subgroups of the main risk factors, arteriographic findings and possible long-term outcomes in these patients, as described in the study by Hedvig et al., in which patients with ST elevation with and without coronary obstruction had similar mortality rates on follow up, the lat ter due to pathological conditions other than atherosclerotic burden 10.
It is interesting that 93 of the 313 patients with obstruc tive lesions on arteriography reported a history of prior coronary disease. This finding should cause concern in the different social security system actors in our country regard ing the measures implemented for follow up, modification of the natural course of the disease, and management of the individual risk of recurrence in previously revascularized patients.
Type II infarctions made up 12.5% of patients without obstructive lesions, contrasting with the literature, in which they have been reported as the cause of elevated troponins in up to 37% of hospitalized patients and 70% of those in the emergency room 11. The main associated etiologies were tachyarrhythmias, sepsis and hypertensive crises, in line with what has been reported in international studies 12. It should be noted that these patients have a greater mortality attributable to the burden of disease due their comorbidities, and a similar rate of cardiovascular events as those in the type I infarction group 12,13. In this study, two in-hospital deaths from septic shock were recorded for this category.
Another group of patients with clinical and biochemical evidence of ischemia, but without obstructive coronary dis ease findings on arteriography, was the MINOCA category. While its prevalence has been reported to range from 2 to 15% 14,15, local studies have reported a prevalence close to 19% 9, and this study found a frequency of 17.1%. A point of interest was a slight predominance of women over men at 50.1%, which differs from the epidemiology de scribed for this condition, with a known risk approximately five times greater for younger women 16 compared to type I infarction patients.
Likewise, and emphasizing patients with biomarkers elevated > p99 but with no evidence of myocardial necrosis or obstructive lesions on arteriography (for whom the fourth definition of infarction has proposed the category of myo cardial injury [5]), a frequency of 11.6% was found. Here it is interesting to note that cardiac and non-cardiac etiologies are shared with the type II infarction group (hypertensive crises, tachyarrhythmias, sepsis and valve disease).
The relevance of myocardial injuries lies in that, with the use of high-sensitivity troponins, elevations of this marker for any other reason can confuse clinicians in their diagnostic approach. This was shown in a cohort of patients published by Sandoval et al., in which, of 1,640 patients in the emergency department whose high-sensitivity troponins were measured, 30% (427 patients) had troponins > p99 and, among the etiologies of this troponin elevation, only 4.8% were due to type I infarction, 5.7% to type II infarc tion, and 17% to myocardial injury 17. Similarly, several studies have shown that having a myocardial injury from any etiology is related to an approximately 70% increase in three and five-year mortality, as well as a 30% increase in cardiovascular events during the same period18,19. This implies the need for inpatient and outpatient clinical follow up of patients with myocardial injury, even if obstructive coronary disease is ruled out.
Lastly, we highlight a group of patients with clinical symptoms and/or risk factors for whom the clinician con sidered arteriography to be pertinent, with no obstructive disease found. After the retrospective analysis of the medical charts, chest pain, cardiac and extra-cardiac diseases were identified as possible causes of the chest pain. This once more highlights the need to implement predictive models for rationalizing invasive studies as well as access to other diagnostic resources which can confirm the differential etiologies.
Among the study limitations is the fact that the data are derived from a single hospital and, since patients who due to their clinical condition could not undergo cardiac catheterization or who died prior to the procedure were excluded, the frequency of the different variables described here could be greater. Carrying out similar multicenter studies will con solidate the local epidemiology of this disease and provide the basis for timely clinical decision making.
Conclusions
Acute coronary syndrome is a common condition, presenting more frequently in males, with hypertension, dyslipidemia, obesity and diabetes mellitus as the most predominant cardiovascular risk conditions. The frequency of type I infarction, according to the universal definition of infarction, was only 33.2%; therefore, and since 56.1 % of the patients did not have obstructive lesions on arteriography, it is important to interpret the symptoms, electrocardiographic findings and cardiac biomarker kinetics in relation with other pathological conditions, not just atherosclerotic plaque rup ture, helping rationalize the diagnostic resources.











 text in
text in