Introduction
Acute coronary syndrome (ACS) is the evidence of myocardial injury manifested clinically, biochemically and/ or through an electrocardiogram, caused by coronary isch emia 1. This is the main cause of morbidity and mortality worldwide, and it is estimated that more than seven million people are diagnosed with ACS each year, including more than one million who require hospitalization in the United States for this condition 2.
Evidence of myocardial ischemia with normal or almost normal coronary arteries is a recently introduced term to describe patients with acute myocardial infarction (MI) without atherosclerotic coronary obstruction (myocardial infarction with no obstructive coronary arteries, or MI-NOCA). It is characterized by normal or almost normal arteries on coronary angiography (<50% diameter stenosis in a major epicardial vessel), being a heterogenous clinical entity with multiple causes 3,4. Between 1-13% of patients with clinical criteria for ACS correspond to MINOCA 5. If there is no apparent alternative diagnosis (for example, takotsubo syndrome, myocarditis or pulmonary embolism), the diagnosis of MINOCA is applied, which should initially be considered a working diagnosis until other causes of the clinical presentation are ruled out 6. Given the heteroge neity of causes, the prognosis is influenced by the degree of myocardial damage and the underlying etiology, with an inpatient mortality rate of 0.9% and a 12-month mortality rate of 4.7% 7.
Unlike atherosclerotic obstructive ACS, MINOCA oc curs more often in females, characteristically at earlier ages and with fewer traditional cardiovascular risk factors, which causes a morbidity and mortality problem in a previ ously healthy population 5. This entity can present with or without ST elevation on the electrocardiogram (EKG) and usually with a lower rise in cardiac biomarkers 8.
Latin American statistics have reported a prevalence of approximately 2.8%, as documented in a study performed in Argentina 9,10. On the other hand, in Colombia, an estimated 19% of patients with ACS correspond to MINOCA 11.
At a regional level, the prevalence and characteristics of patients with MINOCA are unknown, as is its short and medium-term course. Therefore, the objective of this study was to identify the demographic, clinical, paraclinical, electrocardiographic, echocardiographic angiographic and therapeutic characteristics, as well as the adverse outcomes at six months and one year, of patients with MINOCA at a tertiary care center in a Colombian city during 2019 and 2020.
Materials and methods
This was a cohort, analytical observational study evaluat ing time-to-event in patients with a diagnosis of MINOCA. The population is the set of patients diagnosed with MI NOCA at a tertiary care center in a Colombian city during 2019 and 2020. Patients 18 years old and older at the time of admission to the emergency room, with a diagnosis of MI as defined in the fourth universal definition of MI (clinical and biomarker criteria and/or electrocardiographic changes) 12 and who had undergone coronary catheterization show ing ≤50% obstruction or no obstruction of an epicardial vessel, were included. Individuals in whom the ACS event was triggered or accompanied by a significant comorbidity such as a traffic accident, trauma, gastrointestinal bleeding, surgery or a procedure, and those who had the acute coronary event after being hospitalized, were excluded. The primary outcome was the composite of hospitalization for angina or heart failure, reperfusion therapy, death from a cardio vascular cause and death from any cause. The independent variables were sociodemographic, clinical, paraclinical, electrocardiographic, echocardiographic, angiographic and therapeutic. At six-month and one-year follow up, telephone calls were made to inquire about the primary outcome vari ables, with subsequent confirmation in the medical chart. This study took into account the bioethical aspects covered by Colombian law. Thus, Resolution 008430 of 1993 was considered, which establishes the scientific, technical and administrative parameters for health research.
A general descriptive analysis of the collected data was performed. Continuous quantitative variables were sum marized using means and standard deviations if they were normally distributed; variables which did not meet the as sumption of normality were described using medians and interquartile ranges. Both ordinal and nominal categorical variables were described using absolute and relative frequen cies. In addition, multiple regression or generalized linear models were used to evaluate the association between one outcome variable and other variables of interest. Regarding the time-to-event analysis, a complete survival analysis was proposed (Kaplan-Meir estimators, Cox regression) for the question of interest.
Results
Altogether, between January 1, 2019, and December 31, 2020, 1,500 coronary arteriographies were reviewed to select the records which met the angiographic criteria of a MINOCA diagnosis (Figure 1). A total of 292 heart catheterizations compatible with MINOCA were found, of which 163 patients met the inclusion criteria and were incorporated in the study. Forty-one medical chart records were not found, and 88 patients were eliminated because they met the exclusion criteria.
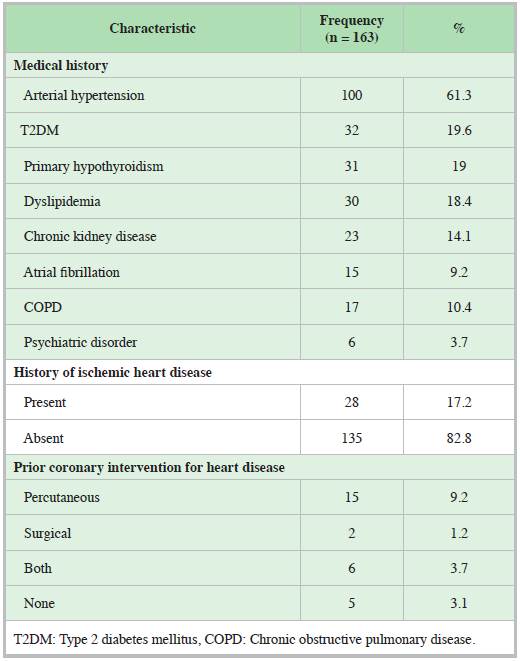
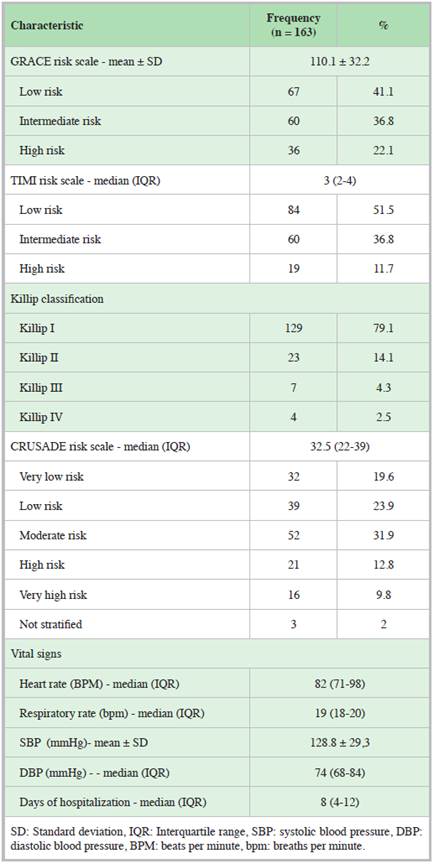
There was a slight predominance of males. The sociodemographic characteristics are summarized in Table 1. Arterial hypertension (HTN) was the most prevalent comorbidity, followed by type 2 diabetes mellitus (T2DM), hypothyroidism and dyslipidemia. Other background factors are described in Table 2. Most of the records were classified as low risk on the GRACE and TIMI scales. The risk of bleeding according to the CRUSADE scale was predomi nantly moderate. The median length of hospital stay was eight days (IQR 4-12). The remaining clinical characteristics are described in Table 3.
The most frequent EKG abnormality was an inverted T wave, which was present in 29.7% of the patients (n=47), followed by paroxysmal supraventricular tachycardia (n=28; 17.6%) and ST segment abnormalities due to its elevation (n=18; 11.4%) or depression (n=16; 10.1%). Less frequently, there was a significant Q wave (n=12; 7.6%), right bundle branch block (RBBB) (n=10; 6.3%) and atrial fibrillation (AF) with rapid ventricular response (n=9; 5.7%). Ventricu lar tachycardia (n=5; 3.1%) and left bundle branch block (LBBB) (n=5; 3.2%) were the least common findings.
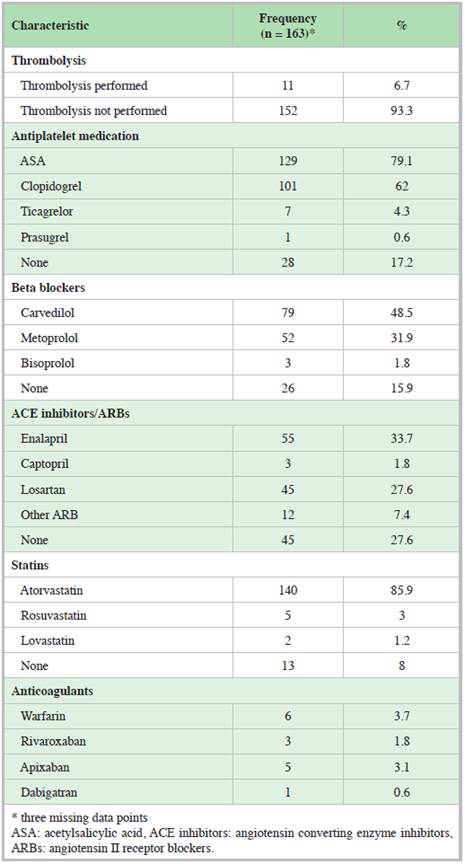
Preserved LVEF (>50%) was most frequent, occurring in 133 patients (81.6%). The most common valve disease (moderate to severe) was aortic regurgitation (n=11; 7.0%), followed by mitral regurgitation (n=9; 5.7%). The median initial troponin T was 0.03 ng/dL (IQR 0.02-0.09) for a normal reference value <0.014 ng/dL, and a follow up troponin T of 0.06 ng/dL (IQR 0.03-0.13). The median change (delta) in the serial troponin T values (rise or fall) was 49.5% (IQR 22.5 164.1). Regarding the pharmacological treatment ordered at hospital discharge, 82.8% of the patients were discharged on some type of antiplatelet medication. Other therapeutic characteristics at discharge are described in Table 4.
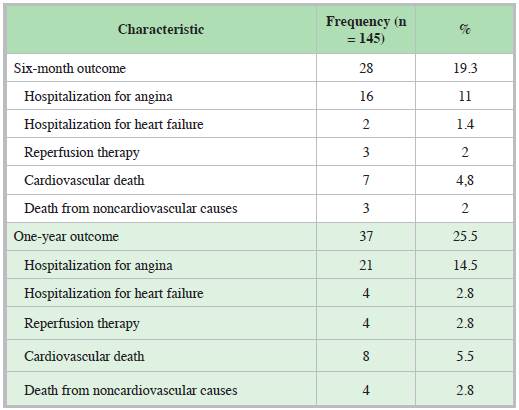
Follow up data were not obtained from 18 patients (11%) due to a lack of further records in the medical chart and the inability to make telephone contact. The most frequent outcome at both six months and one year was hospitalization for angina (Table 5).
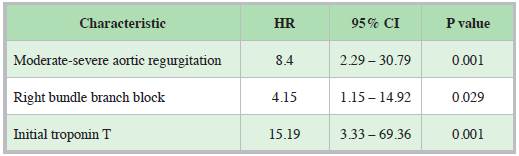
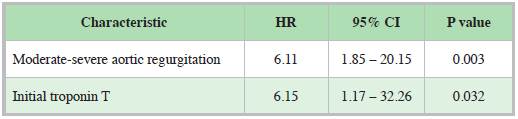
The factors associated with the outcomes on bivariate analysis were the following: at six months: age, sex, moder ate to severe aortic regurgitation or stenosis, RBBB, initial troponin T level, HTN, T2DM, dyslipidemia and a prior history of ischemic heart disease. At one year: age, sex, place of origin, alcohol consumption, CRUSADE scale score, initial troponin T value, days of hospitalization, moderate to severe aortic regurgitation, HTN, T2DM, dyslipidemia, a prior history of ischemic heart disease and RBBB.
On bivariate analysis, the presence of AF behaved as a protective factor for having an outcome at six months, as no patient with this history had an outcome at six months, compared with 28 patients who did have the outcome (OR 0.79 95% CI 0.72-0.86; p= 0.012).
Regarding the individual components of the outcome at six months, patients who died from non-cardiovascular causes during this time were found to have been hospital ized for almost twice as many days as those who did not have the outcome: 17 days [interquartile range (IQR) 15-26] and eight days (IQR 4-11), respectively, with a statistically significant difference (p=0.013). There was also a differ ence in non-cardiovascular death at one year and days of hospitalization, as those with the event had a median of 16 days (IQR 9-30.5) of hospitalization compared with those who did not have this event, with a median of eight days (IQR 4-11) of hospitalization (p=0.042).
According to the pharmacological treatment ordered at discharge, the bivariate analysis showed that using an angiotensin II receptor blocker (ARB) other than losartan was associated with a reduction in the outcomes at six months (OR 0.78 95% CI 0.71-0.86; p=0.019). A difference was found favoring enalapril in terms of hospitalization for angina at six months and non-cardiovascular death at one year, but statistical significance was not reached (p=0.084 and p=0.123, respectively).
A multivariate analysis was conducted using Cox regres sion models with the variable of outcomes at six months (Table 6) and one year (Table 7). The variables found to be associated with the outcome at six months were moderate to severe aortic regurgitation, the initial troponin T value and RBBB; and at one year, moderate to severe aortic regurgitation and the initial troponin T value.
Discussion
Different studies have described a predominance of females in MINOCA 13-16. One of the largest systematic reviews of MINOCA was published by Sivabaskari et al.7 in the journal Circulation in 2015, reporting a higher prevalence in women, with a younger age at presenta tion (average age 55 years) compared to atherosclerotic obstructive MI which has a higher incidence in men and a higher median age 5. The current study found a similar proportion of men and women, with a slight preponderance of males, noting a difference in the gender distribution. However, this finding was consistent with what was described in the Subanalysis of the CONAREC XVII Registry in Argentina by Cristian Rossler et al. (2021) 10, whose population is more similar to that of our study, which also found more men (69.7%) than women.
Only one study has been published in Colombia char acterizing patients with MI without coronary obstructive disease, carried out in Bogotá and published by Rojas et al. (2017) 11, in which they also found a significant predomi nance of men (4:1 male to female ratio). The median age in the current study was 64 years, and although this is higher than what was reported in Sivabaskari et al. 's systematic review 7 and the Bogotá registry (average of 58 years) 11, it is similar to what was described in the CONAREC XVII Argentinian registry 10, in which they found an average age of 64.5 years. These similarities in the distribution of sex and age at presentation, comparing the Latin American study with our own, propose the hypothesis of whether there are differences in the presentation of MINOCA in the Latin American population compared with countries on other continents.
The traditional cardiovascular risk factors which are often found in atherosclerotic obstructive MI have been reported less frequently in MINOCA in some studies 17,18; these include the MINOCA state of the art published by Bertil Lindahl et al. (2021) 6 and the Virgo study 16. In contrast to what has been described, the current study found a higher frequency of these risk factors. This phenotype has also been described in some publications which report a similar prevalence both in MINOCA and in obstructive MI. Thus, HTN was found in more than half of the patients (62% also had HTN in the Bogotá registry 11), T2DM in 19.6%, but a low prevalence of dyslipidemia (18.4%), very similar to the findings described in the 2015 systematic review 7 in which the prevalence was 44, 13 and 21% para HTN, T2DM and dyslipidemia, respectively.
Curiously, the current study is the only one that has found a history of AF as a protective factor in MINOCA. This being a prior history of AF rather than a de novo diagnosis in the context of MINOCA (that is, a new finding on the admission EKG), it creates the hypothesis of whether anticoagulation in patients with a history of AF may produce a protective effect in those who develop MINOCA.
The median length of hospitalization is double what has been described in Latin America 10, Korea 19, Portugal (20) and the COAPT study 21. This result is concerning for three reasons: first, those who died from non-cardiovascular causes at six months spent more than twice as many days hospitalized compared with those who did not have this out come; second, in the individual outcomes it was found that patients who were hospitalized for heart failure at one year had been hospitalized for more days during the MINOCA event than those who did not have the outcome; and third, there was a difference in non-cardiovascular death at one year and days of hospitalization. There are no studies investigating the length of hospital stay in MINOCA compared with outcomes. However, these bivariate analysis findings highlight the need to promote a shorter hospital stay in patients with MINOCA.
The most common electrocardiographic presentation in MINOCA is NSTEMI and it accounts for more than half of the patients in almost all the series 22. A systematic review and meta-regression published in 2020 by Francesco Pelliccia et al.23 included 44 and found that NSTEMI occurred in 57% of the cases; in the 2015 systematic review it was 67% of the cases 7, in the Virgo study it was 79% 16 and in the Eggers et al. study it was 76.2% 24. These findings are consistent with what was shown in the current study, in which 86.5% (n=141) of the patients had NSTEMI. A single study reported STEMI as the predominant manifestation of MINOCA 10.
The initial troponin T value (on hospital admission) was significantly related to the probability of having outcomes at six months and one year, mainly due to a significantly greater risk of cardiovascular death. This is similar to what was reported in the study by Ciliberti et al. (2018) 25, where the authors found that the maximum troponin value was significant for predicting MACE (p=0.09); however, the level of statistical significance used in this study was p=<0.10.
After a multivariate adjustment for possible confounding variables, the initial troponin T level continues to behave as a risk factor for outcomes at six months and one year. The troponin value in MINOCA as an important prognostic marker had already been reported previously; for instance, in a record-based cohort study published by Hjort et al. (2018) 26. The authors used data from 1,639 patients with MI-NOCA in Swedish hospitals from 2009 to 2013, and in their adjusted analyses, the troponin T level (high-sensitivity assay Elecsys® Troponin T, Roche Diagnostics, Basel, Switzerland) in patients with MINOCA predicted all-cause mortality (HR 1.32; 95% CI 1.11-1.56), cardiovascular mortality (HR 2.11; 95% CI 1.51-2.96) and MACE (HR 1.44; 95% CI 1.20-1.72).
In our study, preserved LVEF (>50%) was most common, occurring in 81.6% (n=133) of the records, a finding similar to what was described in the various series which report a preserved LVEF ranging from 72.4% to 91.8% 20,24.
Two valve diseases related to some components of the outcome at six months and one year were documented, with this study being the first to report these statistically significant differences, especially greater cardiovascular mortality at six months and one year for moderate to severe aortic regurgita tion, and only at six months for moderate to severe mitral regurgitation. After adjusting the multivariate analysis, aortic regurgitation continued behaving as a risk factor for outcomes at six months, a finding not reported in previous studies.
The study by Vijay S. Ramanath et al. (2010) carried out at the University of Michigan with 123 patients with MINOCA 27 was one of the first to report that patients with MI without significant obstruction had less probability of having medi cations prescribed for secondary prevention, finding fewer prescriptions compared with obstructive MI. These findings are very similar to the current study's, except for a greater prescription of dual antiplatelet therapy (DAPT) due to more prescription of P2Y12 inhibitors and statins.
The only drug group which showed a significant differ ence on bivariate analysis in this study was the use of an ARB (other than losartan), which showed a reduction in six-month but not one-year outcomes. This was the first study to show this result, compared with prior records, a finding which sug gests the need to evaluate different ARBs in the context of MINOCA in future studies.
The multivariate analysis found no relationship between the outcomes and pharmacological treatment. The evidence for MINOCA treatment has been very controversial. The benefit of ACE inhibitors/ARBs and statins has been shown previously 28-30, as in the study by Choo EH et al. (2019) 31. In a multivariate model, its authors found that the use of renin-angiotensin system blockers (HR, 2.63; 95% CI, 1.08-6.25; P=0.033) and statins (HR, 2.17; 95% CI, 1.04-4.54; P=0.039) was associated with lower mortality in patients with MINOCA. In our study, we found a beneficial tendency with enalapril in hospitalization for angina at six months and non cardiovascular death at one year, but this was not statistically significant.
For beta blockers, the data have been more heterogeneous; most observational studies do not support an overwhelming benefit in MINOCA 25,32. The study by Pelliccia et al.23 found a direct relationship between higher mortality and the use of beta blockers on patient follow up (p=0.010; coef ficient: 0.000; 95% CI: -0.000 - 0.001). However, Ciliberti et al. (2021) 33 recently published a study promoting the use of beta blockers in MINOCA, as a benefit was found in their multivariate analysis with the use of these medications (HR 0.49, 95% CI, 0.31-0.79, p=0.02).
No observational study has found a benefit in dual anti platelet therapy after a MINOCA, and most of the results have shown a neutral effect 6,18,23,28. On the contrary, a post hoc analysis of the Clopidogrel and Aspirin Optimal Dose Us age to Reduce Recurrent Events-Seventh Organisation to As sess Strategies in Ischaemic Symptoms (CURRENT-OASIS) clinical trial published in 2021 by Matthias Bossard et al. (34) compared high doses (day 1: 600 mg, days 2-7: 150 mg, then 75 mg per day) versus the standard dose (day 1: 300 mg, then 75 mg/day) of clopidogrel and reported that dual antiplatelet therapy based on clopidogrel, even at the standard dose, does not appear to provide any additional benefit, and may even harm patients with MINOCA. A higher risk of adverse events has even been reported in those on aspirin monotherapy (HR 2.47, 95% CI, 1.05-5.78, p=0.04) 33.
The pathophysiology of MINOCA, and especially the lack of obstructive coronary lesions, initially suggested the hypothesis that MINOCA was a benign condition. However, over the last few years, different published studies have re futed this hypothesis and have proven that its outcomes are not good compared with individuals without MINOCA 5. Various registries have reported a 12-month mortality rate from any cause of 4.7% (2.6-6.9%) 7, 5.3% in the COAPT study (2018) 21 and 5.5% in the Portuguese registry 20. These findings are similar to those documented in the current study, with a one-year cardiovascular mortality of 4.8% (n=7).
Evaluating the rest of the outcomes, Bugiardini et al. (2006) 35 reported the presence of the primary outcome (composed of death, MI, revascularization, unstable angina or cerebrovascular disease) in 12.1%, compared with 25.5% of the patients in our study who had the outcome at one year, with unstable angina in both studies (10.1%) and hospitalization for angina in our study (14.5%, n=21) being the most frequent outcome, and more patients undergoing revascularization in our registry (0.8 and 2%, respectively).
A high prevalence of angina following MINOCA has been reported, as revealed by the study published by Lichtlen P et al.36 in which chest pain persisted in 81% of the patients with MINOCA after an average of 10.3 years. In our study, the most frequent outcome both at six months and one year was also chest pain, but evaluated in terms of hospitalization, which occurred in a total of 21 patients (14.5%). Therefore, studies with more follow up are needed to characterize the persistent chest pain in patients with MINOCA and thus determine diagnostic, therapeutic and preventive strategies in this population.
The multivariate analysis in the current study did not show a relationship between the outcomes and the ejection fraction, as has been described in previous studies 37, for example in Pelliccia et al. 's23 meta-regression, in which there was an inverse relationship between long-term mortality and the ejec tion fraction (p < 0.0001; coefficient: -0.001; 95% CI: 0.000 0.001). In this multivariate analysis, we found that RBBB was a risk factor for developing an outcome at six months, with this being the first study to report this finding. The fact that some patients with a history of MI and ischemic heart disease were included may have contributed to this finding, as these situa tions condition structural abnormalities which can predispose to RBBB. The prevalence of prior MI in other series varies, depending on the source consulted, and ranges from 1.8% (35) to 14% 5. In the current study, there were 28 patients with a history of ischemic heart disease (17.2%), a condition which has been excluded in some studies but which we decided a priori to include in this article, since the presence of stents and/or permeable bypasses on coronary arteriography does not exclude a MINOCA diagnosis. One of the studies which included a history of coronary intervention was the Korean MI Registry (KAMIR) 19 in which 16.2 and 2.3% of the patients had a history of surgical and percutaneous revascularization, respectively, with a prevalence of prior MI (20.5%) even greater than that reported in the current study (17.2%).
One of the strengths of this study lies in finding healthy coronary arteries (0% stenosis) in more than half of the pa tients (n=108; 66.3%), in contrast with what was described in the review by Francesco Pelliccia et al. (2020) 23, the Portuguese cohort 20 and the Argentinian registry 10, which reported coronary arteries with no lesions in 46, 41.1 and 26.7%, respectively. In our study, fewer patients had <30% (n=3; 1.8%) and 30-50% (n=52; 31.9%) stenosis. An other strength of the study is that it was carried out after the publication of the latest guidelines for MINOCA diagnosis ac cording to the fourth universal definition of infarction (2018) 12, and therefore takotsubo syndrome, myopericarditis and pulmonary embolism were excluded from MINOCA, this be ing the first study in the region to characterize the population according to the latest definitions.
The inclusion of patients with <50% coronary obstruc tion could be considered a limitation of the current study. The reasons for including 50% stenoses (and not just up to 49%) are described below. First, <50% stenosis, which has traditionally been the threshold consistent with angiographic guidelines 38, has been selected arbitrarily and the wide intra and inter-observer variability in the visual estimate of stenoses during angiography is recognized 5. Therefore, a value reported as a 50% obstruction could be lower (49% or less) and be MINOCA. Second, considering the dynamic pathophysiology of MI, significant angiographic changes can be documented in the same patient due to the presence of a changeable thrombotic mass or bleeding from an unstable coronary plaque or due to fluctuations in coronary vasomo tor tone 39, which can lead to inaccurate visual readings of coronary stenoses.
The unavailability of cardiac magnetic resonance imaging, functional tests, coronary vasospasm tests and intravascular coronary imaging in this setting is a second limitation of our study. However, the first thing to keep in mind is that a large percentage of patients (8-73%) remain without an etiological diagnosis even after undergoing these studies, and even cardiac magnetic resonance imaging may not show a localized area of infarction through late gadolinium enhancement 5,6,40. Intravascular coronary imaging using optic coherence tomography (OCT) or intravascular ultrasound (IVUS) plays a fundamental role in MINOCA, as these studies clarify the etiology with greater diagnostic precision and in a higher number of patients 6,41, since coronary angiography is restricted in its capacity to elucidate the etiology and evalu ate the arterial wall. Furthermore, it is advisable to state that the transverse area of a vessel may be preserved despite the presence of a large plaque, a condition which may not be documented during angiography, and which is known as Glagov's theory (described by Dr. Glagov et al. in 1987) 42.
Another limitation of the study is the presence of informa tion and recall bias. These biases were minimized as much as possible through confirmation of the data provided by the patients using the medical charts.











 texto en
texto en