Introduction
Opportunistic infections (OIs) are an important cause of morbidity and mortality, especially in severely immunocompromised people 1-3. Patients with HIV infection who have a low CD4+ T cell count may develop a variety of OIs with a significant impact on their wellbeing, quality of life, medical care costs and survival 4. In regions like North America, Europe and Australia, Pneumocystis jirovecii pneumonia (PJP), Kaposi sarcoma (KS), esophageal candidiasis, cytomegalovirus (CMV), and disseminated Mycobacterium avium complex (MAC) infection and related disease were the prevalent OIs prior to the antiretroviral therapy (ART) era 5,6. In developing regions, the predominant HIV-related OIs prior to the introduction of ART were tuberculosis (TB), candidiasis, infectious diarrhea, bacterial meningitis and recurrent herpes simplex infections 7,8.
The substantial decrease in OIs with the introduction of ART is evident; however, there are significant differences in the burden of OIs between high-income and limited resource settings. It is important to have information on the reasons for hospital admissions among HIV patients and the type of OIs related to the CD4+ T cell count, in order to improve our clinical practice and favor early diagnosis, the use of empiric therapies and timely targeted therapy, considering that the described epidemiological changes entail different empirical coverage to what is currently used, which can also be influenced by geographic location.
Methodology
This was an observational, descriptive study with retrospective data collection. Adult hospitalized patients with an HIV/AIDS diagnosis and a history of OIs, or at least one OI at the time of admission, from January 1, 2018, to January 1, 2019, were included. The data were taken from the medical chart database at our institution. Those under the age of 18, pregnant women, those with incomplete medical charts, and cases without a confirmed or presumptive diagnosis of OI were excluded. The sociodemographic conditions, clinical characteristics, reasons for hospitalization, type of OIs and cancers were determined, as well as immunovirological markers (CD4+ T cell count and HIV viral load). The study was approved by the Research and Ethics Committee at Hospital Universitario del Valle (HUV). Body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters (kg/m2).
For the initial analysis, BMI was stratified according to the WHO criteria: <17 kg/m2 (moderate to severe undernutrition), 17 to <18.5 kg/m2 (mild undernutrition), >18.5-25 kg/m2 (normal nutrition) and > 25 kg/m2 (overweight and obesity) 9. The definitions of HIV infection/AIDS, opportunistic infections and HIV/AIDS-related cancers were those established by the United States Centers for Disease Control and Prevention (CDC). De novo HIV was defined as those diagnosed for less than three months. The current European definition of late diagnosis (LD) in an individual is a CD4+ T cell count of less than 350 cells/mm3 and/or an AIDS-defining illness at the time of diagnosis (10, 11). We chose to use WHO's definition of LD: a CD4+ T cell count under 200 cells/mm3 or a WHO clinical stage 3 or 4 at the time of diagnosis 12.
Imaging (radiology, tomography), microbiological (Gram, India ink, Cryptococcus capsular antigen, Ziehl-Neelsen, cultures), serum (VDRL), enzyme (ADA) and histopathological methods allowed the diagnosis of OIs. Studies of lavage and brushing samples were performed in the microbiology laboratory, including Gram, KOH, India ink, Ziehl-Neelsen, aerobic, fungal and mycobacterial cultures, as well as molecular biology for Mycobacterium tuberculosis (MTB) and cytomegalovirus. The pathology laboratory processed histopathology and cytology studies using immunohistochemistry, Ziehl-Neelsen, and PAS stains, along with molecular biology studies. For mycobacterial infection diagnoses, direct stains for acid-alcohol fast bacilli were performed, like Ziehl-Neelsen and modified Ziehl-Neelsen, along with Mycobacterium cultures and PCR for MTB. Sample seeding for microbiological isolation during the study period was done on solid culture medium (in duplicate for each sample).
To improve sensitivity, molecular identification tests for MTB were run using the Abbott m2000 Real Time MTB® detection test. To determine the disease stage, the most commonly used system is the CDC>s 1993 revision which substitutes the 1986 classification:
Clinical category A applies to primary infections and asymptomatic patients with or without persistent generalized lymphadenopathy (PGL).
Category B applies to patients with symptoms of diseases which do not belong to category C, but are related to HIV infection (oral candidiasis; persistent vulvovaginal candidiasis; cervical dysplasia; fever or diarrhea for more than one month; oral hairy leukoplakia; herpes zoster; immune thrombocytopenia; listeriosis; pelvic inflammatory disease; peripheral neuropathy).
Category C includes patients who have the diseases included in the AIDS-defining illnesses. Patients in categories C1, C2, C3, A3 and B3 are considered to have AIDS 13.
Results
A sample of 444 patients with an HIV diagnosis was obtained during the study period, after applying the exclusion criteria; 190 patients had HIV infection with at least one OI (Figure 1). Of the observed population, 65.3% were men, with a median age of 37 years (29.0-46.0), and 35.5 years (31.2-43.0) for women. Altogether, 81.6% of the patients were from Valle del Cauca Department, and 5.3% were from Cauca Department.
The patients' most common nutritional status was severe undernutrition, with 37.9%; we found an adequate nutritional status in 23.2% of the cases (Table 1). A total of 45.8% of the patients had been diagnosed for less than three months (de novo), and 69% of the cases had a late diagnosis (CD4+ T cell count less than 200 cells/mm3). Of the patients with a prior HIV diagnosis, only 7.76% were found to use OI prophylaxis.
Table 1 General characteristics of the population.
| Variables | Female | Male | General |
|---|---|---|---|
| Sex | 66 (34.7) | 124 (65.3) | 190 |
| Age | 35.5 (31.2 - 43.0) | 37.0 (29.0 - 46.0) | 37.0 (30.0 - 44.8) |
| Place of origin | |||
| Valle | 57 (86.4) | 98 (79.0) | 155 (81.6) |
| Cauca | 2 (3.0) | 8 (6.5) | 10 (5.3) |
| Nariño | 2 (3.0) | 4 (3.2) | 6 (3.2) |
| Other | 5 (7.6) | 14 (11.3) | 19 (10.0) |
| Time since diagnosis | |||
| Novo | 26 (39.4) | 61 (49.2) | 87 (45.8) |
| Less than one year | 9 (13.6) | 18 (14.5) | 27 (14.2) |
| 1 - 5 years | 11 (16.7) | 17 (13.7) | 28 (14.7) |
| 5 - 10 years | 10 (15.2) | 14 (11.3) | 24 (12.6) |
| More than 10 years | 10 (15.2) | 13 (10.5) | 23(12.1) |
| Vertical | 0 | 1 (0.8) | 1 (0.5) |
| Nutritional status | |||
| Adequate | 20 (30.3) | 24 (19.4) | 44 (23.2) |
| Mild undernutrition | 0 | 1 (0.8) | 1 (0.5) |
| Severe undernutrition | 17 (25.8) | 55 (44.4) | 72 (37.9) |
| No data | 29 (43.9) | 44 (35.5) | 73 (38.4) |
The CD4+ T cell count was less than 200 cells/mm3 in 86.8% of the cases, with a count lower than 50 cells/mm3 in 54.7% of the patients, 50-100 cells/mm3 in 17.4% of the cases, and only 2.1% of the patients having a CD4+ T cell count over 500 cells/mm3. In 8.4%, the HIV viral load (VL) was undetectable, and in 8.9%, the VL was not reported in the chart (Table 2). Regarding their initial classification, C3 was the most frequent stage, with 87.8% of the cases.
Altogether, 42.1% (80) of the patients were on ART, but only 31% of these adhered to the instated treatment; among the patients who had ART ordered, the two most frequently used schemes were a combination of a non-nucleoside reverse transcriptase inhibitor (NNRTI) and two nucleoside reverse transcriptase inhibitors (NRTIs), and a combination of two NRTIs with a potentiated protease inhibitor. One hundred sixty-five patients (86.8%) had had an OI on their last recorded hospitalization.
Table 2. Virological and immunological status.
| Variables | Female | Male | General (%) |
|---|---|---|---|
| Stage on admission | |||
| C1 | 2 (3.0) | 2 (1.6) | 4(2.1) |
| C2 | 13 (19.7) | 8 (6.5) | 21 (11.1) |
| C3 | 51(77.2) | 114 (91) | 165 (86.8) |
| Viral load (Copies/mL) | |||
| 50 - 10,000 | 6 (9.1) | 18 (14.5) | 24 (12.6) |
| 10,000- 100,000 | 14 (21.2) | 37 (29.8) | 51 (26.8) |
| 100,000 - 500,000 | 17 (25.8) | 29 (23.4) | 46 (24.2) |
| More than 500,000 | 15 (22.7) | 21 (16.9) | 36 (18.9) |
| Undetectable | 8(12.1) | 8 (6.5) | 16 (8.4) |
| No data | 6 (9.1) | 11 (8.9) | 17 (8.9) |
| Count (CD4 cells/mm3) | |||
| Less than 50 | 31 (47.0) | 73 (58.9) | 104 (54.7) |
| 50 - 100 | 9 (13.6) | 24 (19.4) | 33 (17.4) |
| 100 - 200 | 11 (16.7) | 17 (13.7) | 28 (14.7) |
| 200 - 500 | 13 (19.7) | 8 (6.5) | 21(11.1) |
| More than 500 | 2 (3.0) | 2 (1.6) | 4(2.1) |
The most common OIs in the whole group were tuberculosis with 28.4%, pneumocystosis with 27.9%, and toxoplasmosis with 27.4%; oral candidiasis, histoplasmosis and crypotcoccosis were reported in 4.2%, 11.1%, and 11.6%, respectively. The least common OIs were CMV with 3.7% and MAC with 0.5% of the cases (Table 3). Altogether, 223 OIs were recorded, with 48 patients having more than one OI; in this group, the most frequent associations were his-toplasmosis associated with pneumocystosis, tuberculosis associated with pneumocystosis, and tuberculosis associated with toxoplasmosis.
Table 3 Opportunistic infections.
| Variables | Female | Male | Total |
|---|---|---|---|
| Type of presentation | |||
| History of OI | 11 (16.7) | 14 (11.3) | 25 (13.2) |
| Prior OI on admission | 55 (83.3) | 110 (88.7) | 165 (86.8) |
| Toxoplasmosis | |||
| Not present | 46 (69.7) | 92 (74.2) | 138 (72.6) |
| Present | 20 (30.3) | 32 (25.8) | 52 (27.4) |
| Pneumocystosis | |||
| Not present | 49 (74.2) | 88 (71.0) | 137 (72.1) |
| Present | 17 (25.8) | 36 (29.0) | 53 (27.9) |
| Cryptococcosis | |||
| Not present | 59 (89.4) | 109 (87.9) | 168 (88.4) |
| Present | 7 (10.6) | 15 (12.1) | 22 (11.6) |
| Histoplasmosis | |||
| Not present | 57 (86.4) | 112 (90.3) | 169 (88.9) |
| Present | 9 (13.6) | 12 (9.7) | 21 (11.1) |
| Candidiasis | |||
| Not present | 63 (95.5) | 119 (96.0) | 179 (94.2) |
| Present | 3 (4.5) | 5(6.2) | 8 (4.2) |
| Tuberculosis | |||
| Not present | 48 (72.7) | 88 (71.0) | 136 (71.6) |
| Present | 18 (27.3) | 36 (29.0) | 54 (28.4) |
| CMV infection | |||
| Not present | 64 (97.0) | 119 (96.0) | 183 (96.3) |
| Present | 2 (3.0) | 5 (4.0) | 7 (3.7) |
| MAC infection | |||
| Not present | 66(100) | 123 (99.2) | 189 (99.5) |
| Present | 0 | 1 (0.8) | 1 (0.5) |
| Coccidia infections | |||
| Not present | 64 (97.0) | 121 (97.6) | 185 (97.4) |
| Present | 2 (3.0) | 3 (2.4) | 5 (2.6) |
| Defining neoplasm | |||
| Not present | 59 (89.4) | 106 (85.5) | 165 (86.8) |
| Present | 7 (10.6) | 18 (14.5) | 25 (13.2) |
| Non-defining neoplasm | |||
| Not presente | 65 (98.5) | 122 (98.4) | 187 (98.4) |
| Present | 1 (1.5) | 2 (1.6) | 3 (1.6) |
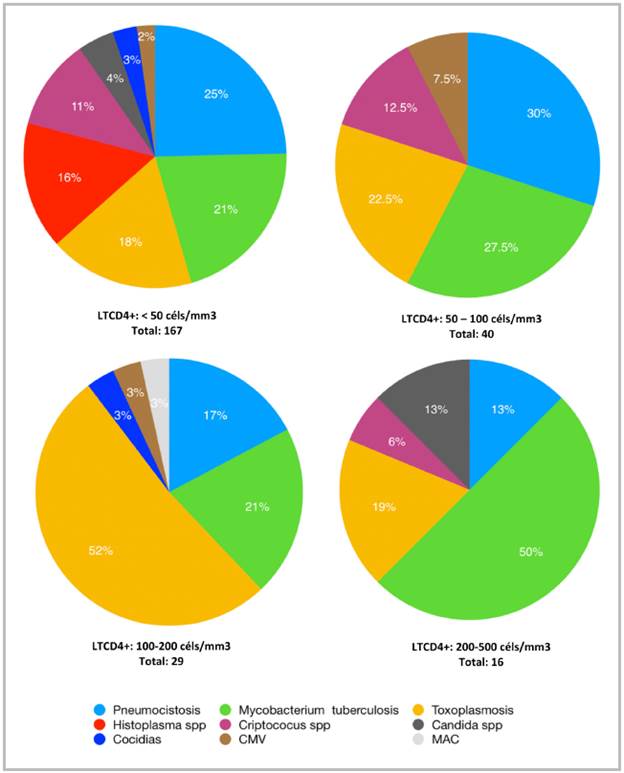
Regarding the association of OIs in relation to the CD4+ T cell count, 91% of the OIs occurred in patients with fewer than 200 cells/mm3 and only 1.8% of the OIs in those with lymphocyte counts greater than 500 cells/mm3.
Sixty-three percent of the cerebral toxoplasmosis cases were found in patients with CD4+ T cell counts less than 100 cells/mm3 and 62% of the pneumocystosis cases were found in patients with CD4+ T cell counts less than 50 cells/mm3, as were 100% of the Histoplasma infections (21). Tuberculosis was found in all ranges, with more patients in the CD4+ T cell range of less than 50 cells/mm3 (52%) (Table 4, Figure 2).
Discussion
Human immunodeficiency virus infection is a public health problem due to its high economic impact 14. In the described population, OIs were more frequent in men (65.3 vs. 34.7%) and at a general age ranging from 33 to 44 years, similar to populations described in other cities in our country and other countries in Latin America and Europe 4-16. The overall prevalence of undernutrition was high (37.9%), comparable to the undernutrition rate of patients hospitalized with AIDS in similar groups 18,19, probably due to most of the admitted patients being severely immunocompromised, with a CD4+ T cell count <200 cells/mm3, which is known to be related to undernutrition 20.
Most AIDS diagnoses and deaths are preventable, and one of the main predictors of HIV morbidity and mortality is late diagnosis of HIV infection. Altogether, 69.6% met the definition of LD, much higher than the 53% recorded in the European population, but similar to some African registers 10,21. A total of 86.8% of the patients with OIs had a CD4+ T cell count <200 cells/mm3; counts under 50 cells/ mm3 were found in 54.7% of the patients, and only 42.1% were on an ART scheme at the beginning of the study, very far from the 90-90-90 WHO 2020 objective and from the 81% reported in some cohorts in industrialized countries 22. For ART to be effective (reach undetectable plasma VLs), at least 95% of the daily doses must be taken; in our study, treatment adherence was measured with a patient survey which indicated that only 31% of the patients had adequate adherence, which could explain the very low percentage of undetectable VLs (8%).
Our study shows that the most common OIs were tuberculosis with 28.4%, followed by pneumocystosis with 27.9% and toxoplasmosis with 27.4%; oral candidiasis, histoplasmosis and cryptococcosis were reported in 4.2, 11.1 and 11.6%, respectively. This spectrum has varied widely from population to population and depends on some factors like access to ART or adequate affiliation to a social security system. Tuberculosis has already been described as the main OI in other data published in our country 23. Human immunodeficiency virus infection is known to have fostered a dramatic increase in the incidence of TB in many areas of the world, in some of which it is 10 times greater in people infected with HIV than in the general population 24.
In other countries, for example the United States, Djawe et al. describe pneumocystosis and Kaposi sarcoma as the most frequently reported OIs of all times (prior to and after the beginning of effective ART) 25. Among the systemic mycoses, cryptococcosis is most often found in patients with AIDS, especially in the form of meningoencephalitis. One of the most significant risk factors for opportunistic mycotic infections in patients with HIV infection is a CD4+ T cell count less than or equal to 200 cells/mm3 (26, which was corroborated in our study.
Table 4 Opportunistic infections according to CD4 T cell count.
| Opportunistic infections | CD4 T lymphocyte count | ||||
|---|---|---|---|---|---|
| Less than 50 | 50 - 100 | 100 - 200 | 200 - 500 | More than 500 | |
| Toxoplasmosis | 24 (17.9) | 9 (22.5) | 15 (51.7) | 3 (18.7) | 1 (25) |
| Pneumocystosis | 33 (24.6) | 12 (30) | 5 (17.2) | 2 (12.5) | 1 (25) |
| Cryptococcus | 15 (11.1) | 5 (12.5) | 0 | 1 (6.25) | 1 (25) |
| Histoplasma | 21 (15.7) | 0 | 0 | 0 | 0 |
| Candida | 6 (4.5) | 0 | 0 | 2 (12.5) | 0 |
| Tuberculosis | 28 (20.9) | 11 (27.5) | 6 (20.7) | 8 (50) | 1 (25) |
| CMV | 3 (2.2) | 3 (7.5) | 1 (3.4) | 0 | 0 |
| MAC | 0 | 0 | 1 (3.4) | 0 | 0 |
| Coccidia | 4 (2.9) | 0 | 1 (3.4) | 0 | 0 |
| Total | 134 | 29 | 4 | ||
| A total of 223 OIs were recorded; 48 patients had more than one OI and the three most common associations were histoplasmosis associated with pneumocystosis, tuberculosis associated with pneumocystosis and tuberculosis associated with toxoplasmosis. | |||||
In our study, 22 cases of Cryptococcus infection were documented, 20 of which were in patients with CD4+ T cell counts under 200 cells/mm3, which corresponds to 12.1% of all patients in this CD4+ T cell range; only two cases were documented in patients with CD4+ T cell counts greater than 200 cells/mm3. We underscore a low percentage of OIs due to Candida, which suggests a low rate of diagnosis at our center. These data are similar to local studies in which a prevalence of Candida infection of up to 5.5% has been estimated in patients with HIV 27.
We highlight the fact that patients with CD4 counts <50 cells/mm3 were more prone to having more than one OI (often three), compared with all the patients studied, which concurs with other reviews 28-29.
Conclusions
Despite the availability of highly-effective ART, OIs continue to cause considerable morbidity and mortality in patients infected with HIV. Accessibility to ART should be improved, delayed diagnosis reduced, and above all, lack of adherence to treatment should be impacted (the latter derived from psychosocial and economic factors, including low educational level, poverty and unemployment) 30. Instating certain measures like regular medical visits, evaluating barriers prior to beginning ART, using ART with a high genetic resistance barrier, simplified dosing schemes (including the single-pill regimen), and multidisciplinary approaches including social work, are important strategies which need to be disseminated more 31,32.
In our population, most patients are hospitalized in advanced stages with OIs and with evidence of severe viral and immunological compromise. Our study contributes valid information regarding the main OIs affecting this population, which should therefore be thoroughly checked for, along with cancers, when evaluating patients with HIV infection.











 texto em
texto em