Introduction
Auto-brewery syndrome, also known as gut fermentation syndrome, is defined as a clinical condition in which the carbohydrates ingested are changed into alcohol by microorganisms in the gastrointestinal tract 1. This syndrome has been found to be more prevalent in patients with comorbidities like diabetes, obesity and Crohn's disease 2,3; however, it has also been described in healthy people 2. Although the syndrome is rarely diagnosed, this is probably due to an underreporting of notifications in the literature 4.
This report describes the case of a patient with classical symptoms of auto-brewery syndrome, with no prior alcohol ingestion and with clinical improvement after medical treatment. It is a very rare case, and, since it is poorly described in the medical literature, we attempt to explain the basic concepts of the disease.
Case description
This was a 55-year-old male patient who was previously active and healthy (height 170 cm, weight 80 kg, BMI 27.6 kg/m2). He was from an urban area, worked as a teacher, had no significant medical or psychiatric history, and was taking no medications at the time of the visit. He was seen for the first time by internal medicine due to a 10-12-year history of general malaise along with symptoms of inebriation after eating certain carbohydrates. These episodes occurred approximately once a week and were triggered or aggravated by emotional stress. He reported a need to eat salty foods after these events, which improved the symptoms somewhat. He denied weight loss or drinking alcohol. A relative (sister) was interviewed and confirmed these events.
Studies and laboratory tests were performed including: normal glucose at 91 mg/dL; negative hepatitis B and C; negative antinuclear, anti-smooth muscle and antimitochondrial antibodies; negative ceruloplasmin; SGPT transaminase at 62 mg/dL and SGPT transaminase at 119 mg/dL (slightly elevated); total bilirubin 1.07 mg/dL, direct 0.27 mg/dL and indirect 0.8 mg/dL (normal); amylase 80 mg/dL (normal); thyroid function with TSH 0.70 mg/dL (normal); and negative IgG and IgM transglutaminases. An abdominal ultrasound reported gallbladder polyps, and a liver within normal limits.
Auto-brewery syndrome was suspected due to the clinical signs and symptoms and their correlation with the diagnostic tests. Management was begun with various treatments including a gluten, starch and carbohydrate-free diet; methadone 500 mg three tablets/day for three months; fluconazole 200 mg/one tablet/day for two months; ampicillin 500 mg/one tablet every six hours for 10 days; prebiotics; and pancreatin plus simethicone, one tablet with each meal.
After three months, the patient reported clear clinical improvement, specifically mentioning that the clinical condition improved mainly with the removal of carbohydrates from the diet. However, episodes persist associated with high work stress (as a teacher) and family stress due to an intolerant spouse and the medical problems of a child with Down syndrome.
He was seen again in August 2018, reporting a new crisis lasting four days which was directly related to a family stress situation. He attended the appointment with his sister who he stated was with him during the episode and who reported that the patient was in good condition and suddenly noticed signs of inebriation with facial reddening and slurred speech. A blood glucose measurement was therefore taken in the office, with a result of 95 mg/dL (normal), and treatment with 1,000 cc per day of dextrose in normal saline solution was ordered for three days, with 3 cc of vitamin B complex in each bag. Treatment was also continued with one tablet of pancreatin before each meal.
The patient went to a follow up appointment in October 2021, reporting that the episode receded quickly with intravenous fluids. He brought complementary studies along: a gastroscopy with a pathology report of Helicobacter pylori positive non-atrophic chronic gastritis (Figure 1); and a colonoscopy showing internal hemorrhoids, two sigmoid polyps 45 cm from the anal border (resected through loop polypectomy), and otherwise normal with a tubular adenoma with low-grade dysplasia reported on pathology (Figure 2). Laboratory tests showed: left and transverse colon KOH with no sign of mycotic structures; negative germ culture at 72 hours; uric acid at 10.95 mg/dL (slightly elevated); pyruvate transaminase 44.45 u/L (normal); total bilirubin 1.06 mg/dL, direct bilirubin 0.3 mg/dL and indirect bilirubin 0.76 mg/dL (normal); oxaloacetic transaminase 27.4 u/L (normal); and quantitative ethyl alcohol in the blood >10 mg (+).
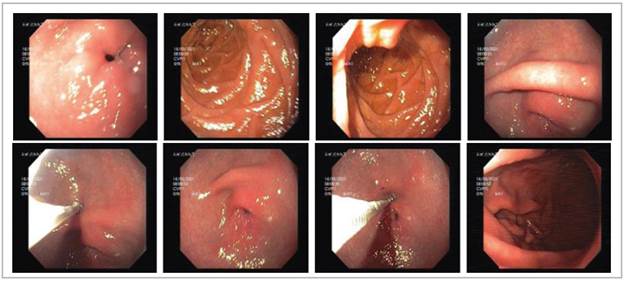
(Source: Authors).
Figure 1 The upper gastrointestinal endoscopy shows a normal mucosa, lumen and caliber in the esophagus and gastroesophagealjunction. The stomach has a scant gastric lake, with no fundus abnormalities. The body has preserved rugae and distensibility and a healthy mucosa. The anthrum shows alternating erythema, and therefore a biopsy was taken. The pylorus and duodenum have a normal mucosa, lumen and caliber.
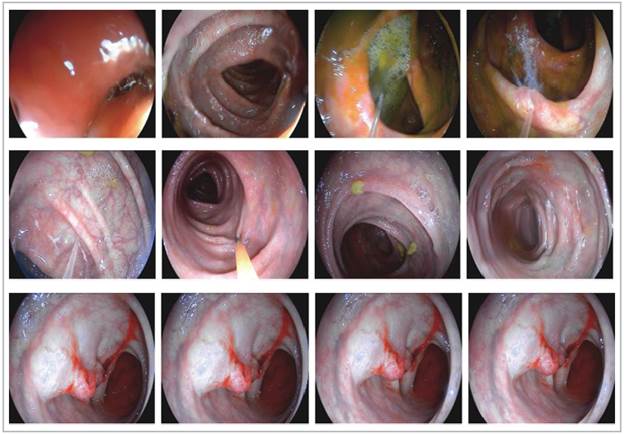
(Source: Authors).
Figure 2 The colonoscopy shows the sigmoid, left, transverse and right colon up to the cecum, with two polyps in the sigmoid colon 45 cm from the border of the anus. A polypectomy was performed using a hot loop prior after infiltrating with adrenaline. The rest of the mucosa, lumen and caliber are normal.
It was determined that the patient should continue with the instated treatment, and a psychology consult was requested given his high degree of emotional stress and its direct relationship with his disease. He continues to be followed by internal medicine and gastroenterology.
Discussion
Auto-brewery syndrome, also known as gut fermentation syndrome and endogenous ethanol fermentation syndrome, is due to ethanol being produced through endogenous fermentation by fungi or bacteria in the gastrointestinal system 5. The body changes sugars and carbohydrates into alcohol. The first cases were reported in Japan in the 1950s-1970s 4,6. A possible relationship is suspected with yeasts (Saccharomyces cerevisiae, Candida albicans, Candida tropicalis and Toluropsis glabrata) and bacteria (Klebsiellapneumonia) identified as pathogens, as they can dissolve carbohydrates in alcohol 6,7. Likewise, patients with type 2 diabetes mellitus or liver cirrhosis have also been noted to have elevated endogenous ethanol levels 1.
The pathophysiology of the disease includes altered intestinal microbiota which allows overcolonization of the previously described microorganisms, and the main associated cause is a diet rich in carbohydrates and refined foods and excessive antibiotic use 6,8.
This syndrome has significant effects on the person's life, given the patient's signs and symptoms which may include vomiting, dizziness, loss of coordination, disorientation, irritable bowel symptoms, mental confusion, fatigue, slurred speech, mood changes, abdominal pain, and dry mouth, as well as other symptoms which are highly significant because of their effect on the patient's quality of life like depression, anxiety, restlessness, and loss of memory and concentration 6,9.
A complete history and physical is needed for diagnosis, including family history and eating habits. Complementary tests are also used, including a complete blood count, metabolic panel, drug screen, stool culture, endoscopy and colonoscopy, collecting gastrointestinal secretions for bacterial and fungal tests. The glucose test, which detects elevated ethanol levels at any stage in the test, can confirm the syndrome and, finally, blood and urine alcohol levels 4,10.
Treatment for the disease is based mainly on general measures and diet modifications, which should be high in proteins and low in carbohydrates, refined sugars and processed foods, as this helps balance the intestinal fungi 10,11. Within pharmacological treatment, most patients need one or more cycles of azoles or polyenes. Antifungals (fluconazole, itraconazole, nystatin, caspofungin) may be used 5,6,11. In this case study, diet restriction and medications like fluconazole, prebiotics, pancreatin plus simethicone and ampicillin were used.











 texto em
texto em 


