Introduction
Acquired or congenital valvular heart disease complicates approximately 1-3% of all pregnancies and is one of the main causes of maternal deaths 1. Over the last few decades, more women with valve disease have achieved pregnancy 2. Although valve disease due to rheumatic heart disease has decreased in industrialized countries, it continues to be one of the main causes of cardiovascular maternal morbidity and mortality in middle and low-income countries 3. Despite improvements in diagnosis and treatment, valve disease continues to be associated with adverse maternal and fetal events. Pregnant women with mechanical prosthetic valves (MPVs) have a higher risk of complications 4. The use of anticoagulants and a prothrombotic state associated with pregnancy cause more maternal and fetal outcomes 5,6. In the ROPAC registry, only 58% of women with mechanical valves had an event-free pregnancy 7. While it is possible for women with MPVs to have successful pregnancies, there are potential complications, some of which can be fatal. Our goal was to identify and describe the main complications in pregnant women with MPVs, whether these outcomes are preventable, and their impact on cardiovascular, obstetric and fetal outcomes.
Materials and methods
This was an analytical study of a prospective cohort at the cardio-obstetric clinic of a referral institution for heart disease in pregnancy. Data were taken from the Registro de Embarazo y Enfermedad Cardiaca (REMEC) [Pregnancy and Heart Disease Registry], in which pregnant women with heart disease were prospectively enrolled. From January 2016 to November 1, 2021, 540 pregnant women with heart disease were registered. This study reports the main cardiovascular, fetal and obstetric outcomes in pregnant women with MPVs included in the registry during this time. The initial characteristics included maternal age, general cardiovascular risk factors, main non-cardiac diseases, the cardiac diagnosis, prior interventions, cardiac symptoms, valve replacement procedure, anticoagulation regimen and obstetric history.
Primary cardiac events were defined as heart failure, sustained symptomatic arrhythmias requiring treatment (tachyarrhythmias or bradyarrhythmias), cerebrovascular accidents, and cardiac arrest or death. Secondary cardiac events were defined as a deterioration of two or more NYHA classes compared with the baseline, and the need for an urgent invasive cardiac procedure during pregnancy or while in the hospital post-partum. Obstetric outcomes were non-cardiac maternal death, hypertensive disorders of pregnancy and postpartum hemorrhage.
Maternal death was defined as death during pregnancy and up to six months after delivery. Spontaneous abortion was defined as a pregnancy loss up to 20 weeks; fetal death as a fetal loss after 20 weeks. Postpartum hemorrhage was defined as a major loss of blood (>500 mL after a vaginal delivery or >1,000 mL after a Cesarean delivery) immediately after delivery and up to 24 hours after delivery.
Neonatal outcomes were considered to be premature birth, low weight for gestational age, respiratory distress syndrome, intraventricular hemorrhage, fetal death, and neonatal death (up to 28 days after birth) 3. Premature birth was defined as delivery before 37 weeks gestation. Low birth weight was defined as birth weight under the 10th percentile for gestational age. We defined late care as the first visit after week 20 8.
Thromboembolic complications were defined as peripheral arterial embolism or mechanical valve thrombosis (MVT), or an embolism manifested by a new transient or permanent neurological deficit. They also include pulmonary emboli, deep vein thrombosis or any ischemic cardiovascular or cerebrovascular event.
For the purposes of this article, inadequate anticoagulation was defined as the lack of anticoagulants in the treatment plan, or two INR test results outside of the desired range from the beginning of pregnancy, or the use of low-molecular-weight heparin (LMWH) without measuring anti-factor Xa levels. Major bleeding was defined as a hemorrhage leading to at least a 1 g/dL reduction in hemoglobin, the need for blood product transfusions or target organ damage, like a hemorrhagic cerebrovascular accident or retinal injury.
Major adverse cardiac events (MACEs) were defined as cardiac death or cardiac arrest, serious arrhythmias, including sustained ventricular arrhythmias or other sustained arrhythmias which require admission to intensive care, congestive heart failure (CHF) requiring admission to intensive care, aortic dissection, myocardial infarction, cerebrovascular events, MVT, pulmonary embolism, endocarditis or the need for an urgent cardiac procedure (during pregnancy and up to four weeks after delivery) 9.
To define preventable events, when a MACE occurs, an assessment is made of whether there were deviations from the standard care that could have led to the outcome.
To determine if primary events were preventable, we used a previously established tool which was first used in the Harvard Medical Practice Study10,11. Finally, for the descriptive analysis, the data were expressed as means with standard deviation for continuous variables and percentages for categorical variables. The analysis was done using SPSS (version 22) software to analyze the data obtained.
Results
Study population
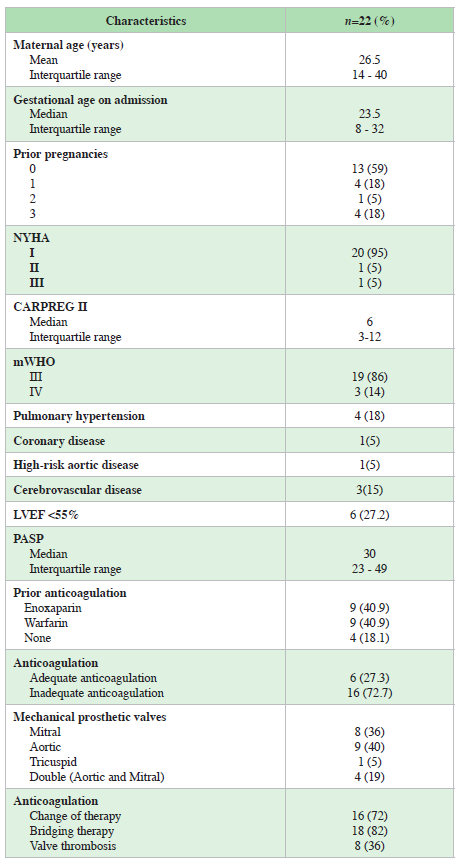
Between January 1, 2016, and November 1, 2021, 22 patients with MPVs were included in REMEC; 4% of the total registry underwent 22 pregnancies. The mean age was 26.5 years (minimum 14 - maximum 40 years). The median number of hospitalizations throughout pregnancy was two (IQR 1-2). The population recorded a median CARPREG II of 6 points (minimum 3 - maximum 12); 86% were classified as mWHO class III and 14% as class IV; 27.2% had left ventricular dysfunction, 18.8% had pulmonary hypertension, and 4.5% had coronary disease. Nine (40.9%) of the pregnancies occurred in women with mitral MPVs, 8 (36.3%) of the pregnancies occurred in patients with aortic MPVs, four (18%) occurred in patients with a double lesion and valve change (aortic and mitral) and one (4.5%) had a tricuspid prosthesis in a systemic ventricle due to congenitally corrected transposition of the great vessels. There were 17 live births from 22 pregnancies (77.3%), with a median of 35.5 gestational weeks at delivery (IQR 24-37); most of the deliveries were by Cesarean (88%); of these, 33% for cardiac reasons and the rest for obstetric reasons; there were only two vaginal deliveries. The demographic and clinical data are presented in Table 1.
Anticoagulation regimen
Sixteen patients (72.7%) had inadequate anticoagulation on admission. Four (18.1%) were not on any anticoagulant treatment on admission. Nine women (40.9%) used VKAs and nine (40.9%) were on a low-molecular-weight heparin scheme. Only one patient had anti-factor Xa levels in her assessment. Most of the women (n = 16) were changed to bridging therapy with UFH (Table 1).
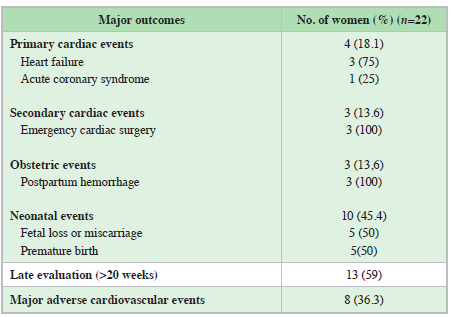
Maternal outcomes
There was 100% maternal survival during follow up. However, the rate of complications was high. We found only four women (18%) with no primary or secondary cardiac, obstetric or neonatal outcomes. Primary cardiac events occurred in 18.1% of the patients, secondary cardiac events in 13% of all cases, and obstetric outcomes in three of the patients (13.6%). Fifty-nine percent of the patients had late assessments (>20 weeks), with a median of 23.5 weeks (IQR 8-32) at the initial visit. None of the patients had a preconception assessment (Table 2).
Neonatal outcomes
Ten (45.4%) had neonatal events. Fetal loss or miscarriage occurred in five of 22 pregnancies (22.7%). On admission, two were anticoagulated with warfarin, two with LMWH and one had no anticoagulation. We found no significant differences in fetal loss between the groups treated with LMWH and those treated with warfarin. There were three spontaneous abortions in the first trimester, and two fetal deaths after week 20. There were five cases of premature birth, one newborn had neonatal depression as a complication of anesthesia from the Cesarean, and there was one case of warfarin syndrome associated with chronic use, despite low doses (<5 mg) (Table 2).
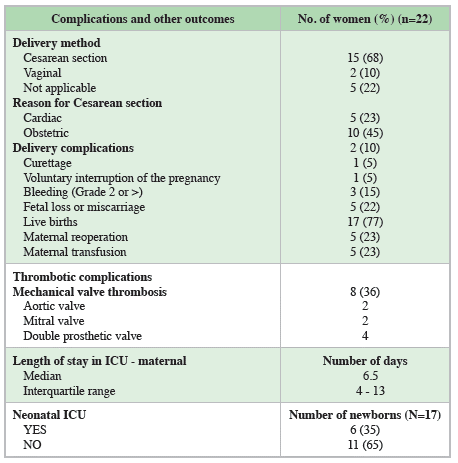
Thrombotic complications
We found MVT in eight cases (36.3%). Of these, four (50%) were in women using LMWH without measuring anti-Xa levels, three (37.5%) in women on warfarin but with inadequate anticoagulation and one patient with no anticoagulation on admission. Three of the women had valvular obstruction requiring acute cardiac surgery during pregnancy (13.6% of all the cases); the rest of the thromboses were treated conservatively. The four women with a double valve lesion (mitral and aortic) developed valve thrombosis. Two of the MVTs occurred in women with mitral valves and two with aortic valves (Table 3).
Hemorrhagic complications
Major gynecological bleeding occurred in three (13.6%) of the cases, and two had minor hemorrhaging. These five patients required reoperation and blood transfusions. Three of these patients were on LMWH at admission, and two were using warfarin, with all of them using UFH prior to the procedure. There was no significant difference in the type of anticoagulant and the need for reintervention or transfusion (Table 3).
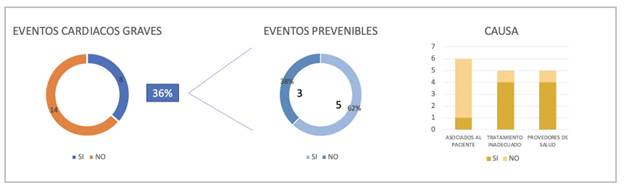
Major adverse cardiac events
No maternal deaths were reported among the MACEs. All MACEs were due to valve thrombosis (eight cases). There were three urgent procedures during pregnancy, two for thrombosis and prosthetic malfunction and one for related heart failure. One case had thrombosis-related ACS which had the same surgical outcome. No cases of infective endocarditis, aortic dissection or ventricular arrhythmias requiring intervention were reported. Of all the MACEs, 62% (5 out of 8) were considered to be preventable according to the definitions used in this study. The preventable events occurred due to patient-related factors (one case), inadequate treatment (four cases) and, in most, a lack of management by healthcare providers (Figure 1).
Other outcomes
The length of ICU stay for the new mothers was 6.5 days (IQR 4-13), and six (35%) of the live births required neonatal ICU. The length of stay after delivery was 12.5 days (IQR 9-26) (Table 3). For postpartum family planning, 11 patients had a defined plan prior to discharge, nine with definitive contraception by tubal ligation, one with pills and one with an implanted device. For the other 11 patients, postpartum planning was left to their healthcare providers.
Discussion
This study evaluated pregnant women with mechanical prosthetic valves in the REMEC, a prospective registry at a tertiary care hospital with a cardio-obstetric clinic. No maternal deaths occurred, although there were very high rates of maternal and fetal events. Of 22 patients with mechanical prostheses, 82% of the patients had some type of adverse event, with 18.1% being primary cardiac events, 9% secondary cardiac events, and 13.6% obstetric outcomes. In addition, there were 45.4% neonatal events, with a 22.7% rate of miscarriages or fetal losses. This elevated rate of adverse events is even more concerning when the rate of MVTs in these patients was found to be 36.3%, in all cases due to inadequate anticoagulation regimens that were not implemented according to the clinical practice guidelines 12. These cases also led to the need for emergency surgery in 13.6% of the patients. The anticoagulation regimens were variable and, unfortunately, inadequate.
Patients with MPVs are at high risk according to the modified WHO classification (Class III) 12; in addition, we had 14% of the patients in modified WHO Class IV, due to the presence of other more serious diseases. The frequency of adverse maternal events was higher than that reported in other studies 13-16 and higher than what is reported in the European Registry of Pregnancy and Cardiac disease (ROPAC), which is the largest study on this topic. In the ROPAC, only 58% of the pregnant women with MPVs had complication-free pregnancies with live births 7. In this study, only 18% of the patients had no complications of any type. Likewise, the MVT rate was high (36.3%) compared with what was reported by Ashour et al. (13.4%) 15, Nassar et al. (9%) 16, Sadler et al. (8%) 13, Maziboku et al. (6.5%) 14, and ROPAC (4.7%) 7. This could be explained by the healthcare access barriers which are common in middle and low-income countries like ours, in which patients have limited opportunities for prompt referrals to centers of excellence due to cultural, geographical or administrative barriers. This can be seen in the fact that 59% of the patients had a late referral to a reference center (>20 weeks' gestational age), and none of the patients had a preconception evaluation, despite having a clearly high-risk cardiovascular history and, consequently, a greater proportion of adverse outcomes.
In the CARPREG-II study, an initial evaluation later than 20 weeks was an independent risk factor for adverse events 17. The difficulties in chronic anticoagulation use are explained in the same way, with inadequate regimens in 72% of the patients at their first visit to the cardio-obstetric clinic, and four patients (18.1%) not even on anticoagulation, despite this treatment being clearly recommended by the different clinical practice guidelines 18,19.
Patients' fear of the treatment side effects and healthcare providers' lack of knowledge of the anticoagulation regimens during pregnancy explain these treatment errors. Likewise, the unavailability of anti-Xa measurements leads providers to begin LMWH due to concerns regarding warfarin's effects on the fetus, but not follow the recommendation to monitor anticoagulation in pregnant women with this test, given the unpredictability of LMWH in pregnant women 12,20. This shows the need for more education on the use of different anticoagulation regimens in pregnancy, including warfarin; for, as stated by Nishimura, "vitamin K antagonists are an accepted and necessary treatment for all patients with mechanical prosthetic valves to prevent valve thrombosis and systemic embolism." 21. We also highlight the fact that LMWH is not recommended when the anti-Xa levels cannot be monitored for weekly dose adjustments (Recommendation III-C) 12,20.
All of the MVT cases occurred in patients who had an inadequate anticoagulation regimen: four cases (50%) in patients who had been changed from warfarin to LMWH, but without anti-Xa level measurements; three cases (37.5%) in patients on warfarin, but with subtherapeutic INR levels; and one case (12.5%) in a patient with no anticoagulation. It is interesting that, although there were four patients with no anticoagulation, the other three did not have MVT on admission and, subsequently, with an adequate anticoagulation regimen and close monitoring, they did not develop this complication. On the other hand, these thrombotic events were classified as major adverse cardiovascular events, finding that 62% of the cases were preventable.
It is important that the events were preventable due to patient-related factors in only one case, while the remaining cases occurred especially due to inadequate treatment and administrative difficulties with the insurer. These findings are similar to those reported by Pfaller et al. in an evaluation of complications of pregnant women with heart disease, in which the main cause of preventable adverse cardiovascular events was attributed to factors related to the healthcare provider 9. These findings indicate the need to look for strategies for educating healthcare providers in the care of pregnant women with heart disease, and especially to seek to facilitate access to referral centers for this vulnerable population.
Despite the high number of cardiac events and, specifically, valve thrombosis events, it is remarkable that there were no maternal deaths in this group of patients, while in the ROPAC they made up 1.4% 7 and in the study by Ashour et al. they accounted for 4% 15. However, three patients (13.6%) required emergency surgery for serious obstructive thrombosis, while the other five cases of valve thrombosis responded to conservative treatment with anticoagulation.
On this point, we believe that the availability of a reference cardio-obstetric team with well-defined functions and treatment plans at the institution may have played a role, with assessment of critically ill patients activated within minutes, resulting in a prompt multidisciplinary evaluation by a team established seven years ago. In addition, the team includes the different medical-surgical specialties needed to care for the complications that may occur in these patients, in line with the recommendations 12,22. However, we insist on the need to prioritize the prevention of complications by adequately explaining the types of valves to women of reproductive age who require valve change, with a detailed description of their advantages and disadvantages, to best determine the type of valve to be implanted, remembering that the guidelines recommend a bioprosthesis in women who wish to conceive (Recommendation IIa-C) 19.
In any case, it should be kept in mind that while the rate of complications is lower with biological valves than with mechanical valves, they will both require close monitoring due to a higher rate of adverse events than in other non-valvular heart diseases, as was shown in ROPAC 7. Furthermore, strategies should be facilitated to increase the number of planned pregnancies and appropriate preconception assessments with experienced groups to implement anticoagulation therapy following the current recommendations in a center with trained staff and the different logistical and laboratory resources needed to guide these therapies 20,22. We reported a very high rate of Cesarean sections in these patients (68%), although most were for obstetric reasons; this rate was higher than previous reports from ROPAC 23 and other REMEC publications 24,25 and possibly related to the fact that the Cesarean sections reported in those studies were in pregnant women with general heart disease and not those with PMVs.
The rate of Cesarean sections for cardiac reasons was also higher (33%) than in previous studies 24,25. This was related to beginning labor without at least a two-week anticoagulation-free period and the risk of fetal brain hemorrhage from passing through the birth canal 12.
Long-term birth control is essential in these patients; thus, part of the multidisciplinary evaluation is to determine a birth control plan 12,22. Half of the patients evaluated had their birth control plan defined prior to discharge, but the rest of the patients, by their own choice, decided on an outpatient birth control plan.
Study limitations
This is the experience of a single tertiary-care referral center for pregnant women with heart disease. The small number of patients prevented a broader statistical analysis and the ability to investigate confounding factors like the underlying cardiac diagnosis or functional status. Another limitation lies in the different anticoagulation regimens used prior to admission, although this is precisely the reality these patients experience in their everyday life. However, these data show points for improvement, like the need to provide education for physicians who are not familiar with these patients, and to seek strategies to eliminate the access barriers in order to improve maternal-fetal outcomes.
Conclusions
This prospective study has shown that pregnant women with mechanical prosthetic valves have a high proportion of cardiovascular, maternal and fetal events. There is a wide variety in anticoagulation regimens and follow up, and the preconception evaluations to reduce risk appear to be insufficient. The information from this study may lead women and physicians to reevaluate the choice of prosthetics for women who wish to conceive. Women with MPVs and their physicians should understand the significant risks of pregnancy and the need for specialized care to concentrate the centers' experience and decrease preventable events in this setting.











 text in
text in