Introduction
At the end of 2019, some cases of a new rapidly contagious infection were reported in Wuhan, China 1, which resulted in the World Health Organization announcing a pandemic on March 11, 2020 2, presenting great challenges for governments and healthcare systems 3 and primarily affecting first line and critical care 4.
Coronavirus disease is characterized by a series of symptoms such as fever, fatigue, headache, muscle aches and diarrhea 5,6. One week after the onset of symptoms, some patients develop dyspnea 7, thus leading to a severe stage of the infection, with the onset of acute respiratory distress syndrome (ARDS) being the main reason for needing ICU care 8.
Acute respiratory distress syndrome is an inflammatory process in the lungs which causes protein-rich non-hydrostatic pulmonary edema whose immediate consequences are severe hypoxemia, decreased pulmonary distensibility and increased pulmonary dead space 9.
In 1967, Ashbaugh et al. 10 described a case series of 12 patients with respiratory diseases who had an unusual clinical course and response to respiratory support, depicting a disease similar to pediatric respiratory distress syndrome or hyaline membrane disease. These patients had severe dyspnea, tachypnea and oxygen-refractory cyanosis with loss of pulmonary distensibility and a better response to PEEP.
After several years of case reports of this new entity, the first American-European Consensus Conference (AECC) was published in 1994 11 recognizing ARDS as a clinical spectrum with an insidious onset which encompassed blood gas and radiological severity parameters such as bilateral opacities on the AP x-rays of patients with a pulmonary wedge pressure < 18 mmHg or without clinical evidence of left ventricular hypertension, thus ruling out patients with cardiogenic pulmonary edema, and who had a PaO2/FiO2 < 200 mmHg. Ventilatory parameters were not taken into account at that time because this practice varied widely, depending on the physician who performed it.
In 2011, a panel of experts gathered at the initiative of the European Society of Intensive Care Medicine, supported by the American Thoracic Society and the Society of Critical Care Medicine 8, and developed the Berlin definition, covering a series of limitations of the AECC definition. They proposed three mutually exclusive categories of ARDS, based on the degree of hypoxemia: mild (PaO2/FiO2 from 200-300 mmHg), moderate (PaO2/FiO2 from 100-200 mmHg) and severe (PaO2/FiO2 less than 100 mmHg), quantifying the time of onset of the symptoms, with the "insidious" stage ending one week after the onset of symptoms or when new respiratory symptoms are exacerbated. The radiological criterion of bilateral opacities was maintained, and, given the lack of use of catheters for measuring pulmonary artery wedge pressure and the potential for concomitant ARDS and congestive heart failure, this criterion was removed, including instead in the definition of ARDS, patients with signs and symptoms of ventilatory failure not totally explained by uncompensated heart failure. A criterion of a minimum PEEP of 5 cm H2O was added, which gained a space in the definition due to the advances of the last few years in protective mechanical ventilation.
In 2019, the Asociación Colombiana de Medicina Crítica y Cuidado Intensivo [Colombian Association of Critical Care Medicine and Intensive Care] 12 published a consensus in which they reviewed the Berlin criteria, proposing that a good number of patients are diagnosed within the first 72 hours, with almost all being diagnosed within the first week. They also recommended performing a chest CT to improve objectivity regarding the criterion of multilobar opacities not due to cardiogenic edema, keeping in mind that a chest x-ray may be observer-dependent, or the image may be confused with masses or nodules. In addition, they recommended using ultrasound as an adjuvant tool.
Considering the ARDS definition, it is interesting how most of our population had COVID-19 cases that could be classified as severe. Thus the need to describe these cases and evaluate the factors that may have contributed to the outcome in this population.
Knowledge of patient characteristics and risk factors associated with mortality in patients with severe COVID-19 ARDS in the ICU is widely discussed in first world countries (13, 14). The risk factors most often found are male sex, arterial hypertension and diabetes mellitus 15.
Data from Wuhan 16 estimate a 41.67% mortality in patients who require hospital care, with greater mortality in older patients, reporting arterial hypertension as a risk factor associated with mortality, with a 52.3% prevalence in non-surviving patients and 44% in survivors. Patients who died had higher levels of IL-2 and the study reported high mortality among patients who required invasive mechanical ventilation.
In Italy 17, they found a 26% mortality in the ICU, with greater lethality in older and male patients. Arterial hypertension was the most frequent comorbidity in patients with severe disease; a high proportion of the patients required invasive mechanical ventilation and higher PEEP levels.
In New York, the mortality of ICU patients was 53.5% 18. The risk factors most associated with mortality were dementia, patients over the age of 65 and male sex.
In Colombia, according to the Ministry of Health and Social Protection figures, 2.73% of the cases were severe infections 19,20, requiring ICU care. COVID-19 was the cause of death in 21.7% of men and 17% of women between January and October 2020 13,21, mainly affecting older adults 22,23.
A study by Universidad de los Andes 24 showed that, as of March 3, 2021, 53% of Bogotá's population had been infected with COVID-19, highlighting a significant public health problem for the country, with the rate of contagion being higher in the lower socioeconomic strata, explained by psychosocial situations such as the inability to maintain a strict quarantine in this type of population.
According to a study by Universidad Nacional 9, the probability of dying and of needing ICU management is strongly correlated with older age and the male sex.
A study performed in four Colombian clinics 25 located in Bogotá, Cali, Pereira and Popayán, found that comorbidities like ischemic heart disease or COPD are more associated with the risk of needing ICU treatment, and advanced age, especially over 65, is associated more with mortality. The study found no variables associated with reducing the risk of death.
Cínica Belén, where the current study was carried out, is located in the town of Fusagasugá, which is part of the department of Cundinamarca, 59 km away from Bogotá. It is the fourth largest municipality in the department after Bogotá, Soacha and Facatativá 26. It is a municipal capital, with a population of 138,498 people according to figures from 2019; 68% of the population is between 15 and 64 years old, and 9% are over the age of 65 19, with a high concentration of vulnerable population compared with other communities in the country. This town has two hospitals with intensive care units, one of which is in Clínica Belén de Fusagasugá.
The population admitted to the ICU at Clínica Belén is characterized by being elderly and having multiple comorbidities, elevated poor prognostic markers and a high percentage classified as severe ARDS. Despite the extensive description globally, in Latin America and in the Colombian capital, there is local underreporting, and therefore there is a need to describe the mortality and lethality and evaluate which factors may have contributed to a fatal outcome, to thus increase the quality of care and vigilance for this type of patients in the future.
The first recommendations for managing our patients were based on prior experiences that considered MERS, SARS and H1N1 infections, which showed that corticoste-roids significantly reduced mortality 27, and which countries like Italy and the United States subsequently adopted, reporting positive impacts of corticosteroids on treatment.
We adopted a management plan based on the available evidence which consisted of the use of corticosteroids, beginning dexamethasone at 6 mg/day for 10 days, according to the RECOVERY study 28 in which thromboprophylaxis, adjusted according to the Padua and Caprini scales, was ordered. Next, antibiotic treatment was given, with ampicillin sulbactam as the first line, if needed by the patient (signs of systemic inflammatory response); if there was a risk of pseudomonas, piperacillin tazobactam 29 was begun. On the third day, if the patient had negative cultures, procalcitonin was taken; if it was negative, piperacillin was withdrawn. Colchicine was used as an anti-inflammatory in patients with multilobar pneumonia who required oxygen, in line with the Grecco 19 study 30, in which the patients who received colchicine as an anti-inflammatory had significantly less clinical deterioration (1/55 1.8% vs. 7/50 14%; OR=0.11, 95% CI 0.1-0.96), with a longer event-free survival in the group treated with colchicine, compared with the control group (97 versus 83%, p=0.03); therefore, colchicine was begun at 0.5 mg every 12 hours.
Materials and methods
Patient description
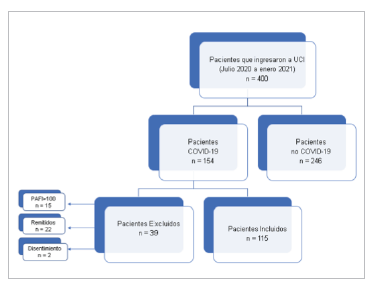
Data were taken from patients in the intensive care unit of Clínca Belén de Fusagasugá between July 2020 and January 2021. Most of the patients were from Fusagasugá and other patients came from neighboring communities or from Bogotá, due to its proximity. A total of 400 patients were admitted to the ICU during this time, 154 of whom met the criterion of SARS-CoV-2 infection confirmed by nasal swab using real-time polymerase chain reaction (RT-PCR), following the national guidelines.
Keeping the Berlin criteria in mind 8, all the patients had one week of respiratory symptoms or their exacerbation, and opacities in all four quadrants on the chest x-ray, verified by chest imaging and not explained by decompensated heart failure, lung collapse or nodules.
Data collection
This was a descriptive observational study in which 15 out of 154 patients were excluded for not meeting the criteria for severe ARDS, due to having a PaO2/FiO2 > 100 mmHg or requiring a PEEP < 5 cm H2O, thus resulting in 139 patients, 22 of whom were excluded because they required referral to more complex care, which made it difficult to follow them. Finally, two patients were excluded because they refused consent for invasive maneuvers, if needed. Altogether, 115 patients met the inclusion criteria for this study (Figure 1).
The analyzed variables included age, sex and comor-bidities; poor prognostic clinical laboratory parameters like LDH, ferritin, troponin, D-dimer and C-reactive protein; mortality and severity risk scales like APACHE II, SOFA, News2, MuLBSTA, and COVID GRAM; as well as the type of ventilatory support required (nonrebreather masks, noninvasive and invasive mechanical ventilation) and the timing of invasive mechanical ventilation after intensive care unit admission (taking < 48 hours and > 48 hours after admission to the ICU as cut off points). The FIO2 requirement on ICU admission and when invasive mechanical ventilation was begun was analyzed, as well as the required PEEP. The need for vasopressor support and patients who underwent prone positioning were also considered. Furthermore, patients with failed extubation, or the need for ECMO and renal replacement therapy (continuous veno-venous hemodiafiltration available in the intensive care unit) were taken into account. Survival data were taken at hospital discharge. Comorbidities and complications were analyzed according to age and survival status. The data used in this study were taken from the medical charts, analyzing the care received on admission to the ICU.
Statistical analysis
Qualitative variables were reported as absolute and relative frequencies, and quantitative variables were reported with measures of central tendency with prior verification of the assumption of normality using the Shapiro-Wilk test. The groups were compared with Chi2 and Fisher's exact tests for qualitative variables and Kruskal Wallis, Student's t or Mann-Whitney tests for quantitative variables; a p<0.050 was considered significant. Mortality and lethality rates per 1,000 inhabitants were calculated for each month of the study and for the study period. The comparisons were done according to age groups and survival status. Statistical analyses were done using STATA v.14 software.
This project was carried out according to the guidelines set forth in the Declaration of Helsinki 31 and local regulations 32. The data are protected such that none of the enrolled patients can be identified. The local regulations of the Colombian Ministry of Health in Resolution 8430 of 1993, with regard to Chapter I "Ethical aspects of human research," were followed. This study is classified as no risk, and therefore did not require approval by the clinic's medical ethics committee. Access to the research tools is limited to the investigators, in line with Ministry of Health's Article 8 of Resolution 008430 of 1993.
The investigators are responsible for maintaining absolute confidentiality of the information in the medical charts and following the current regulations regarding data handling in the following documents:
Results
Univariate analysis
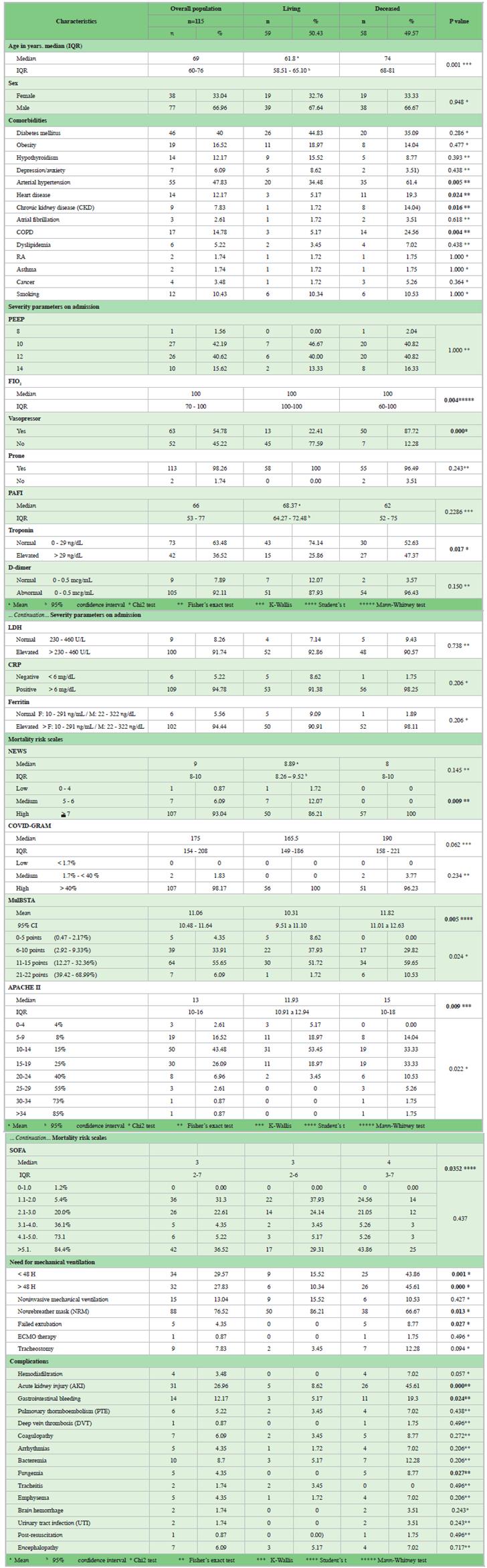
Altogether, 66.96% (n=77) were male patients with a median age of 68 years (Range 58 to 74) Table 1.
The frequency of use of the different ventilation strategies was evaluated in this group of patients, finding that NRBs were required in 76.52% of the cases, 14.7% of whom also required NIV cycles; 9% required IMV < 48 hours after ICU admission and 36.3% required IMV > 48 hours after ICU admission. The remaining 40% only required NRBs throughout their ICU stay; NIV was required in 13.04% of the patients, 6.6% of whom subsequently required IMV <48 hours and 46.6% required IMV > 48 hours after ICU admission; the remaining 46.8% alternated between NRBs and NIV cycles, and 57.36% of the patients required MV, in 29.57% of whom it was instated within the first 48 hours after hospital admission, and in 27.83% after 48 hours. All patients studied in this group required PEEP > 5 cm H2O and more than 90% of the study subjects required PEEP higher than 10, with an FiO2 ranging from 70 to 100%.
The PaO2/FiO2 found in the study population ranged from 53 to 77, and the prone positioning strategy was used in 98% of the patients. With regard to additional procedures required by the patients, 7.83% underwent tracheostomy, 0.87% required ECMO therapy and 4.35% had failed extubation.
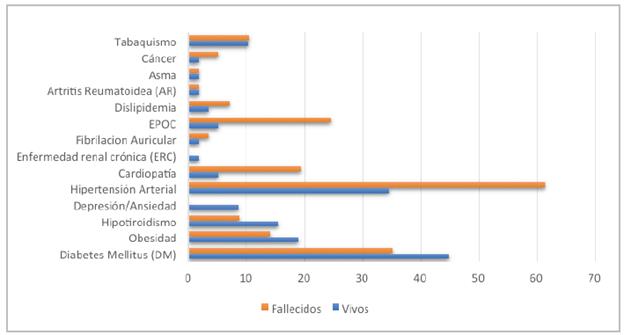
The most common comorbidities in the study population were arterial hypertension (47.83%), diabetes mellitus (40%), obesity (16.52%), chronic obstructive pulmonary disease (14.78%), hypothyroidism (12.17%) and smoking (10.43%) (Figure 2).
Severity parameters like troponin, ferritin, LDH, D-di-mer and CRP were evaluated on admission to the ICU. The need for vasopressor support was also taken into account.
Sixty-three percent of the patients required vasopressors and, for poor prognostic parameters like D-dimer, ferritin, and LDH, more than 90% of the population had values above the normal laboratory range, with the exception of troponin.
Several mortality and severity risk scales were measured, finding that most of the patients had high risk levels, especially on the NEWS2 (93.04% for risk >7); COVID Gram (98.17% for risk > 40%) and SOFA (36.52% for risk >5.1) scales (Table 1).
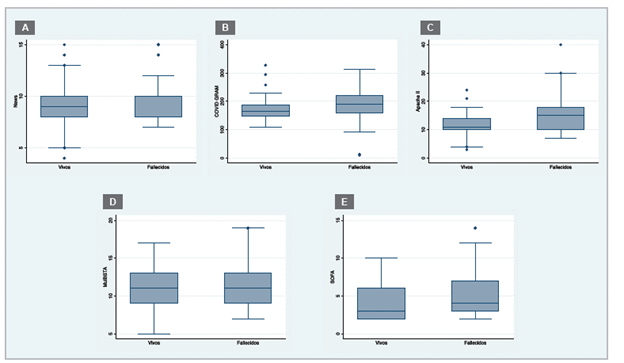
Figure 3 shows the comparison of medians, where higher medians are seen on the COVID Gram, Apache and SOFA scale in the group of deceased patients. It should be noted that, for the other scales evaluated, the figures show equal median values in both groups, but given the normal distribution of the data, the means with their 95% CI and P values were calculated, and are reported in Table 1.
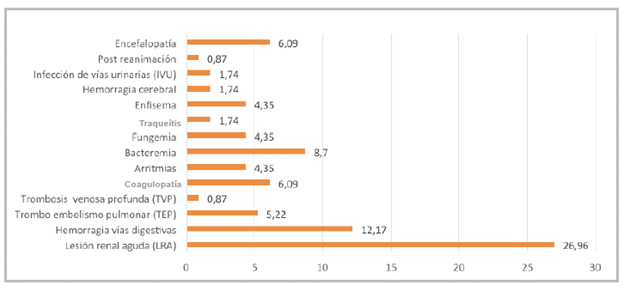
Various complications were found in the study population. The most frequent were acute kidney injury with 26.96% and gastrointestinal bleeding with 12.17%; all of the complications are found in Figure 4. Altogether, 3.48% required continuous veno-venous hemodiafiltration.
Bivariate analysis
The study variables were compared between the living and deceased groups. Significant differences were found in regard to the age of the ARDS patients who died, where the median was 74 years (range: 68 to 71, p=0.000). With regard to severity parameters, a significant difference was only found in troponin elevation in patients who died (p=0.017).
A correlation was found between patients who died and a greater FiO2 requirement, with a significant difference (p=0.004), as well as in patients who required vasopressor support (p=0.000).
Regarding the measurement of mortality risk scales, most were significant (Table 1), except the COVID Gram scale which was not significant in the comparison of medians (p=0.062), nor in the frequency for each level of risk (p=0.234).
The most prevalent comorbidities in the population of those who died were arterial hypertension (61.4%), diabetes mellitus (35.09%), COPD (24.56%) and heart disease (19.3%), with the difference in arterial hypertension (p=0.005), heart disease (p=0.024) and COPD (p=0.004) being significant compared to the living patients.
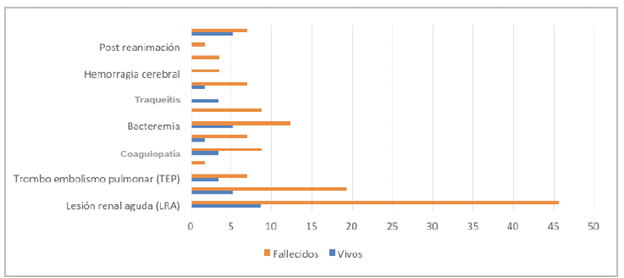
The observed complications were more frequent in the population who died (Figure 5), but only acute kidney injury (p=0.000), gastrointestinal hemorrhage (p=0.024) and fungemia (p=0.027) showed a significant difference compared to those who lived.
Subgroup analysis
Since age was a significant variable in the study population, stratification was done by age groups (under 60 years old and over 60 years old), along with a comparative analysis of the study variables between living and deceased patients. We found that, in those under 60, the significant variables were the need for vasopressor support (p=0.022), PaO2/FiO2 (p=0.021), the need for mechanical ventilation (p=0.001), failed extubation (p=0.040), the need for continuous venovenous hemodiafiltration (p=0.040) and fungemia (p=0.040). On the other hand, in those over 60, the following were significant: COPD (p=0.027), the need for high FiO2 (p=0.029), the need for vasopressor support (p=0.000), the NEWS2 score (p=0.010), the use of NRMs (p=0.000), mechanical ventilation (p=0.000) and acute kidney injury (p=0.000).
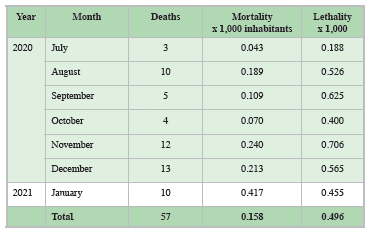
The mortality of patients with severe COVID-19 ARDS who were admitted to the ICU was calculated for each study month, as well as for the study period (Table 2). In Clínica Belén de Fusagasugá' s ICU, the COVID lethality rate was 49 out of 100 patients admitted to the ICU for COVID. Mechanical ventilation, regardless of whether it was begun before or after 48 hours, was found to be significant and seemingly more associated with a greater probability of dying from severe COVID-19 ARDS (Table 2). Mortality and lethality in COVID-19 ARDS patients in the ICU.
Discussion
Lethality varies significantly among COVID-19 patients, from 4.44 to 84.62% in the published case series 33. This variability may be influenced by the difference in the availability of ICU beds in different communities, as well as the variability of ICU admission criteria in each country.
A case series in Canada 34 found a 15% lethality rate, explained by the low need for invasive mechanical ventilation and high ICU admission capacity, where 40% of the patients admitted to the hospital were transferred to the intensive care unit daily. Another retrospective cohort in Wuhan, China 16, which included 191 patients, found a 72% lethality rate in patients admitted to the ICU, reported in January 2020.
According to the Ministry of Health 19, the overall lethality in Colombia is 4.4%. Nationwide, there is a lethality of 3.30%, with three out of 100 positive cases in Colombia dying 35. In Cartagena 36, lethality was found to be 0.97%, taking mild, moderate and severe cases into account.
In this study, lethality in critically ill patients with severe ARDS was 49%, a finding which is comparable with the international literature, considering that our sample only included patients with severe ARDS.
In Cundinamarca, taking the entire population into account, the lethality was 2.70, and in Bogotá it was 2.76 35. However, there is insufficient medical literature available in Colombia of studies on critically ill patients.
The most significant risk factor related to mortality in our study was the need for IMV, as was seen in Wuhan 16 and New York 37 where the mortality rate in patients requiring invasive ventilation was reported to be 97% and 55.3%, respectively. A distinction was made between more than and less than 48 hours, to determine if early initiation of this strategy would affect the patients' outcome; however, there was no significant difference in this study.
Increased mortality in patients with the need for IMV could be explained by multiple reasons; first, patients who require ventilation are more seriously ill; second, mechanical ventilation decreases cardiac output, which, coupled with the need for sedation causes hypotension and the need for vasopressor support, leading to a greater predisposition to complications like arrhythmias or kidney failure 38 and potentially affecting the probability of dying. This, however, does not mean that the best strategy is not to implement invasive ventilation in this type of patients, as it is a necessary support measure.
A relationship with mortality was also found in patients with failed extubation, explained by the fact that these patients probably have myopathy which makes it harder to rehabilitate them and thus affects survival.
In Italy 18, the median PaO2/FiO2 on ICU admission was 160.8, while in our case it was 66, probably explained by most patients' delay in seeking care, information which could not be gathered in this study, which is a limitation. They required higher FiO2 levels during mechanical ventilation and thus the risk of death increased, according to the data gathered.
Another factor associated with increased COVID-19 mortality 1,23 was age; the median age of the study patients was 68; however, the median age among patients who died was 74. This finding is comparable with the international 17,18 and national 9,25,38 literature, as seen in a study at Universidad del Valle 17 which reports that the risk of dying from COVID-19 is 15 times higher in patients over the age of 60.
Despite the literature reporting a higher risk of death in male patients 5,17,18,23 (except for a cohort in the United States 39 which reported a higher proportion of women [55.9%]), in this study, most of the patients were male (66.96% [n=77]), but there was no significant correlation regarding the mortality risk in the study population.
Despite comorbidities like obesity, hypothyroidism and smoking being among the most prevalent in the population, they were not directly correlated with a higher risk of death, while arterial hypertension, diabetes mellitus and COPD were among the most prevalent and were significantly associated with the risk of death, which correlates with the literature 40. And although pre-existent heart disease was not one of the most prevalent, it was correlated with a greater risk of death.
Arterial hypertension has been the most frequently described pre-existing morbidity associated with mortality 20,41, which correlates with our findings. This finding could be related to the primary SARS-CoV2 receptor or angiotensin-converting enzyme 2 (ACE2) 38, as the use of medications which act on the renin-angiotensin-aldosterone system can affect the course of the disease.
The prone positioning strategy was used in 98% of the patients at least once; only in 2% of the patients was it unable to be used due to hemodynamic instability which contrain-dicated this measure. The ventilatory parameters used were based on protective mechanical ventilation.
Several case series 42 describe poor prognostic markers associated with mortality like ferritin, lactate dehydrogenase, troponin, D-dimer, CRP and IL-6, and therefore these were ordered from the onset in all patients (except for IL-6, which was not available) and were taken as an objective in this study. However, it is interesting that only troponin had a statistical association in the population described.
Regarding the risk scales, a cohort in Norway 43 reported a correlation between NEWS2 and mortality, as was seen in this population. Of the evaluated scales, APACHE, SOFA and MuLBSTA were significantly related to mortality, but COVID GRAM was not related. This was contrary to what was published in a study in Spain 44, where the most accurate scale for evaluating the mortality risk was COVD-GRAM, and to findings in the scale's validation studies; further studies are needed to evaluate the validation of this scale in our population. However, it should be noted that the COVID-GRAM scale is a measure designed to predict the risk of critical illness 45 and is not strictly related to mortality, which could explain our results.
These results could be useful for caring for patients with COVID-19, because they help recognize these variables in the population and thus increase the quality of care in this type of patients, to avoid a fatal outcome. The study also describes a population which had not been evaluated previously. No variables that could reduce the mortality risk were found in this study.
Limitations
This study had several limitations associated with its type of design. Being a retrospective study, some of the data were incomplete or unavailable, thus affecting the measurement and report of some of the variables of interest which were unable to be evaluated. Another limitation was the lack of proper chart completion and clarity regarding the patients' clinical picture, with many of them coming from rural areas or being referred by ambulance with ventilation without much information regarding the initial clinical picture due to the health emergency and lack of ICU beds for all the patients in the nation's capital at the beginning of the pandemic. Thus, the time of onset of the symptoms could not be included in the study variables. However, this missing information was dealt with by reviewing the doctors' shift change reports, nursing statistics and the clinic's functional registry, which allowed the information to be cross-checked its rigor determined.
Furthermore, mortality was assessed at hospital discharge, with no mortality information after discharge, due to the difficulty in communicating with the entire population described in this article.
We were unable to measure laboratory tests like interleu-kins to compare them with the national literature, as these reagents are not available in the institution and these tests are not cost effective for the healthcare system.
In addition, we used available information published by the Colombian government, and this information cannot be verified. Changes may have occurred in the time elapsed since the information was reviewed.
Conclusions
The COVID-19 lethality rate was 49%, which is comparable with what is described in the literature, considering the severity of the cases included. Among the factors which most contributed to this outcome were the need for invasive mechanical ventilation, and comorbidities like arterial hypertension, diabetes and COPD. A correlation was found between the severity scales used and mortality, except for COVID-GRAM. Age is a factor which strongly affects mortality.











 text in
text in