INTRODUCTION
Mastitis is the inflammation of the mammary gland, caused by the invasion and destruction of the mammary glandular tissue due to the pathogenic action of microorganisms. It is a major problem in specialized dairies herds due to the direct economic losses that it causes through the decrease of milk production, the poor quality of raw milk, increase in culling rate of animals and additional expense for treatment and labor costs. In addition to the milk that is lost due to antibiotic treatment. (Andrade-Becerra et al. 2012; Taponen et al. 2016; Haubert et al. 2017; Petersson-Wolfe et al. 2018).
Mastitis has special economic importance, it is estimated that the losses in countries like India are $1.1 billion, the United States $ 2 billion, United Kingdom $ 371 million and worldwide $ 35 billion. In Colombia, the estimated annual losses are from $ 1,250-25,000 dollars, caused by the prevalence of mastitis in cows and dairy farms, respectively. (Haubert et al. 2017; Ortíz-Duran et al. 2017).
Mastitis can be differentiated into clinical and subclinical mastitis. The first form produces noticeable inflammation of the mammary gland and alterations occur in the milk due to the presence of bacteria and cells participating in the inflammatory process. In subclinical mastitis, there are no visible changes in the mammary gland, but milk production decreases, there is the presence of bacteria in the milk and the milk properties change due to the enzymatic processes (Ferrero et al. 2014; Caggiano et al. 2016; Andrade-Becerra et al. 2018).
According to its infectious etiology, mastitis can also be divided into contagious and environmental forms. Contagious mastitis is caused by microorganisms such as Staphylococcus aureus, Streptococcus agalactiae, Arcanobacterium pyogenes and Mycoplasma spp.; and its reservoirs are the mammary gland and the milk of infected cows. Its transmission can occur at the time ofmilking by poor practices such as the sharing oftowels to wash and dry teats; by the contaminated hands of farmworkers or by the sharing of non-disinfected teat liners between cows in the milking (Blowey and Edmondson 2010; Andrade-Becerra et al. 2014).
Environmental mastitis is caused by Gram-negative germs, normally found in the environment such as Escherichia coli, Klebsiella spp., Enterobacter spp., Serratia spp., Pseudomonas spp., and Proteus spp. and some Gram-positive bacteria such as Streptococcus uberis and Streptococcus dysgalactiae, which cause mild and moderate forms of mastitis and within the rare germs are yeasts and molds (Haubert et al. 2017). Also, mastitis can be due yeast and molds, but this presentation in dairy herds is low (Williamson and Di Menna 2007).
The objective of this study was to determine the bacterial etiological agents and infectious fungal causes of subclinical mastitis, and its prevalence, in dairy farms in the Highlands of Boyacá.
MATERIALS AND METHODS
Determination and characteristics of the farms included
By means of a convenient probabilistic sampling ofand by means ofa retrospective longitudinal descriptive study during the years 2016-2018 (Martin et al. 2010), 25 dairy farms were chosen, located between 2300 and 2800 meters above sea level, with average annual temperatures of 13 °C and rainfall from 800-1200 mm/year (Institute of Hydrology, Meteorology and Environmental Studies, 2018). All the farms had mechanical milking twice daily. The genetic basis of the cattle was 100% Holstein Friesian. The main grass was the Kikuyu (Cenchrus clandestinum). 1108 animals were involved, cows with 2-4 calving, with a total of 4432 teats. The average milk production was 4300 L /cow/year and the number of somatic cells in the milk tank on average was 330,000 cel / mL.
Sampling and transport
From January 2016 to December 2018, California Mastitis Test (CMT) tests were performed in all quarters. Previous to this test, a complete clinical analysis was performed in every mammary gland, and no one apparent changes were discovered on its. The CMT was performed following this: the first stream of milk was discarded and then a few streams of milk (5 mL) were collected in corresponding paddle wells, then an equal amount of commer-cial reagent was added to each cup. A gentle circular movement was applied in a horizontal plane for 20 seconds to mix milk with reagent. The results were scored and interpreted as either 0 (negative or no thickening of the mixture), Trace (slight thickening), 1 (or +, distinct thickening but no tendency to form a gel), 2 (++, or immediate thickening, with a slight gel formation), or 3(+++, or gel is formed and surface of the mixture becomes elevated) to asses the inflammatory response based on the viscosity of the gel formed by mixing reagent with milk (Tolosa et al. 2013; Godden et al. 2017; Mendoza et al. 2017).
In all the teats that were positive (CMT > o 2+) milk samples were stored in new and sterile plastic bags (Whirl-pack), after cleaning and disinfecting the tip of the teat, the procedure described by the National Mastitis Council was followed (NMC 2009).
Teats were washed, dried and disinfected with a soap solution, then rinsed with sterile water and dried with sterile gauze, disinfected with iodine solution. Once asepsis was completed, the sample was collected in Whirl-pack bags. The collected samples were kept and transported in refrigeration until they arrived at the laboratory for analysis.
Bacteriological tests and bacterial identification
The samples were taken by a veterinarian and transported in refrigeration to the laboratory of milk quality analysis and mastitis control, as well as to the veterinary microbiology laboratory of the Universidad Pedagógica y Tecnológica de Colombia in Tunja. The laboratory of analysis ofmilk quality and mastitis control, as well as the Veterinary Microbiology lab, proceed in a routine diagnosis, as well as with the isolation of non-common microorganisms following the methodology proposed in the Laboratory Handbook on Bovine Mastitis, by the National Council of Mastitis of the United States (NMC 2017).
The milk samples were cultivated in a blood agar base (ovine blood), to determine the type of hemolysis. Also, MacConkey agar was used to cultivate the samples. These two agars were incubated between 24-48 hours. After this time, Gram coloration was performed, to classify samples into Gram-positive and Gram-negative and cocci or bacilli. The Gram-positive cocci were tested using catalase and differentiated as positive and negative coagulase. Then the colony was cultivated in ID32 STAPH, to identify and confirm gender and species, thus Staphylococcus aureus differed from other Positive Coagulase Staphylococcus. For Streptococcus, CAMP, hydrolysis of esculin, hippurate and inulin, and growth in NaCl was used. For Gram-negative bacilli: oxidase, indole, triple sugar, Methyl Red-Voges Proskauer (RM-VP), Lys Agar decarboxylase (LIA), urea and citrate tests were used. All samples were cultivated in Saboureaud agar for yeast and molds.
Statistical analysis
The data obtained were recorded in the database using dBASE 5.0 and were analyzed statistically using SPSS Windows 7. Descriptive statistics were used. The results of the statistical analysis were interpreted with a confidence level of 95%.
RESULTS
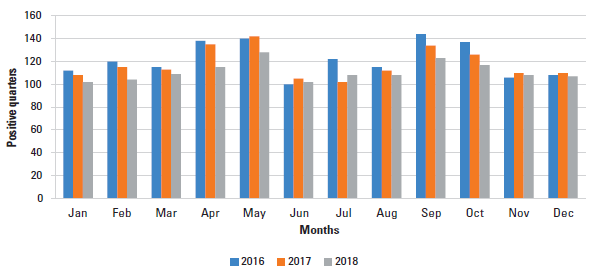
The results of the positive teats during the study are recorded in Figure 1. The results show an increase in positive teats in the months of April-May and September-October (months with the highest rainfall) during the 3 years of the study, for 2016 the number of positive quarters in April and May was 138 and 149 respectively, for 2017 the results was 135 and 142, and 2018 115 for April and 128 for May.
On the other hand, generally, the months with the lowest prevalence in the three years were January, June, July, November and December (lowest rainfall). In 2016, the prevalence of positive quarters for January was 112, June 100, November 106 and December 108. For 2017, in January the number of positive quarters 108, June 105, July 102, November and December 110. For 2018, in January and February the results were 102 and 104 respectively, in June and July 102 and 108, and November and December 108 and 107 positive quarters.
The Table 1 shows the microbiological results for each sample analyzed during the study. For the three years the major percentage of the samples did not show microbiological growth. In 2016 this percentage was 54.75%, in 2017 48.88% and in 2018 60.20%. The Streptococcus agalactiae was the most prevalent microorganism in all three years of sampling, in 2016 it had a prevalence of 17.37%, in 2017 13.77% and in 2018 12.28%. Followed by Staphylococcus aureus which has a prevalence of 10.16% in 2016, 11.55% in 2017 and 11.59% in 2018. The next microorganisms in the list was the others Streptococcus which had a prevalence of 3.93% in 2016, 6.22% in 2017 and 3.11% in 2018. The other microorganisms like: others Staphylococcus CP, Staphylococcus CN, Arcanobacterium pyogenes , mixed infection with Staphylococcus aureus and Streptococcus agalactiae, E. coli, Corynebacterium bovis and yeast had prevalence lower than 6%.
TABLE 1 Shows the microbiological results for each of the samples analyzed during the study.
| Years of sampling | 2016 | 2017 | 2018 | |||
|---|---|---|---|---|---|---|
| Total number of test | 305 | 225 | 578 | |||
| Number | Percentage | Number | Percentage | Number | Percentage | |
| No Growth | 167 | 54.75% | 110 | 48.88% | 348 | 60.20% |
| Arcanobacterium pyogenes | 6 | 1.96% | 7 | 3.11% | 10 | 1.73% |
| S. agalactiae | 53 | 17.37% | 31 | 13.77% | 71 | 12.28% |
| Others Streptococcus | 12 | 3.93% | 14 | 6.22% | 18 | 3.11% |
| Staphylococcus aureus | 31 | 10.16% | 26 | 11.55% | 67 | 11.59% |
| Others Staphylococcus CP | 8 | 2.62% | 1 | 0.44% | 9 | 1.55% |
| Staphylococcus CN | 6 | 1.96% | 4 | 1.77% | 19 | 3.29% |
| S. aureus +S. agalactiae | 5 | 1.63% | 9 | 4% | 11 | 1.90% |
| E. coli | 3 | 0.98% | 6 | 2.66% | 9 | 1.55% |
| Corynebacterium bovis | 6 | 1.96% | 13 | 5.77% | 10 | 1.73% |
| Yeast | 8 | 2.62% | 4 | 1.77% | 6 | 1.03% |
| Total growth | 138 | 45.19% | 115 | 51.06% | 230 | 39.76% |
DISCUSSION
Many factors are associated with the presence of mastitis, even in the absence of bacterial growth, these are usually traumatic damages (lacerations, cuts, injuries), chemical irritants, external conditions, where the teats or the udder, in general, are affected, thus increasing the somatic cell count, (Bhutto et al. 2010; Andrade-Becerra et al. 2018), this could explain the presence of a CMT +2 but without growth of bacterium colonies.
The months when the prevalence of mastitis increased were between April and May; and September and October, due to the rainy season which can cause problems with contamination of the udder (Andrade-Becerra et al. 2012), these data are similar to those reported by Andrade-Becerra et al. (2014) in the Highland of Boyacá, evaluating farms under similar conditions.
The total prevalence of mastitis in the three years of study is low concerning the value reported by Santivañez et al. (2013) which was 72.25% in the Peruvian Andes, also using CMT for the diagnosis of intramammary infection. Similarly, Ruiz et al. (2011) in Brazil isolated pathogenic microorganisms in 61% of the samples evaluated, a value that is higher than reported in this study with 15.81% for 2016, 9.94% for 2017 and 21.24% for 2018. In Uruguay, Gianneechini et al. (2014), in similar productive conditions, with an average prevalence of54.2%, using somatic cell count (SCC) (> 300,000 cells / mL), which is similar to those reported in this study for the year 2017, and less than the years 2016 and 2018.
In the North Coast of Colombia, Calderón et al. (2011) reported a prevalence of 92.21% using CMT, a value that is higher than that reported in this study for any of the three years. In Antioquia, Trujillo et al. (2011) determined a prevalence of 42.4% using CMT and SCC, which is similar to what was reported in this study for 2016 and 2018, but less than was reported for 2017.
Calderón and Rodriguez (2008) in Boyacá reported prevalence, using CMT, of34.40%, a value that is lower than that reported in this study for any of the three years analyzed. Andrade-Becerra et al. (2014) determined an average prevalence for three years of that study (2010-20112012) of 36.7%, a value that is lower than that reported in this study for any of the three years evaluated.
Bacteria are the most important microorganisms that generate mastitis in dairy herds, and can act like an opportunistic pathogen or contagious pathogen. Due to its presence in the skin and mucous membranes, Trueperella (Arcanobacterium) pyogenes is an opportunistic pathogen that can contaminate the mammary gland and produce mastitis (Rodriguez et al. 2015), in this study, the CMT value from de samples with growth of these microorganisms was +2 and +3. However, this pathogen is seldom found in samples from mastitis cows, Gianneechini et al. (2014) only reported it at 0.3%, while for this study the results were higher. Concerning the reported by Andrade-Becerra et al. (2014), it found a value for the year 2010 of1.1%; for 2011 of 2.2% and 2012 of 0.5% with similar values for CMT; values that are very similar but lower than those found in this study even with farms in similar conditions of milking practices.
Streptococcus agalactiae is a highly contagious pathogen in cows with mastitis, having a common transmission in herds that allow the microorganism to colonize, invade and it replicates in the udder (Carvalho-Castro et al. 2017. In Brazil, Oliveira et al. (2015), reported a presence of 5% in cows with mastitis, a value similar to that reported by Mekonnen et al. (2017) in Ethiopia of 4%, and both are less than reported in this study. Both studies have been realized in dairy herds with mechanical milking like in this study. Generally, this pathogen can be transited between cows trough milking machine, so, differences between results can be due to differences in cleaning practices. The results of CMT in both studies indicates subclinical mastitis, similar to reported here.
The values reported for this pathogen are lower than found by Ramirez et al. (2011) who reported a prevalence of 34%, and also was the pathogen mostly isolated as in the present study. Calderón et al. (2011) in Montería-Colombia, found 2.1%, which was one of the lowest values in this study. In Boyacá, Calderón and Rodriguez (2008) found a prevalence of 6.84% and Andrade-Becerra et al. (2014) in 2010 a prevalence of 9.7%, 9.1% in 2011 and 10.4% in 2012, all this value is lower than reported in this study for all years. In Uruguay, Gianneechini et al. (2014) reported a prevalence of only 0.6%, a value lower than that reported in this study. Ruiz et al. (2011) in Brazil found a prevalence of 12.9%; in India, Ranjaan et al. (2011) found a prevalence of 5.9%, in China, Yuan et al. (2012) found a prevalence of 15.5% all these studies were performed in herds with mechanical milking, and shows similar epidemiology, which can be due similar practices of cleaning of milking machines.
Staphylococcus aureus is one of the most commonly reported pathogens worldwide as a cause of mastitis, due to its pathogenic characteristics (exotoxins) and it is easily transmitted to the teat and is especially important due to the generation of resistance to antibiotics (Haubert et al. 2017). Generally, mastitis due to this microorganism is clinical; however, due to the absence of clinical changes in mammary glands evaluated here the mastitis that it caused here was subclinical due the CMT result was +2.
Gianneechini et al. (2014), in Uruguay, determined that this microorganism was the one that was most isolated from samples from cows with clinical mastitis, with a prevalence of 23.1%; double what was reported in this study. In India, Ranjaan et al. (2011) determined a prevalence of 27.37%, a value that is more than double that reported in this study for any of the three years evaluated. In Brazil, Ruiz et al. (2011), found it in 36.4% in mechanical milking, results that are higher than reported in this study, and the form of mastitis also was different for any study.
In Colombia, Trujillo et al. (2011) in Antioquia determined a prevalence of 10.3%, a result that is very similar to that reported in this study for any of the three years. Calderón et al. (2011) determined it in 87.56% of the samples evaluated in Monteria, a value that is higher than that reported in this study for any of the three years, possibly due to the differences between routines of milking.
In Boyacá, Calderón and Rodriguez (2008), found a prevalence of 29.09%. On the other hand, Trujillo et al. (2011) found it in 61.76% CMT +2 and in 29.41% CMT +3, results that are higher than those reported in this study, and with similar results of CMT; for the last three investigations, it was determined that this was the pathogen with the highest presentation, contrary to that reported in this study. In Boyacá in 2012, Andrade-Becerra et al. (2014) found a prevalence of 10.7%, a result that is lower than what was determined in this study for 2017 and 2018, but similar to 2016.
In the case of other Positive Coagulase Staphylococcus, which due to its presence in the skin of the teats and the udder it facilitates the contamination of the teats canal and the generation of mastitis, generally subclinical. In Boyacá, Calderón and Rodriguez (2008) found a prevalence of 4.04%, a value higher than that reported in this study; for 2016 this value is above 1.42%; 3.6% in 2017 and 2.49% for 2018. Likewise, Andrade-Becerra et al. (2014) determined it at 0.6% for 2010, 0.5% for 2011 and 0.0% in 2012, values that are below what was found in this study, even when production conditions were similar.
Negative Coagulase Staphylococcus are environmental pathogens found in sites such as the apex of the teats and are frequently isolated from quarters with subclinical mastitis worldwide (Mekonen et al. 2017), and its epidemiology can vary due the cleaning process at the milking time, also due cleaning of the milking equipment. Calderón and Rodriguez (2008), in the same region, found a prevalence of 11.75%, a value that is greater than that reported in this study; however, the same author in 2011, only isolated it in 0.3% of the samples in the Northern Colombian zone. On the other hand, Trujillo et al. (2011), in Antioquia isolated these microorganisms in 23%, and Ramirez et al. (2011), reported prevalence 10.2%. In Uruguay, Gianneechini et al. (2014) found a prevalence of 5% for clinical mastitis and 6% for subclinical mastitis, data greater than those in this study. Similarly, in India, Ranjaan et al. (2011) found a prevalence of 12.63%. Like was mention before cleaning practices are the most determinant factor for the presentation of these microorganisms in dairy herds.
The only mixed infection found in this study was Staphylococcus aureus and Streptococcus agalactiae. Both are major pathogens causing mastitis, generally with extensive damage to the glandular tissue. Similarly, in Uruguay, Gianneechini et al. (2014), determined it in 0.3% of the samples of clinical mastitis, and in 0.7% of subclinical mastitis, results much lower than those of results much lower than those determined in this investigation. Likewise, Calderón and Rodriguez (2008) determined that this type of mixed infection was the most frequent in dairy herds of the department of Boyacá, determining the prevalence of 1.2%. Andrade-Becerra et al. (2014) in their study, determined a 0.9% prevalence for this mixed infection in 2010 and 2011, and 0.5% in 2012; values that are lower than those reported in this study even when the herds had similar conditions, which show differences in milking practices.
Mastitis due E. coli is reported worldwide and is clinically important due to the possibility of endotoxic shock in the cow if there is a large bacterial presence. Its pathogenicity factors (endotoxins) are responsible for this problem (Yangliang et al. 2016; Zhang et al. 2017). Generally, mastitis due E. coli is clinical, but this can vary due the number of microorganisms in the mammary gland, also the number of endotoxins presents (Andrade-Becerra et al. 2012). Its presentation is related with poor cleaning practices at the milking time.
In Uruguay, Gianneechini et al. (2014) reported it in 1.5% of clinical mastitis samples E. coli but did not find E. coli in subclinical mastitis, which is similar to what was reported in this study for 2018; lower than for 2017 and higher than in 2016. In Antioquia, Trujillo et al. (2011) reported it in 1.3% for clinical mastitis, similar to reported in 2018. In Montería, (Calderón et al. 2011), reported it in 0.60% in double purpose farms, a result inferior to the one reported here. In An-tioquia (Ramirez et al. 2011) reported E. coli at 0.9% similar to what was reported in 2016, but lower in 2017 and 2018.
Among the rare germs isolated from mastitis are the yeasts, which enter the teat canal due to anthropogenic factors (introduction of a contaminated cannula) and are very rare worldwide (Andrade-Becerra et al. 2012). In the current study, they were determined at 2.62% in 2015; 1.77% in 2016 and 1.03% in 2017 of samples; values that are inferior to that reported by Ranjaan et al. (2011) who in India reported mastitis due to yeasts in 3.15% of the herds. Gianneechini et al. (2014), reported clinical yeast mastitis in 0.6% of the animals sampled, and none in subclinical mastitis, thus showing the aggressiveness of yeast mastitis. Andrade-Becerra et al. (2014) report it in a maximum of 0.9% of the samples, in a similar study. Ramirez et al. (2011) reported Candida spp. in 0.6% of cows with clinical mastitis.
Corynebacterium bovis generates moderate forms of mastitis; it is easily transmitted when there are deficient milking techniques and poor cleaning of the milking equipment. In 2016 its prevalence was 1.96%; 5.77% in 2017 and 1.73 in 2018; however, these results are lower than reported in Boyacá by Calderón and Rodriguez (2008), who reported it in 8.44% of the milk samples. In Brazil, Ruiz et al. 2011 reported this pathogen in 45% of clinical mastitis. In Antioquia, Ramirez et al. 2011 reported it in 8.6% of the teats affected a result higher than the one given in this study. In Monteria, Calderón et al. 2011 found a prevalence of 2.13% in dual-purpose farms, higher than in 2016 and 2018, bur lower than in 2017. In Antioquia Trujillo et al. (2011) found a prevalence of 1.3% a result lower than all those found in all the years evaluated.
CONCLUSIONS
There was an increase in the prevalence of infected teats corresponding to the months (April, May, September, and October) of increased rainfall in the Highlands of Boyacá. The infectious pathogens like Staphylococcus aureus and Streptococcus agalactiae causing mastitis were the most prevalent, more than the environmental ones. The etiological agents vary from one farm to others, even in the same geographical region and the same milking practices.