Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Colombian Journal of Anestesiology
versión impresa ISSN 0120-3347
Rev. colomb. anestesiol. vol.41 no.1 Bogotá ene./mar. 2013
https://doi.org/10.1016/j.rca.2012.08.002
http://dx.doi.org/10.1016/j.rcae.2012.08.004
Efficacy of anesthetic premedication in pediatric patients using oral midazolam and acetaminophen. Observational study
Eficacia de la premedicación anestésica en el paciente pediátrico con midazolam oral y acetaminofén. Estudio observacional
Luz María Gómez Ba, Federico Ocampo Ab, Jaime Andrés Orozco Ac, Juliana Caicedo Sc
a Anesthesiologist, Masters in Epidemiology in Clinical Epidemiology, Associated Professor, Universidad de Caldas, Manizales, Colombia
b Specialist in Anesthesiology, Assistant Professor, Universidad de Caldas, Manizales, Colombia
c Third Year Anesthesiology Resident, Universidad de Caldas, Manizales, Colombia
Please cite this article as: Gómez B LM, et al. Eficacia de la premedicación anestésica en el paciente pediátrico con midazolam oral y
acetaminofén. Estudio observacional. Rev Colomb Anestesiol. 2013;41:4-9.
Corresponding author at: Calle 81B N.◦ 25 - 41. Conjunto Bosques de la Sierra, casa 1, Manizales, Colombia.
E-mail address: lagomezco@yahoo.com (L.M. Gómez B).
ARTICLE INFO
Article history: Received 6 February 2012 - Accepted 6 August 2012
Abstract
Anesthetic premedication with midazolam helps reduce anxiety in the children and the
parents, the need for analgesic use, and the development of negative psychological events
during the postoperative period; it also results in shorter inhalation induction and orotracheal
intubation. Compounded preparations have been developed using ampoules for
parenteral administration mixed with flavor modifiers in order to improve acceptance. To
determine the efficacy of premedication using a mix of midazolam plus acetaminophen, a
prospective descriptive observational study was conducted in 216 children ASAI or II, scheduled
for surgical or diagnostic procedures requiring general anesthesia. Anxiety-sedation
scales were given (Modified Yale scale and RASS), and tolerance to separation from the
parents was assessed.
Results: The RASS scale applied at the time of induction showed that 92% of the patients
were at an appropriate level of sedation to tolerate facemask inhalation induction, and 86%
of patients tolerated well their separation from their parents. It was found that age, gender,
education, socioeconomic status, pre-anesthetic check type (telephonic or in person), or a
history of previous anesthesia, did not have a statistically significant correlation with the
degree of anxiety-sedation.
Conclusions: Premedication with a compounded preparation does reduce anxiety at the time
of separating the child from its parents, and allows a good acceptance of the inhaled anesthetic
induction.
Keywords: Midazolam, Premedication, Anesthesia, Anxiety.
© 2012 Sociedad Colombiana de Anestesiología y Reanimación. Published by Elsevier España, S.L. All rights reserved.
Resumen
La premedicación anestésica con midazolam, permite disminuir la ansiedad de los niños y los padres así como los requerimientos analgésicos, la aparición de eventos psicológicos negativos en el postoperatorio, y acorta los tiempos de inducción inhalatoria de la intubación orotraqueal. Se han desarrollado preparaciones magistrales utilizando ampollas de administración parenteral mezcladas con sustancias que modifican su sabor para mejorar la aceptación. Para determinar la eficacia de la premedicación con midazolam mezclado con acetaminofén se realizó un estudio observacional descriptivo prospectivo en 216 niños ASAI o II sometidos a procedimientos quirúrgicos o diagnósticos que requerían anestesia general; se aplicaron escalas de ansiedad-sedación (Yale modificada y RASS) y se valoró la tolerancia a la separación de los padres.
Resultados:
La escala de RASS aplicada al momento de la inducción evidenció que el 92% de los pacientes se encontraban en un grado adecuado de sedación para tolerar la máscara facial y la inducción inhalatoria, y además el 86% de los pacientes toleró de manera adecuada la separación de sus padres. El 61,6% de los pacientes se encontraban con un grado adecuado de sedación ansiólisis con la escala de Yale, previo al momento de la separación de los padres. Edad, género, escolaridad, estrato socioeconómico, tipo de valoración preanestésica o antecedente de anestesia no se correlacionaron con el grado de ansiedad-sedación.
Conclusiones: La premedicación con la mezcla magistral utilizada disminuye la ansiedad en el momento en que el niño se separa de sus padres y permite una buena aceptación de la inducción anestésica inhalada.
Palabras clave: Midazolam, Premedicación, Anestesia, Ansiedad.
© 2012 Sociedad Colombiana de Anestesiología y Reanimación. Publicado por Elsevier España, S.L. Todos los derechos reservados.
Introduction
Anesthetic premedication is a frequent practice in pediatric anesthesia services. It has been shown to reduce anxiety in the children and their parents at the time they are taken to the operating room, the analgesic requirements, and the time required for inhaled induction and orotracheal intubation. It has also been found to prevent the development of negative psychological events during the post-operative period.1, 2, 3.
The use of pharmacological premedication has shown to be more cost-effective for controlling anxiety when compared with the use of non-pharmacological means such as the presence of the parents during induction, or behavioral preparation programs before surgery.3, 4
Midazolam has been used extensively for pharmacological premedication, with adequate results.5, 6, 7 Considering that there is no oral midazolam in our setting, compounding has been done using ampoules for parenteral administration mixed with some flavor modifiers in order to improve acceptance by the children and also to avoid the anxiety caused by needles.6, 8, 9
At the Red Cross Children's University Hospital in Manizales, a compounded preparation has been used since 2000, consisting of a mix of midazolam ampoules 15mg/3ml plus acetaminophen suspension 150mg/5ml. At the institution, the mix is known as “midazophen”, and after it is prepared it consists of midazolam 1mg/ml and acetaminophen 24mg/ml. The dose used is half the body weight in cubic centimeters, which is equal to 0.5mg/kg of oral midazolam and 12mg/kg of acetaminophen. The dose is given orally to patients scheduled for elective surgery. The objective of this descriptive study is to assess the efficacy of this premedication, measuring the degree of anxiety in the children when they are separated from their parents and, in particular, the degree of sedation obtained at the time of inhaled induction.
Materials and methodsAfter approval by the Ethics Review Board of the Children's Hospital, a prospective descriptive observational study was undertaken with 216 pediatric patients scheduled for surgical or diagnostic procedures requiring anesthesia at the Rafael Henao Toro Children's Hospital in Manizales (Caldas, Colombia), a Level III healthcare institution.
All patients that met the inclusion criteria between September 2010 and January 2011 were included.
Informed consent was obtained for the observation and the review of the clinical record from the guardians of the children. The inclusion criteria were patients ASA I or II, under 8 years of age, scheduled for elective surgery or diagnostic procedures requiring anesthesia, and who were prescribed anxiolytic premedication with midazolam plus acetaminophen by the anesthesiologist. The presence of a known malignancy or of a mental disease was considered as an exclusion criterion.
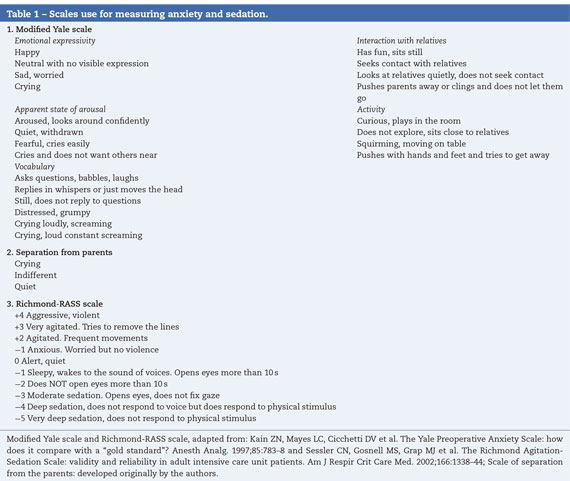
During the preoperative assessment, the anesthesiologist gathered demographic information (age, gender, weight, schooling and socioeconomic status), aside from the usual information for the anesthesia record. The information was recorded in the instrument designed for the study. Most patients coming from areas located far away from the city of Manizales received a phone call a few days before the procedure in order to gather information about their history, and to determine the use of midazolam plus acetaminophen. On the day of the surgery, based on the information already gathered, the patients arrived with their guardians at the Ambulatory Surgery services where they were given the indicated dose of the compounded mix. Before they were taken to the operating room, the patients were again assessed by the attending anesthetist, and given the modified Yale scale. The degree of anxiety at the time of separation from the parents was recorded also (see Tabla 1 for the anxiety assessment scales). Patients were taken on a stretcher to the operating room, and after setting up basic monitoring, inhaled induction was initiated using sevoflurane. At that point (1min), the Richmond-RASS sedation-agitation scale was applied (see Tabla 1). The anesthetic and surgical procedures were carried out in accordance with the institutional standards, and no other measurements were made. Before starting data collection, a pilot test was conducted with 15 cases, and this allowed revision of some technical issues of the tool.
Modified Yale scale and Richmond-RASS scale, adapted from: Kain ZN, Mayes LC, Cicchetti DV et al. The Yale Preoperative Anxiety Scale: how does it compare with a “gold standard”? Anesth Analg. 1997;85:783-8 and Sessler CN, Gosnell MS, Grap MJ et al. The Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002;166:1338-44; Scale of separation from the parents: developed originally by the authors.
Once the information was collected, it was analyzed using the statistical SPSS package. The three outcome variables analyzed were the three sedation and anxiety measurement scores used at three different points of time. The adequate or optimal levels for the three scales were as follows: values ranging between 23.4 and 30 on the Yale scale, a quiet or indifferent child at the time of separation for the degree of anxiety, and a score of 0 or −1 on the Richmond-RASS scale at the time of induction.
A characterization of the population, social and demographic data was performed for the statistical analysis, using descriptive statistical tools such as the mean and the standard deviation.
The social, demographic, medical and anesthetic variables included in the form were correlated with the outcome variables of sedation efficacy using the Chi-Square test.
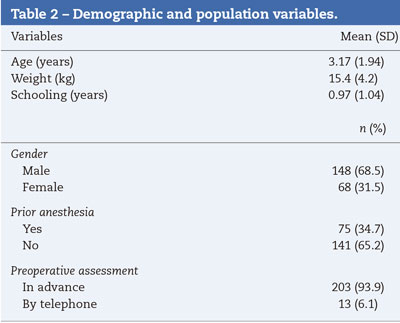
ResultsThe sample collected included 216 patients ranging between 6 months and 8 years of age. Of these, 31.5% (68) were females and 68.5% (148) were males. A description of the demographic variables of the study population is shown in Tabla 2.
The application of the Yale scale showed adequate sedation and anxiolysis in 61.6% of the patients. It is worth noting that at the time of the evaluation, the time elapsed between the moment the drug was given until the scale was applied was within an ideal range (15-90min) only in 25% of the children. Moreover, of the 55 patients in whom the administration interval was appropriate, 60% were found to be anxious, and 40% were not anxious. These variations preclude any valid conclusions for this phase.
When the sedation-anxiolysis scale was applied at the time the children were separated from their parents, it showed that 86% (186) of the children were indifferent or quiet. At this stage, there was no evaluation of the time elapsed from the moment the midazolam-acetaminophen mix was given. However, this must have happened approximately 10min after the previous phase.
The Richmond-RASS scale applied at the time of induction showed that 70% (152) of the patients had adequate sedation (score between −1 and 0), which resulted in easy and quiet acceptance of the facemask. When the 39 children whose score on this scale was +1 are added to this group, the percentage rises to 92%. Tabla 3 shows the data obtained for each score on this scale.
In terms of the time elapsed between the administration of the drug and the induction of general anesthesia, optimum time was achieved in 89% (192) of the patients (ranging from 15 to 90min). Of the patients in whom optimum time was not achieved, 12 patients had less than 13min between the moment they were given the compounded mix and the time of anesthesia induction.
There was no statistically significant correlation among variables such as age, gender, schooling, socioeconomic status, type of anesthetic check (by telephone or in person), or a history of prior anesthesia, and the presence of anxiety at the time of applying the Yale scale, or with the degree of sedation at the time of anesthesia induction.
DiscussionSedation obtained by means of pre-medication enhances pediatric patient cooperation at the times of highest anxiety during the perioperative period - separation from the parents and anesthetic induction - and creates a tear-free environment and a more reassuring atmosphere for the other patients, the parents and the caregivers. An additional benefit is a lower incidence of post-operative emotional disturbances that might create emotional morbidity in the long run.10, 14
Several strategies have been used to obtain adequate sedation. Among them, one of the most effective is the pharmacological strategy, midazolam being one of the drugs of choice because of ease of administration, safety, good bioavailability when given orally, and because it does not delay emergence from anesthesia or the time to discharge from the recovery unit.11, 2, 12
Reducing perioperative anxiety must be one of the most important objectives in pediatric anesthesia, because anxiety has been associated with postoperative adverse events such as increased pain and negative behavioral changes, including psychomotor agitation at emergence, crying, disorientation, post-operative delirium, sleep disorders and avoidance behaviors in medical and hospital environments, which may last even up to 2 weeks after the procedure.13, 14
The modified Yale scale was applied prior to separation from the parents, in the waiting room, in order to assess the presence or absence of anxiety at that point in time,13and anxiety was found in 61.6% of patients. This might be explained because the time elapsed between the administration of oral midazolam and that point in time was not adequate in most cases (14min in average). The time elapsed between the administration of oral midazolam and the onset of action has been described as 5-10min, with a peak clinical effect at 20-30min, and waning between 45 and 90min. However, of the 55 children in whom the time was adequate, 33 (33/55=60%) were anxious and 22 (22/55=40%) were not. Consequently, there probably are other conditioning factors that were not considered, such as those mentioned in some studies that show that individual behavioral disorders are directly related with failure of adequate sedation16; in our study, the evaluation of existing personality traits was not included as an objective. On the other hand, it is important to consider that the Yale scale was designed to determine whether anxiety is present or not, but not to determine its degree.13, 15Consequently, several children could have experienced imperceptible degrees of anxiolysis. Studies with the participation of psychology professionals might provide more specific information in this regard.
As stated previously, there are several critical moments when sedation is more important. The first one is when the child is separated from its parents before entering the operating room, and the next one is during inhaled anesthetic induction. 15 In our study, at the time of separation from their parents, 86% of the children appeared quiet. Other studies, like the one by Rosenbaum et al. have shown that seeing a quiet child improves parental satisfaction.10
Another moment that might be traumatic and stressful for the child and might create psychological sequelae is anesthetic induction with the use of a facemask. Several strategies have been used to overcome this problem, with varying degrees of success. 15, 16, 17, 18 Our study found that 70.4% of the patients showed good acceptance of the anesthetic induction, with good tolerance of the facemask; these results are similar to those reported by other authors.11 However, when patients with a RASS score of +1 (see Tabla 3), which is acceptable for anesthetic induction and tolerability of the facemask, are added in this study, then 92% of patients had good acceptance.
There are several sources of error in our study, including the range of time periods between the administration of the drug and the various assessments, a variable that was impossible to standardize given the particular administrative and healthcare processes of the institution. A second potential source of error is the fact that chemical testing has not found a homogenous concentration of midazolam in the compound prepared at our Hospital; however, the staff is always careful to shake the vial containing the drugs before administering the compound. The third potential source of error is that, although the vast majority of children accepted the mix easily because of its nice flavor, significant amounts of the dose may have been lost during the process of administration, thus affecting the results; however, since there is no quantitative measurement of plasma levels of the medication, there is no way to establish this fact objectively. The fourth source of error is the fact that personality traits were not correlated with the results of the premedication, because the assessment scales have not been validated fully. There was no comparison group because the efficacy of premedication has been clearly demonstrated in the world literature, and we did not think it was ethical to deprive the patients of its benefits, because our main objective was to provide objective proof of the usefulness of an experience based practice. However, if a control group is required, the administration of another drug considered useful as anesthetic premedication, or the use of non-pharmacological measures, may also be considered.
It has been described that acetaminophen may shorten gastric emptying, which could increase the bioavailability of midazolam and shorten the time required to achieve its clinical effect. This may interfere to a certain degree with our results when compared to those of other authors.19The significance of this phenomenon must be assessed in future studies about this topic.
Intravenous midazolam combined with other drugs such as fentanyl and propofol has been used for deep sedation in patients taken to magnetic resonance imaging. Oral midazolam together with acetaminophen might probably be a good and safe option in less complex, non-painful diagnostic tests.20
ConclusionIn the light of the results obtained, premedication with compounded midazolam plus acetaminophen used at the Manizales Children's Hospital is useful: it reduces anxiety at the time when the children are separated from their parents, and it leads to good acceptance of inhaled anesthesia induction, improving the whole experience, both for the children as well as for the parents.
FundingCaldas University, Red Cross Children's Hospital, Manizales, Colombia.
Conflict of interestThe authors have no conflicts of interest to declare.
Acknowledgments
The authors would like to thank Universidad de Caldas, Hospital Infantil de la Cruz Roja de Manizales Staff and Biostatistician Luz Marina Agudelo.
1. Baroncini S, Villani A, Serafini G. Anestesia neonatal y pediátrica. 13.a ed. Elsevier; 2006. p. 21-33. [ Links ]
2. Bailey Jr PD, Bastien JL. Preinduction techniques for pediatric anesthesia. Curr Opin Anaesthesiol. 2005;18:265-9. [ Links ]
3. Rosenbaum A, Kain ZN, Larsson P, Lonnqvist PA, Wolf AR. The place of premedication in pediatric practice. Paediatr Anaesth. 2009;19:817-28. [ Links ]
4. McCann ME, Kain ZN. The management of preoperative anxiety in children: an update. Anesth Analg. 2001;93: 98-105. [ Links ]
5. Singh N, Pandey RK, Saksena AK, Jaiswal JN. A comparative evaluation of oral midazolam with other sedatives as premedication in pediatric dentistry. J Clin Pediatr Dent. 2002;26:161-4. [ Links ]
6. Sheta SA, Alsarheed M. Oral midazolam premedication for children undergoing general anaesthesia for dental care. Int J Pediatr. 2009;2009:274-380. [ Links ]
7. Arevalo J, Duque J. Utilidad del midazolam oral como medicación preoperatoria en el paciente pediátrico. Trabajo de grado. Facultad de Medicina, Universidad de Caldas; 1991. [ Links ]
8. Shrestha S, Shrestha BR. Oral administration of intravenous solution of midazolam mixed in syrup of paracetamol is an effective way of premedicating children undergoing surgery under general anaesthesia. Kathmandu Univ Med J (KUMJ). 2007;5:449-55. [ Links ]
9. Yuen VM, Hui TW, Irwin MG, Yuen MK. A comparison of intranasal dexmedetomidine and oral midazolam for premedication in pediatric anesthesia: a double-blinded randomized controlled trial. Anesth Analg. 2008;106: 1715-21. [ Links ]
10. Rosenbaum A, Kain ZN, Larsson P, Lönnqvist PA, Wolf AR. The place of premedication in pediatric practice. Paediatr Anaesth. 2009;19:817-28. [ Links ]
11. Isik B, Baygin O, Kapci EG, Bodur H. The effects of temperament and behaviour problems on sedation failure in anxious children after midazolam premedication. Eur J Anaesthesiol. 2010;27:336-40. [ Links ]
12. Horgesheimer JJ, Pribble CG, Lugo RA. The effect of midazolam premedication on discharge time in pediatric patients undergoing general anesthesia for dental restorations. Pediatr Dent. 2001;23:491-4. [ Links ]
13. Fortier MA, Del Rosario AM, Martin SR, Kain ZN. Perioperative anxiety in children. PaediatrAnaesth. 2010;20:318-22. [ Links ]
14. Davidson A, McKenzie I. Distress at induction: prevention and consequences. Curr Opin Anaesthesiol. 2011;24:301-6. [ Links ]
15. Bozkurt P. Premedication of the pediatric patient -anesthesia for the uncooperative child. Curr Opin Anaesthesiol. 2007;20:211-5. [ Links ]
16. Vagnoli L, Caprilli S, Messeri A. Parental presence, clowns or sedative premedication to treat preoperative anxiety in children: what could be the most promising option? Paediatr Anaesth. 2010;20:937-43. [ Links ]
17. Kazak Z, Sezer GB, Yilmaz AA, Ates Y. Premedication with oral midazolam with or without parental presence. Eur J Anaesthesiol. 2010;27:347-52. [ Links ]
18. Navas G. ¿Cómo evitar que la inducción anestésica sea recordada como un proceso traumático? En: Anestesiología Pediátrica. Bogotá: Sociedad Colombiana de Anestesia-Scare, Medilegis; 2003. p. 68-79. [ Links ]
19. Oscier CD, Milner QJ. Peri-operative use of paracetamol. Anaesthesia. 2009;64:65-72. [ Links ]
20. Delgado JA, Abad P, Angel GJ, Llano JF, Gomez FJ, Calvo VD. Uso de sedación profunda asistida por un anestesiólogo en resonancia magnética para población pediátrica. Rev Colomb Anestesiol. 2010;38:487-97. [ Links ]











 texto en
texto en