Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Colombian Journal of Anestesiology
Print version ISSN 0120-3347
Rev. colomb. anestesiol. vol.43 no.2 Bogotá Apr./June 2015
Scientific and Technological Research
Association between fibrinogen levels and the severity of postpartum haemorrhage*
Asociacion entre el nivel de fibrinogeno y severidad en la hemorragia posparto
Victoria García Velásqueza,**, Marco González Agudelob, Arturo Cardona Ospinac, Ricardo Ardila Castellanosd
a Specialist in Obstetrics and Gynaecology, Critical Care Medicine and Intensive Care; Specialist at Women's ICU, Clínica del Prado, Medellín, Colombia
b Specialist in Internal Medicine, Critical Care Medicine and Intensive Care, Master in Epidemiology; Coordinator at Women's ICU, Clínica del Prado, Medellín, Colombia
c Specialist in Obstetrics and Gynaecology, Fetal Medicine, Maternal-Fetal Unit Coordinator, Clínica del Prado, Medellín, Colombia
d Specialist in Internal Medicine, Pulmonology, Epidemiology; Fellow in Critical Care Medicine and Intensive Care, UNAB, Colombia
* Please cite this article as: García-Velásquez V, González-Agudelo M, Cardona-Ospina A, Ardila-Castellanos R. Asociacion entre el nivel de fibrinogeno y severidad en la hemorragia posparto. Rev Colomb Anestesiol. 2015;43:136-141.
** Corresponding author at: Departamento de Medicina Crítica y Cuidado Intensivo, Clínica del Prado, Medellín, Colombia. Carrera 50A #64-42 Unidad de Cuidados Intensivos Clínica del Prado.
E-mail address: victoriagarcia1982@hotmail.com (V. García Velásquez).
Article info
Article history: Received 24 April 2014 Accepted 25 December 2014 Available online 5 March 2015
Abstract
Objective: To determine if the level of fibrinogen at the onset of postpartum haemorrhage is associated with bleeding severity and a higher number of complications; to determine outcome-related cut-off points.
Materials and methods: Secondary analysis of a cohort study conducted with 79 mothers admitted to the Intensive Care Unit between February 1st, 2012 and January 31st, 2013, with a diagnosis of postpartum haemorrhage, defined as all cases of blood loss greater than 1000 mL. Fibrinogen levels were measured at the onset of the postpartum haemorrhage. Fibrinogen values were compared between patients with severe obstetric bleeding and those with mild-to-moderate bleeding, in order to establish the correlation with severity of blood loss and complications.
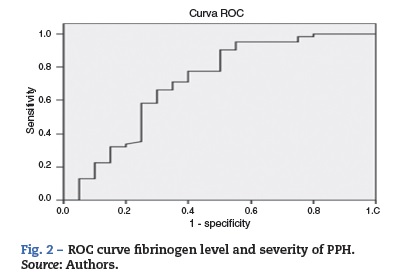
Results: Overall, 24.1% of the patients showed severe postpartum haemorrhage compared to 75.9% of the patients classified as having mild-to-moderate haemorrhage. There were 12 complications (15.2%), including 9 cases of acute renal injury, 2 cases of disseminated intravascular coagulation, and one death, all of them only in patients with severe obstetric haemorrhage. Regarding the initial fibrinogen value, the AUC-ROC for fibrinogen levels and their relationship with the severity was 0.71, with a cut-off point of <200 mg/dL to predict severity (100% positive predictive value).
Conclusion: The initial fibrinogen level in obstetric postpartum haemorrhage is a predictor of severity that helps in alerting to the need for treatment in these patients.
Keywords: Postpartum hemorrhage, Fibrin fibrinogen degradation products, Blood transfusion, Blood coagulation, Maternal mortality.
Resumen
Objetivo: determinar si el nivel de fibrinógeno al inicio de la hemorragia posparto se asocia con la severidad del sangrado y mayor número de complicaciones; además definir los puntos de corte que se relacionan con el desenlace.
Materiales y métodos: análisis secundario de un estudio de cohortes realizado en 79 madres que ingresaron con diagnóstico de hemorragia posparto, definido como todo sangrado mayor de 1000 mL, a la Unidad de Cuidados Intensivos entre el 1 de febrero de 2012 al 31 de enero de 2013. Los niveles de fibrinógeno se realizaron al inicio de la hemorragia posparto. Se comparó el valor de fibrinógeno entre las pacientes que presentaron hemorragia obstétrica severa contra las hemorragias obstétricas leve-moderada, y de esta forma se correlaciona el valor del fibrinógeno con la severidad de la hemorragia y las complicaciones presentadas en las pacientes.
Resultados: el 24,1% de las pacientes presentaron hemorragia posparto severa y se comparó contra el 75,9% de las pacientes clasificadas como leve y moderada. Se presentaron 12 complicaciones (15,2%), 9 fueron injuria renal aguda, 2 coagulación intravascular diseminada y muerte en 1 paciente, sólo en las pacientes con hemorragia obstétrica severa. En cuanto al nivel inicial de fibrinógeno, el AUC-ROC para el valor de fibrinógeno y su relación con severidad fue de 0,71 con un punto de corte < 200 mg/dL para predecir severidad (valor predictivo positivo 100%)
Conclusión: el nivel de fibrinógeno inicial en hemorragia obstétrica posparto es un predictor de severidad que ayuda a alertar el tratamiento en estas pacientes.
Palabras clave: Hemorragia postparto, Productos de degradación de la fibrina-fibrinógeno, Transfusión sanguínea, Coagulación sanguínea, Mortalidad materna.
Introduction
Worldwide, in developed as well as developing countries, obstetric haemorrhage continues to be a significant cause or mortality.1 Postpartum bleeding is the main cause, and atony accounts for 70% of cases and continues to be the main trigger of massive postpartum haemorrhage (PPH) and complications due to coagulopathy.2
The evaluation of postpartum bleeding includes clinical, haemodynamic and laboratory variables used to classify the severity3 and assess patients that benefit from early massive transfusions4 and admission to the intensive care unit, and women at risk of developing complications due to severe haemorrhagic shock. The most important cause of maternal mortality due to postpartum haemorrhage secondary to uterine atony is the inadequate use of transfusion therapy and insufficient intravascular volume replacement,5 as well as inadequate bleeding control in patients that appear clinically "stable". Consequently, early identification of patients that may progress to organ dysfunction and increased risk to their lives is of critical importance.
Procoagulant activity increases two-fold towards the end of pregnancy and, therefore, when postpartum bleeding develops, thrombin and partial thromboplastin times may appear normal, masking patients that are evolving towards early coagulopathy. When fibrinogen values drop to <100 mg/dL they are associated with the loss of 1.4 blood volumes, establishing a relationship between fibrinogen values and the severity of postpartum haemorrhage.6
The objective of this study was to determine whether fibrinogen levels at the onset of postpartum bleeding are associated with the probability of maternal complications, and to define cut-off points related with the outcome.
Materials and methods
Secondary analysis of a cohort study7 with data collected prospectively in an obstetrical Intensive Care Unit in mothers presenting with a diagnosis of postpartum haemorrhage between February 1st, 2012 and January 31st, 2013. Based on the records of that cohort of patients, fibrinogen levels on admission were evaluated and outcomes were correlated with the presence or absence of complications secondary to the haemorrhage upon discharge from the unit. Postpartum haemorrhage was defined as every blood loss greater than 1000 mL following vaginal delivery or caesarean section, estimated by the attendant obstetrician at the time.
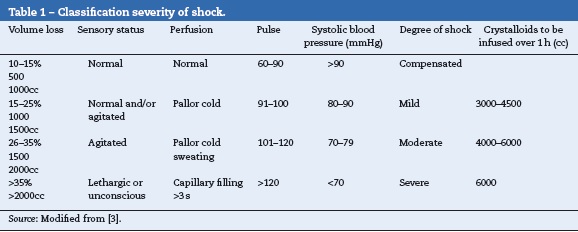
Bleeding severity was defined on the basis of the worst clinical parameter in the haemorrhagic shock classification (Table 1) or an initial estimated blood loss of more than 2000 mL. Mothers with associated diseases such as sepsis, prior liver disease, ketoacidosis and heart disease were excluded, considering that the study was a secondary analysis of a study that assessed lactic acid as a prognostic marker in obstetric haemorrhage and the above disorders may elevate lactic acid levels. Moreover, these disorders are associated with altered coagulation parameters, leading to altered fibrinogen levels not related to the severity of postpartum bleeding.
Fibrinogen levels were measured once, at the onset of postpartum bleeding, in accordance with the protocol used at the Unit for the management of these patients. The initial value was then compared with the gold standard which, in this case, was clinical follow-up upon discharge, and the presence or absence of complications, defined as acute renal injury,8 disseminated intravascular coagulation (DIC),9 death, reintervention for hysterectomy, and adult respiratory distress syndrome (ARDS).10 The endpoint was the presence or absence of complications, not the degree of bleeding severity, which was classified according to the usual clinical standard previously described.
The ROC curve was performed in order to determine the diagnostic accuracy of fibrinogen levels in relation to the presence of complications upon patient discharge from the unit. The area under the curve was estimated in order to assess the accuracy of fibrinogen levels in evaluating the probability of complications in postpartum haemorrhage, and the cut-off point with the highest sensitivity and specificity was determined. A value of p < 0.05 was defined as significant. Version 17 of the SPSS package was used for the statistical analysis.
Considering that the information was collected from records and there was no intervention or modification of patient variables, this study is considered as research with no risk.11 The study followed the ethical principles that apply to human research, stated in the Declaration of Helsinki by the World Medical Association,12 and data collection for the study was approved by the ethics and research committee of the institution.
Results
Data were collected for 79 patients with obstetric postpartum haemorrhage in the initial cohort, with a mean age of 24.6 years; 19 patients (24.1%) developed severe PPH compared with 60 patients (75.9%) who presented with mild and moderate PPH. All patient charts contained the initial fibrinogen value, hence their inclusion in the analysis.
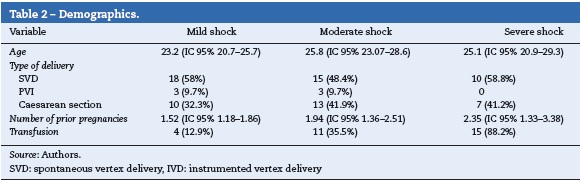
The demographic characteristics are described in Table 2. No significant differences were found between age, number of previous pregnancies or route of delivery in relation to bleeding severity (Table 2).
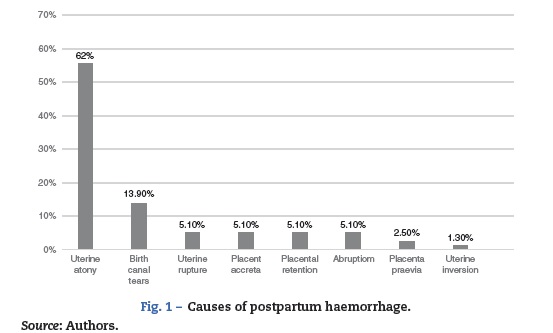
In terms of the causes of postpartum haemorrhage, the majority (62%) were due to uterine atony, followed by cervical or vaginal tear, 13.9%; abruptio placenta, uterine rupture, placenta accreta and placental retention, 5.1% each; placenta praevia, 2.5%; and uterine inversion, 1.3% (Fig. 1). No relationship was found between the cause of the bleeding and its severity.
The main comorbidity was pregnancy-associated hypertensive disorder, found in 21 patients (26.6%); however, no relationship was found with bleeding severity in patients with this comorbidity. There were complications in 12 patients (15.2%), including 9 cases (11.4%) of acute renal injury (all AKIN I), 2 cases (2.5%) of disseminated intravascular coagulation, and 1 death (1.3%).
Resuscitation treatment was similar in all patients, based on haemodynamic targets and perfusion parameters. The use of blood products was based on the judgement of the physician in charge of the unit, with a total of 30 patients (38%) receiving transfusion. Of them, 4 were classified as mild (12.9%), 11 as moderate (35.5%) and 15 as severe (88.2%). Some patients required additional procedures besides pharmacological treatment to control the bleeding (25.4%), including Bakri balloon placement in 7 (8.9%), use of B-Lynch suture in 10 (12.7%) and hysterectomy in 3 (3.8%).
Al patients with fibrinogen levels equal to or lower than 200 mg/dL presented with severe haemorrhage, 12 of them with complications (12/19, 63%), accounting for 100% of all the patients who developed complications. However, 20.5% of patients with fibrinogen levels greater than 200 mg/dL were also classified as severe, but none of them had complications secondary to bleeding. The AUC-ROC for fibrinogen levels and their relationship to complications was 0.71, with a cut-off point ≤200 mg/dL for predicting complications (PPV 100%) and a cut-off point ≥515 mg/dL for predicting absence of complications following postpartum haemorrhage (71% sensitivity, 65% specificity) (Fig. 2).
Discussion
Procoagulant activity increases two-fold towards the end of pregnancy as a way to respond to the need of providing fast and effective haemostasis at the time of placental detachment in order to prevent exsanguination. The main changes observed are increased plasma concentrations of fibrinogen, Factor-VIII and Von Willebrand's factor.13
In cases of severe postpartum haemorrhage requiring massive amounts of infused intravascular volume, dilutional coagulopathy is usually observed with prolonged PTT and PT, and a drop in fibrinogen levels and platelet counts, the majority being late changes. Moreover, there is additional consumption of coagulation factors for thrombus formation at vascular injury sites, with plasma levels - fibrinogen included - dropping below the haemostatic threshold.14
In our study, when initial fibrinogen values dropped below 200 mg/dL there was a correlation with the severity of the postpartum bleeding and the presence of complications, as described by Cortet et al.15 These authors found fibrinogen levels to be an independent factor for postpartum haemorrhage severity, with an OR = 1.90 (95% CI: 1.16-3.09) for a fibrinogen value between 200 and 300 mg/dL, and a better correlation with fibrinogen levels under 200 mg/dL (OR = 11.99; 95% CI: 2.56-56.06).
Along the same lines, Charbit et al.16 showed that a fibrinogen value <200 mg/dL had a 100% PPV for severe PPH. We found that this cut-off point in obstetrics, as well as in the studies mentioned above, is similar to the recommended cut-off point in trauma resuscitation in non-pregnant women, where the association with severity is found in patients with fibrinogen levels below 150-200 mg/dL.17
The use of fibrinogen as a predictor of severe PPH is a reference tool in the identification and classification of severity in this group of patients, given the difficulty for the intensive care physician that has not been present at the onset of postpartum bleeding and may often underestimate the severity of the blood loss. This may result in suboptimal resuscitation, considering that physiological variables undergo late changes in this age group, in otherwise healthy patients with good cardiopulmonary reserve.
Additionally, the finding of a fibrinogen level <200 mg/dL at the onset of postpartum haemorrhage in a patient with hypovolemic shock secondary to severe PPH will facilitate adequate intravascular resuscitation therapy with other blood products besides red blood cells, such as fresh frozen plasma, cryoprecipitate or fibrinogen concentrate, as recommended in current massive transfusion protocols.18-20
The study has some limitations, including the subjective assessment of the initial blood loss by the attendant obstetrician. This is a relevant fact in terms of the initial classification, although it is a recurrent finding in the vast majority of studies in patients with massive bleeding, obstetric or otherwise.
Despite the above, this subjectivity is actually found in daily practice in delivery rooms and intensive care units. In this sense, our study reflects the reality of mothers in our units and underscores the importance of an objective measurement to guide the physician in determining the true severity of the haemorrhage, as is the case with fibrinogen values at the onset of postpartum bleeding.
Conclusion
Fibrinogen levels measured at the onset of bleeding may be used to guide treatment and resuscitation in patients with postpartum haemorrhage. A cut-off point of <200 mg/dL must warn the practitioner about the high risk of severe haemorrhage and complications despite the finding of stable physiological parameters and vital constants, and may be an indication for aggressive transfusion therapy with replacement of coagulation factors, including fibrinogen. In patients with fibrinogen values >200 mg/dL, clinical and physiological variables may continue to be used for severity classification, together with other paraclinical tissue perfusion parameters to help distinguish, early on, patients who will develop complications from those that will not.
Funding
The authors did not receive sponsorship to undertake this article.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Conflict of interest
The authors report no conflict of interest.
References
1. Khan KS, Wojdyla D, Say L, Gulmezoglu AM, Van Look PF. WHO analysis of cases of maternal death: a systematic review. Lancet. 2006;367:1066-74. [ Links ]
2. James AH, McLintock C, Lockhart E. Postpartum hemorrhage: when uterotonics and sutures fail. Am J Hematol. 2012;87:S16-22. [ Links ]
3. Baskett PJ. ABC of major trauma. Management of hypovolaemic shock. BMJ. 1990;300:1453-7. [ Links ]
4. Gutierrez MC, Goodnough LT, Druzin M, Butwick AJ. Postpartum hemorrhage treated with a massive transfusion protocol at a tertiary obstetric center: a retrospective study. Int J Obstet Anesth. 2012;21:230-5. [ Links ]
5. Montufar-Rueda C, Rodriguez L, Jarquin JD, Barboza A, Bustillo MC, Marin F, et al. Severe postpartum hemorrhage from uterine atony: a multicentric study. J Pregnancy. 2013:525914. Epub 2013 Dec 2. [ Links ]
6. Hippala S, Myllyla G, Vahtera E. Hemostatic factors and replacement of major blood loss with plasma-poor red cell concentrates. Anesth Analg. 1995;81:360-5. [ Links ]
7. García-Velásquez V, Rodas-Acosta D, González-Agudelo M, Ardila-Castellanos R. Ácido láctico como marcador pronóstico en hemorragia obstétrica posparto. Med Intens. 2014. Epub ahead of print Feb 01. [ Links ]
8. NICE clinical guideline 169. Acute Kidney Injury. Prevention, detection and management of acute kidney injury up to the point of renal replacement therapy. [accessed 23.08.13]. Available from: http://www.guidance.nice.org.uk/cg169. [ Links ]
9. Levi M, Van der Poll T. Disseminated intravascular coagulation: a review for the internist. Intern Emerg Med. 2013;8:23-32. [ Links ]
10. ARDS Definition Task Force. Acute respiratory distress syndrome. JAMA. 2012;307:2526-33. [ Links ]
11. Resolución 8430 de 1993 del Ministerio de Salud en Reglamentación en Ciencia y Tecnología. Bogotá, DC: Ministerio de Salud, Dirección de desarrollo científico y tecnológico, Republica de Colombia; 1998. [ Links ]
12. World Medical Association. Declaration of Helsinki; 2008 [accessed 2.02.14]. Available from: http://www.wma.net/s/ethicsunit/helsinki.htm. [ Links ]
13. Matsouka C. Haemostatic changes during pregnancy. Haematology. 2005;8 Suppl. 1:S68-71. [ Links ]
14. Hardy J, Moerloose P, Samana M. Massive transfusion and coagulopathy: pathophysiology and implications for clinical management. Can J Anesth. 2004;51:293-310. [ Links ]
15. Cortet M, Deneux-Tharaux C, Dupont C, Colin C, Rudigoz R-C, Bouvier-Colle M-H, et al. Association between fibrinogen level and severity of postpartum haemorrhage: secondary analysis of a prospective trial. Br J Anaesth. 2012;108:984-9. [ Links ]
16. Charbit B, Mandelbrot L, Samain S, Baron G, Haddaoui B, Keita H, et al. The decrease of fibrinogen is an early predictor of the severity of postpartum hemorrhage. J Thromb Haemost. 2007;5:266-73. [ Links ]
17. Spahn D, Cerny V, Coats T, Duranteau J, Fernandez-Mondejar E, Filipescu D, et al. Management of bleeding and coagulopathy following major trauma: an updated European guideline. Critical Care. 2013;17:R76. [ Links ]
18. Onwuemene O, Green D, Keith L. Postpartum hemorrhage management in 2012: predicting the future. Int J Gynecol Obstet. 2012;119:3-5. [ Links ]
19. Buterlow M, Riley E, Druzin M, Fontaine M, Viele M, Goodnough LT. How we treat: management of life-threatening primary postpartum hemorrhage with a standardized massive transfusion protocol. Transfusion (Paris). 2007;47:1564-72. [ Links ]
20. González VH. Transfusión en trauma. Rev Colomb Anestesiol. 2012;40:287-92. [ Links ]











 text in
text in