Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Colombian Journal of Anestesiology
Print version ISSN 0120-3347
Rev. colomb. anestesiol. vol.43 no.3 Bogotá July/Sept. 2015
Case report
Importance of sympathectomy induced by continuous brachial plexus block for digital replantation in a patient with liver cirrhosis: Case report*
Importancia de la simpatectomía inducida por el bloqueo continuo del plexo braquial para la cirugía de reimplante digital en un paciente con cirrosis hepática: reporte de caso
Rosana Guerrero-Domíngueza,**, Daniel López-Herrera-Rodrígueza, Guiomar Fernández-Castelllanob, Francisco Federeroa, Ignacio Jiméneza
a Anesthesiologist and Resuscitation, Hospital Universitario Virgen del Rocío, Sevilla, España
b Resident of Anesthesiology and Resuscitation, Hospital Universitario Virgen del Rocío, Sevilla, España
* Please cite this article as: Guerrero-Domínguez R, López-Herrera-Rodríguez D, Fernández-Castellanos G, Federero F, Jiménez I. Importancia de la simpatectomía inducida por el bloqueo continuo del plexo braquial para la cirugía de reimplante digital en un paciente con cirrosis hepática: reporte de caso. Rev Colomb Anestesiol. 2015;43:250-253.
** Corresponding author at Avenida Ramón Carande, N 11, 4 E, 41013, Sevilla, España.
E-mail address: rosanabixi7@hotmail.com (R. Guerrero-Domínguez).
Article info
Article history: Received 12 January 2014 Accepted 8 March 2015 Available online 5 May 2015
Abstract
Hand microsurgeries are procedures performed by reconstructive surgeons and require a complex and highly individualized approach. The management of anesthesia in patients with cirrhosis may be challenging. Liver dysfunction may condition the extended use of anesthetic agents as a result of a disrupted metabolism and clearance.
This case describes the anesthetic management of a patient with cirrhosis, using a combined anesthetic technique with continuous axillary block of the brachial plexus to prevent postoperative pain and maintain extended vasodilatation. The continuous brachial plexus block under local anesthesia has shown improved tissue perfusion following limb replantation surgery. This technique is particularly helpful to prevent vasospasm in the reconstructed tissue during the postoperative period. In patients with cirrhosis, this technique provides adequate postoperative pain control.
Keywords: Liver cirrhosis, Nerve block, Microsurgery, Brachial Plexus, Anesthesia.
Resumen
Las intervenciones de microcirugia sobre la mano son procedimientos realizados por cirujanos reconstructores que requiere un abordaje complejo y altamente individualizado. El manejo anestésico en pacientes con cirrosis puede ser difícil. La disfunción hepática puede condicionar una duración prolongada de los fármacos anestésicos por un metabolismo e índice de aclaramiento alterados.
Describimos el manejo anestésico de un paciente con cirrosis, empleando una técnica anestésica combinada con bloqueo axilar continuo del plexo braquial para prevenir el dolor posoperatorio y mantener una vasodilatación prolongada. El bloqueo continuo del plexo braquial con anestésicos locales ha mostrado mejorar la perfusión tisular tras la cirugía de reimplante de miembros. Esta técnica es especialmente beneficiosa para prevenir el vasoespasmo en el tejido reconstruido en el periodo posoperatorio. En los pacientes cirróticos, esta técnica ofrece un adecuado control del dolor posoperatorio.
Palabras clave: Cirrosis hepática, Bloqueo nervioso, Microcirugia, Plexo braquial, Anestesia.
Introduction
The continuous brachial plexus block (CBPB) in digital replantation surgery offers numerous advantages in terms of the best graft perfusion1-3. Patients with liver disease are at high risk of perioperative morbidity and mortality due to the effects of surgery and the drugs used, that may further deteriorate the baseline condition leading to liver decompensation4. The metabolism of most opioid drugs is slow5, with a long half-life and increased risk of respiratory depression.
Clinical case
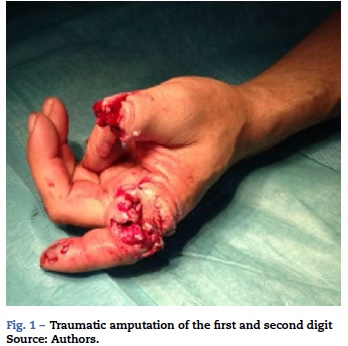
This is a 46 year-old patient with traumatic amputation of the proximal phalanx of the first and second digits (Fig. 1). The personal history highlights liver cirrhosis due to stage A according to the Child-Turcotte-Pugh classification and surgical resection of the liver carcinoma. Following the evaluation of the patient by a multidisciplinary team including plastic surgeons, trauma surgeons and anesthesiologists, the decision was made to do digital replantation. The complementary tests including complete blood count, biochemistry and coagulation tests were all unremarkable.
Upon the usual non-invasive blood pressure monitoring, ECG, pulse oximetry (SpO2), neuromuscular block using the TOF watch SX monitor and placement of an electric blanket, 3mg of midazolam were administered to reduce anxiety. The patient was placed in decubitus supine with the arm abducted at 90° with regard to the trunk. The axillary artery was localized with ultrasound and the medial, ulnar, musculocutaneous and radial nerves were identified, for a needle approach of the plexus plane. The catheter was inserted into the perivascular fascia compartment of the brachial plexus to maintain continuous anesthesia with an initial 0.2% ropivacaine dose of 20 ml. An anesthetic induction then followed with propofol 150 mg, fentanyl 150 and cisatracurium 18 mg and the patient was intubated and connected to mechanical ventilation. 1 CAM sevoflurane and continuous infusion of ropivacaine 0.2% at 6ml/h were used for maintenance of the anesthesia through a nerve catheter. The patient was hemodynamically stable during the intraoperative period of 5h. The first digit was remodeled and the anastomosis of the vascular pedicles was performed, maintaining adequate level of analgesia. At the end of the procedure the patient was extubated and transferred to the postoperative care unit. The patient had a satisfactory evolution during the postoperative period, demonstrating good distal perfusion according to Doppler ultrasound and pulse oximetry of the re-implanted digit. The axillary catheter was kept in place for continuous perfusion of ropivacaine 0.2% at 6 ml/h for 72 h, with adequate analgesia and a visual analog scale (VAS) score < 3; no adjuvant analgesia was needed, no neural lesions were identified and the patient was free of complications.
Discussion
The axillary approach to Brachial Plexus Blockade under local anesthesia is a technique widely used by anesthesiologists6, because of its analgesic efficacy and low risk of complications. It has shown to improve the digital tissue perfusion following replantation microvascular surgery as a result of the sympathetic block and the associated vasodilatation7-10, decreasing the risk of postoperative vasospasm1,2 in areas where the peripheral circulation may be compromised1 with subsequent rise in temperature1.
CBPB provides the best analgesia during the postoperative period as the main indication for this block2,10, and is the ideal analgesic technique for limb replantation surgery9. Because of the few healthcare centers that do this type of surgery, few cases have been described. There are other indications however for CBPB: vascular insufficiency resulting from vasoactive drug therapies, trauma hand injuries, digital amputations, long upper limb surgery, and complex regional pain syndrome1. Regional anesthesia maintains extended and continuous vasodilatation of the operated limb1,2,9,10. Some complications have been described2,11 with regard to the brachial plexus blockade, including infections, hematomas12, retention of catheter fragments, paresthesias, and drug toxicity2,11. The advances in ultrasound have resulted in a lower incidence of neurovascular lesions13 because of the direct visualization of the nerves, the needle, the adjacent structures, and mostly because of the controlled distribution of the local anesthetic agent6.
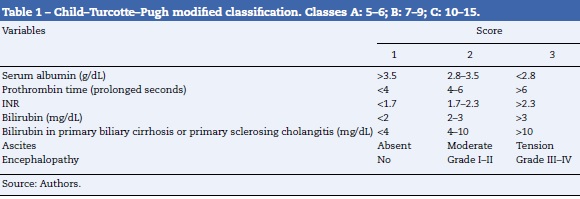
Liver disease poses a high risk of perioperative morbidity and mortality14 because of the effects of surgery and anesthesia on the liver. Various prognostic evaluation scales have been used, such as the Child-Turcotte-Pugh classification (Table 1) or the mathematical model to predict survival of patients with end-stage disease (MELD - Model for End-stage Liver Disease). The model evaluates creatinine and bilirubin levels, the International Normalized Ratio (INR), prothrombin time (PT), and the etiology of liver disease.
Some authors suggest that a patient with a MELD < 10 may undergo elective procedures; a MELD from 10 to 15 indicates that the elective surgery may be done with the potential of surgery-related side effects. A MELD > 15 is indicative of a patient who is a candidate for liver transplant and elective surgery should be avoided15. The case under discussion with A Child classification and MELD > 10, is associated with a moderate anesthetic risk.
Liver cirrhosis presents an increased risk of coagulopathy4,14. The correction of coagulopathy is controversial, since the volume expansion may promote bleeding and raise the portal pressure, resulting in an imbalance of the pro and anti-coagulant factors.4 This approach shall be reserved for active bleeding situations and evidences a deficit in coagulation factors4.
Right ventricle ejection fraction catheter monitoring and trans esophageal echocardiography are recommended4, particularly in intra-abdominal surgery and MELD > 10, as it is considered a high-risk procedure.
The liver is the principal organ responsible for drug metabolism and clearance5. In the presence of liver insufficiency, many drugs may have extended action because of delayed metabolism and reduced clearance rate5,15,16. Benzodiazepines should be carefully dosed since the raise in GABA receptors increases the sensitivity to the drug15. Pain control is critical because the anxiety caused by pain2 during the immediate postoperative period promotes the release of cate-cholamines and vasoconstriction of the re-implanted tissue2.
Based on the pharmacokinetic behavior4, anesthetic agents can be classified into three categories15. Hypnotics like propofol, etomidate, ketamine, morphine or fentanyl4 belong to the group of low protein binding and high liver extraction, with a good safety profile in liver failure and influenced by hepatic flow. The other two groups include those with a low rate of liver extraction that accumulate in cirrhosis (thiopental, diazepam, and methadone)4, and those partially dependent on the liver blood flow with an activity directly related to plasma concentration (midazolam, neuromuscular blockers).4 Both desflurane and sevoflurane maybe safely used for maintaining anesthesia; sevoflurane is associated to lower transaminase elevation during the postoperative period15,16.
Cisatracurium is the best choice for neuromuscular block since it metabolizes through the Hoffman pathway, regardless of the liver impairment.
CBPB reduces the use of opioids and fentanyl provides a good safety profile4,15. Remifentanyl, with a liver-independent metabolism due to plasma stearases, becomes the opioid drug of choice for the intraoperative period15. The use of NSAIDs15 presents some limitations in liver failure because the inhibition of the prostaglandin synthesis has the potential to exacerbate the vasoconstriction of the renal arteries resulting from the presence of vasoconstrictive substances15 (i.e., angiotensin II or noradrenaline).
In summary, a combined anesthetic technique is considered the best anesthetic strategy for digital replantation surgery, where CBPB optimizes distal perfusion and improves the graft survival, preventing the development of vasospasm in the digital arteries of the re-implanted digit17,18. The management of anesthesia in the presence of liver dysfunction involves consideration of drug metabolism, hyper dynamic circulation, perioperative hypoxemia and risk of bleeding14.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Funding
None.
Conflict of interest
The authors declare no conflict of interest.
References
1. Su HH, Lui PW, Yu CL, Liew CS, Lin CH, Lin YT, et al. The effects of continuous axillary brachial plexus block with ropivacaine infusion on skin temperature and survival of crushed fingers after microsurgical replantation. Chang Gung Med J. 2005;28:567-74. [ Links ]
2. Kurt E, Ozturk S, Isik S, Zor F. Continuous brachial plexus blockade for digital replantations and toe-to-hand transfers. Ann Plast Surg. 2005;54:24-7. [ Links ]
3. Taras JS, Behrman MJ. Continuous peripheral nerve block in replantation and revascularization. J Reconstr Microsurg. 1998;14:17-21. [ Links ]
4. Sabaté A, Acosta Villegas F, Dalmau A, Koo M, Sansano Sánchez T, García Palenciano C. Anesthesia in the patient with impaired liver function. Rev Esp Anestesiol Reanim. 2011;58:574-81. [ Links ]
5. Ziser A, Plevak DJ. Morbidity and mortality in cirrhotic patients undergoing anesthesia and surgery. Curr Opin Anaesthesiol. 2001;14:707-11. [ Links ]
6. Berger A, Tizian C, Zenz M. Continuous plexus blockade for improved circulation in microvascular surgery. Ann Plast Surg. 1985;14:16-9. [ Links ]
7. Ilfeld BM. Continuous peripheral nerve blocks: a review of the published evidence. Anesth Analg. 2011;113:904-25. [ Links ]
8. Li J, Karmakar MK, Li X, Kwok WH, Kee WD. Regional hemodynamic changes after an axillary brachial plexus block: a pulsed-wave Doppler ultrasound study. Reg Anesth Pain Med. 2012;37:111-8. [ Links ]
9. Bergman BD, Hebl JR, Kent J, Horlocker TT. Neurologic complications of 405 consecutive continuous axillary catheters. Anesth Analg. 2003;96:247-52. [ Links ]
10. Ekatodramis G, Macaire P, Borgeat A. Prolonged Horner syndrome due to neck hematoma after continuous interscalene block. Anesthesiology. 2001;95:801-3. [ Links ]
11. Vásques MI, Jiménez AM, Aguirre OD, González MP, Ríos AM. Bloqueo supraclavicular bilateral con ecografía. Rev Colomb Anestesiol. 2012;40:304-8. [ Links ]
12. Ortega Romero A, de Diego Isasa D, del Olmo Rodríguez C, Maroto Ramos E, Rouco Gil R. Ecografía portátil en anestesia regional: bloqueos del plexo braquial. Rev Esp Anestesiol Reanim. 2008;55:294-303. [ Links ]
13. Greengrass RA, Feinglass NG, Murray PM, Trigg SD. Continuous regional anesthesia before surgical peripheral sympathectomy in a patient with severe digital necrosis associated with Raynaud's phenomenon and scleroderma. Reg Anesth Pain Med. 2003;28:354-8. [ Links ]
14. Kiamanesh D, Rumley J, Moitra VK. Monitoring and managing hepatic disease in anaesthesia. Br J Anaesth. 2013;111:50-61. [ Links ]
15. Paulino Leal-Villalpando R, Garduño AD. Evaluación y manejo perioperatorio del paciente con cirrosis hepática para cirugía no hepática. Rev Mex Anestesiol. 2008;31:132-8. [ Links ]
16. Hoetzel A, Ryan H, Schmidt R. Anesthetic considerations for the patient with liver disease. Curr Opin Anaesthesiol. 2012;25:340-7. [ Links ]
17. Sorensen J, Bengtsson M, Malmqvist EL, Nilsson G, Sjoberg F. Laser Doppler perfusion imager (LDPI) - for the assessment of skin blood flow changes following sympathetic blocks. Acta Anaesthesiol Scand. 1996;40:1145-8. [ Links ]
18. Breschan C, Kraschl R, Jost R, Marhofer P, Likar R. Axillary brachial plexus block for treatment of severe forearm ischemia after arterial cannulation in an extremely low birth-weight infant. Pediatr Anesth. 2004;14:681-4. [ Links ]











 text in
text in