Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Colombian Journal of Anestesiology
Print version ISSN 0120-3347
Rev. colomb. anestesiol. vol.43 no.4 Bogotá Oct./Dec. 2015
Health education
Ultrasound-guided ankle block: An attractive anaesthetic technique for foot surgery*
Bloqueo de tobillo guiado por ultrasonido: una técnica anestésica atractiva para cirugía de pie
Laura Girón-Arangoa,**, María Isabel Vásquez-Sadderb, María Patricia González-Obregónc, Carlos Enrique Gamero-Fajardoa
a Anaesthesia Resident, Universidad CES, Medellín, Colombia
b Anaesthetist, Clínica CES; Regional Anaesthesia Committee Coordinator, S.C.A.R.E.; Secretary, LASRA International, Medellín, Colombia
c Anaesthetist, Clínica CES; Pain and Palliative Care Specialist, Universidad CES, Medellín, Colombia
* Please cite this article as: Girón-Arango L, Vásquez-Sadder MI, González-Obregón MP, Gamero-Fajardo CE. Bloqueo de tobillo guiado por ultrasonido: una técnica anestésica atractiva para cirugía de pie. Rev Colomb Anestesiol. 2015;43:283-289.
** Corresponding author at: Clínica Universidad CES, Calle 58 N° 50C-2 Prado Centro, Medellín, Colombia.
E-mail address: laura_giron55@hotmail.com (L. Girón-Arango).
Article info
Article history: Received 18 May 2015 Accepted 13 July 2015 Available online 12 August 2015
Abstract
Foot innervation, defined as distal to the tibial and fibular malleoli, is provided by five nerves, namely the tibial, peroneal (deep and superficial), sural and saphenous nerves. Blockade of these nerves is referred to as ankle block. The main advantage of using this block in foot surgery over other regional techniques is the absence of motor blockade above the ankle, which allows faster mobility after surgery. The use of ultrasound for this block has been shown to be of higher clinical efficacy when compared to a landmark approach. The purpose of this continuing education article is not only to detail the anatomy and sonoanatomy of the five nerves innervating the foot, but the ultrasound technique as well. The ultrasound-guided ankle block can be used alone as anaesthetic technique or as adjuvant for analgesia in foot surgery.
Keywords: Anesthesia, conduction, Ultrasonography, Nerve block, Ankle, General surgery.
Resumen
La inervación del pie, definida como aquella distal a los maléolos tibial y peroneal es dada por cinco nervios: tibial, peroneal (superficial y profundo), sural y safeno. El bloqueo de estos nervios se conoce como el bloqueo de tobillo. Su principal ventaja en la cirugía de pie comparado con otras técnicas regionales es la ausencia de bloqueo motor por encima del tobillo, que permite una rápida movilización posterior a la cirugía. El uso del ultrasonido para este bloqueo ha mostrado mayor eficacia clínica cuando se compara con la técnica por reparos anatómicos. El objetivo de este artículo de educación continua no es sólo detallar la anatomía y sonoanatomía de estos cinco nervios sino también describir la técnica guiada por ultrasonido. El bloqueo de tobillo guiado por ultrasonido puede ser usado como una técnica anestésica única o como coadyuvante analgésica en la cirugía de pie.
Palabras clave: Anestesia de conducción, Ultrasonografía, Bloqueo nervioso, Tobillo, Cirugía general.
Introduction
Regional anaesthesia has become increasingly popular in ambulatory surgery because it has been shown to offer excellent pain control in the immediate postoperative period, with shorter length of stay in the post-anaesthetic care unit, and perioperative opioid sparing.1-3
Ankle blockade consists of blocking the five nerves that provide sensory innervation to the region distal to the malleoli. It is used alone as anaesthetic technique in foot surgery provided no pneumatic tourniquet is used during the procedure, or it can also be used together with general or neuroaxial anaesthesia in order to provide adequate post-operative analgesia.4 Whenever a tourniquet is required, we propose its use at ankle level, with good tolerance when the ankle block is used as the only anaesthetic technique.5,6
Its main advantage over the simultaneous sciatic and femoral nerve block is the absence of motor blockade above the ankle. This allows for rapid mobilization of the patient, which is important in the outpatient context or when bilateral procedures are required.7
Migues et al.8 conducted a prospective randomized study in 51 patients, comparing the quality of surgical anaesthesia, postoperative analgesia and postoperative complications of the sciatic nerve block at the popliteal level with the ankle block in foot surgery. In their study, they used the anatomic landmark technique for the ankle block, and the peripheral nerve stimulator for the popliteal sciatic block. The authors did not find a significant difference in terms of block efficacy and the quality of postoperative analgesia. No complications were reported in this study.
Although high rates of success have been reported with the anatomical landmark technique (89-100%),9,10 it has been perceived as technically challenging and not very reliable.11
Regarding the ultrasound technique, Chin et al.12 conducted a six-year retrospective cohort study comparing the ultrasound technique with the anatomical landmark technique for ankle blocks and found that the use of ultrasound increases clinical efficacy with improved surgical anaesthesia, a lower need for rescue systemic opioids, and smaller postoperative opioid doses.
The objective of this article is to review the relevant anatomy and sonoanatomy in ankle blocks and to provide anaesthetists with a tool for localization and successful blockade of the nerves involved.
Ankle innervation
Innervation distal to the malleoli comprises the tibial, superficial and deep peroneal, sural and saphenous nerves.
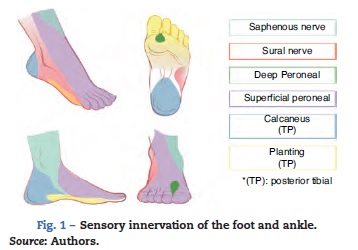
All of these nerves are branches of the sciatic nerve except for the saphenous, which is a branch of the femoral nerve. The deep peroneal, posterior tibial and sural nerves are accompanied by blood vessels, which are useful anatomical landmarks for the ultrasound approach. Fig. 1 shows the regions corresponding to the sensory innervation of each of the nerves of the foot.
Although it has been suggested that saphenous nerve block is only necessary in 3% of patients taken to foot surgery,13 a complete rather than a selective block is recommended regardless of the type of surgery, because nerve territories are often superimposed.4
Tibial nerve: A nerve with mixed characteristics (sensory and motor), it arises from the terminal branches of the sciatic nerve. As it crosses the popliteal fossa it receives the name of tibial nerve, and becomes superficial in the region that lies posterior to the medial malleolus. It is the largest of the group of five nerves innervating the foot and provides sensation to the sole and the heel. At the ankle, it divides into its medial, lateral and calcaneal branches.14,15 With the knee in flexion and the hip in external rotation, the transducer is placed crosswise between the medial malleolus and the Achilles tendon (Fig. 2).
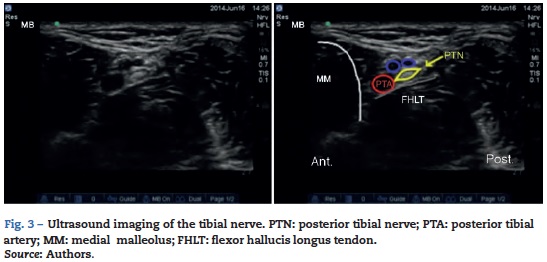
Blood vessels in this area are identified with the help of the sonanatomy, including the posterior tibial artery which runs posterior to the medial malleolus, and two accompanying veins. The tibial nerve appears as a hyperechoic structure adjacent to the posterior tibial artery (Fig. 3).
The tibial nerve is most often found posterior to the artery, although sometimes it may be anterior to it. It is recommended to perform this block proximal to the eminence of the medial malleolus to ensure blockade of the calcaneal branch.16 Finally, it is important to bear in mind the flexor hallucis longus tendon deep to the tibial nerve; because of its sonoanatomic characteristics, it may be mistaken occasionally for a nerve structure.
Redborg et al.15 conducted a prospective randomized study with 18 healthy volunteers comparing the anatomical landmark technique with the ultrasound-guided technique for tibial nerve blockade and showed a higher proportion of complete blocks after 30 minutes when ultrasound was used (72% vs. 22%).
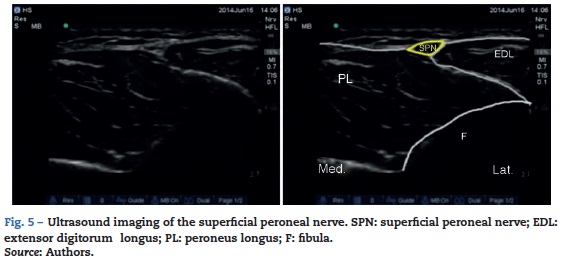
Superficial peroneal nerve: The superficial peroneal nerve is the superficial branch of the common peroneal nerve. It arises at the level of the fibular neck and courses down the lateral compartment of the leg providing sensation to the dorsum of the foot and the toes.17 With the knee in flexion and hip in internal rotation, the transducer is placed across the middle third of the lateral aspect of the leg (Fig. 4).
The anatomical landmark used is the fibula, which generates a rectangular-shaped echo. Superficial to it are the peroneous brevis and extensor digitorum longus muscles. The intermuscular septum and the superficial peroneal nerve are usually visualized at this level between the two muscles, deep to the crural fascia (Fig. 5).
As the transducer is advanced distally, the nerve becomes more superficial until it crosses the crural fascia. At this point, the nerve branches into the intermediate dorsal and medial cutaneous nerves, which innervate the dorsum of the foot.17,18
Regarding the superficial peroneal nerve in particular, no studies were found comparing the success of the ultrasound-guided technique with that of the anatomical landmark technique.
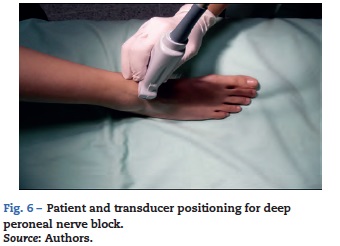
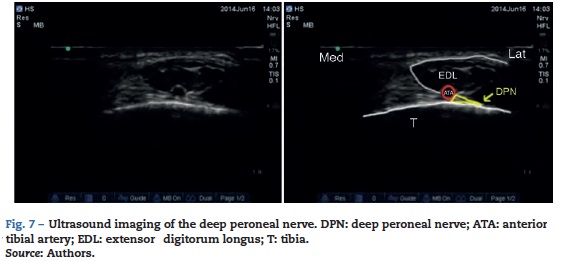
Deep peroneal nerve: The deep peroneal nerve is a branch of the common peroneal nerve and, like the superficial branch, it emerges at the level of the fibular neck. It courses deep to the extensor hallucis longus and becomes more superficial until it comes to the anterior aspect of the interosseous membrane where it is localized lateral to the anterior tibial artery, although anatomical variants have been reported.19,20 It provides sensation to the region between the first and the second rays, the lateral aspect of the first ray, and the medial aspect of the second ray. The transducer is placed cross-wise over the intermalleolar region (Fig. 6), where the anterior tibial artery is visualized as the main anatomical landmark, which is of great use in cases where it is difficult to visualize the nerve because just by surrounding the artery with local anaesthetic the nerve block is assured (Fig. 7).4
Care must be exercised not to press too hard on the transducer because this could occlude the artery and impair adequate visualization.
Antonakakis et al. conducted a prospective randomized controlled study with 18 healthy volunteers comparing the anatomical landmark approach with the ultrasound-guided technique for deep peroneal nerve blockade. At the end of the study, the authors concluded that although the use of ultrasound for deep peroneal nerve blockade reduced latency times, it did not improve the quality of the final block when compared to the conventional anatomical landmark technique.20
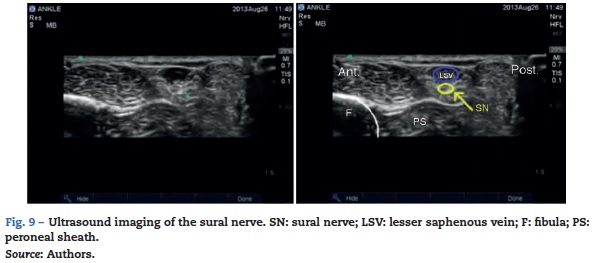
Sural nerve: This nerve arises from branches of the tibial and common peroneal nerves where the gastrocnemii come together in the upper third of the calf. It reaches the ankle in a posterolateral position in contact with the lesser saphenous vein and lateral to the Achilles tendon, branching into two terminal portions referred to a lateral calcaneal and lateral dorsal.14 It provides sensory innervation to the lateral aspect of the heel and to the proximal lateral third of the foot in the majority of cases, and may extend to the lateral aspect of the fifth ray. The patient is positioned with the knee in flexion and the hip in internal rotation, and the transducer is placed across the space between the lateral malleolus and the Achilles tendon (Fig. 8). A hyperechoic image is observed lateral to the lesser saphenous vein along the same subcutaneous plane, but in the event it is not possible to visualize it, localizing the peroneal sheath helps localize the nerve outside and anterior to it (Fig. 9).
Another way to make visualization of the sural nerve easier is by placing a tourniquet in the upper third of the leg in order to provoke distension of the lesser saphenous vein to help with the anatomic localization of the nerve.21 In the event the nerve is not visible, local anaesthetic may be injected around the vein.
Redborg et al.21 conducted a prospective blinded randomized study with 18 healthy volunteers divided into two groups. In one group, ultrasound guidance was used to block the sural nerve, and in the second group they made the blockade under landmark guidance. They concluded that the use of ultrasound results in a more prolonged and complete block.
Saphenous nerve: This is the only nerve arising from the lumbar plexus as it is the terminal branch of the femoral nerve. It courses alongside the greater saphenous vein down to the medial malleolus. It provides sensory innervation to the medial aspect of the ankle and to the heel. There are reports of the saphenous nerve extending deep down to the periostium of the distal tibia, the medial malleolus capsule in the ankle joint and, in some cases, to the capsule of the talocalcaneon-avicular joint medially.22
The patient is positioned with the hip in external rotation and the transducer is placed proximal to the medial malleolus (Fig. 10).
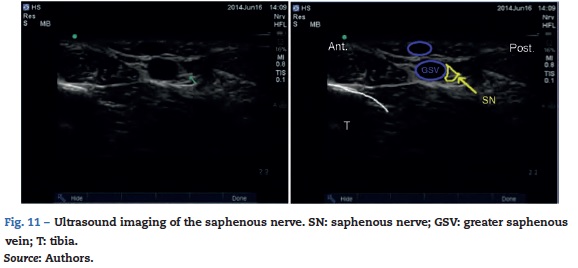
The anatomical landmark is the greater saphenous vein. In the event it is not possible to visualize it, a tourniquet may be placed around the calf in order to promote venous filling. The saphenous nerve may be visualized as a small superficial hyperechoic structure posterior to the greater saphenous vein. However, it is not always visible and the block may require infiltration of local anaesthetic around the vein.23
We did not find studies comparing the use of ultrasound with the anatomical landmark technique for blocking this nerve in particular (Fig. 11).
Ultrasound approach and local anaesthetic volume
The linear transducer is recommended for ankle nerve blocks considering that nerves are superficial, and 50 mm short bevel needles or 25-27G hypodermic needles may be used.
In terms of the approach, both the in-plane or the out-of-plane technique may be used for the five nerves; recommendations regarding the use of one over the other vary in the literature and depend on the authors' own experience.4,7,14
As to the volume of local anaesthetic, it is recommended to use 5 mL for every nerve, except the tibial nerve which requires between 5 and 10 mL because of its larger size. There is general agreement in the literature regarding the use of a total volume ranging between 30 and 40 mL.4'7'12,13 This total volume is not significantly different from the volume used for ankle blocks with the anatomical landmark technique. Fredrickson et al.24 assessed 72 patients taken to foot surgery in whom the ankle block was used. The patients were divided into two groups: in the first group, a low volume of local anaesthetic was used (approximately 16 mL), while the total conventional volume (30 mL) was used in the second group. The authors concluded that, despite a high success rate with the block when low volumes are used, the duration of postoperative analgesia may be compromised.
Conclusions
Ankle blockade is an effective regional anaesthesia technique when used alone or as analgesic adjuvant in foot surgery. In outpatients, it offers the advantage of reduced motor blockade with similar analgesic effectiveness when compared to the sciatic block.8 It may be considered an alternative for patients with heart or pulmonary disease in order to avoid side effects from general anaesthesia and highly potent systemic analgesics such as opioids.5
Although the use of ultrasound to guide the blockade of these five nerves is relatively recent, there are studies in the literature that favour its use over the traditional landmark-guided technique.12,13 Moreover, when the two techniques have been compared in terms of the quality and latency of the blockade for each separate nerve, the literature favours ultrasound for tibial15 and sural21 nerve blocks and does not show any difference in block quality for the deep peroneal nerve.20 No studies were found comparing the two techniques for the superficial peroneal or the saphenous nerves.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Funding
The authors did not receive sponsorship to undertake this article.
Conflict of interest
The authors have no conflicts of interest to declare.
References
1. Collins L, Halwani A, Vaghadia H. Impact of a regional anesthesia analgesia program for outpatient foot surgery. Can J Anaesth. 1999;46:840-5. [ Links ]
2. Chelly JE, Greger J, Casati A, Al-Samsam T, McGarvey W, Clanton T. Continuous lateral sciatic blocks for acute postoperative pain management after major ankle and foot surgery. Foot Ankle Int. 2002;23:749-52. [ Links ]
3. Pearce CJ, Hamilton PD. Current concepts review: regional anesthesia for foot and ankle surgery. Foot Ankle Int. 2010;31:732-9. [ Links ]
4. Peng PWH. Ultrasound for pain medicine intervention: a practical guide. Vol. I: Peripheral structures. Philip Peng education series (electronic book); 2012. [ Links ]
5. Vadivelu N, Kai AM, Maslin B, Kodumudi V, Antony S, Blume P. Role of regional anesthesia in foot and ankle surgery. Foot Ankle Spec. 2015;8:212-9. [ Links ]
6. Purushothaman L, Allan AG, Bedforth N. Ultrasound-guided ankle block. Contin Educ Anaesth Crit Care Pain. 2013;13:174-8. [ Links ]
7. Fredrickson MJ. Ultrasound-guided ankle block. Anaesth Intensive Care. 2009;37:143-4. [ Links ]
8. Migues A, Slullitel G, Vescovo A, Droblas F, Carrasco M, Perrin 17. Turenne H. Peripheral foot blockade versus popliteal fossa nerve block: a prospective randomized trial in 51 patients. J Foot Ankle Surg. 2005;44:354-7. [ Links ]
9. Tryba M. Ankle block: a safe and simple technique for foot surgery. Curr Opin Anaesthesiol. 1997;10:361-5. [ Links ]
10. Lee TH, Wapner KL, Hecht PJ, Hunt PJ. Regional anesthesia in foot and ankle surgery. Orthopedics. 1996;19:577-80. [ Links ]
11. Rudkin GE, Micallef TA. Impediments to the use of ankle block in Australia. Anaesth Intensive Care. 2004;32:368-71. [ Links ]
12. Chin KJ, Wong NWY, Macfarlane AJR, Chan VWS. Ultrasound-guided versus anatomic landmark-guided ankle 21. blocks: a 6-year retrospective review. Reg Anesth Pain Med. 2011;36:611-8. [ Links ]
13. Lopez AM, Sala-Blanch X, Magaldi M, Poggio D, Asuncion J, Franco CD. Ultrasound-guided ankle block for forefoot 22. surgery: the contribution of the saphenous nerve. Reg Anesth Pain Med. 2012;37:554-7. [ Links ]
14. Peer S, Gruber H. Atlas of peripheral nerve ultrasound. Berlin: Springer; 2013. [ Links ]
15. Redborg KE, Antonakakis JG, Beach ML, Chinn CD, Sites BD. Ultrasound improves the success rate of a tibial nerve block at the ankle. Reg Anesth Pain Med. 2009;34:256-60. [ Links ].
16. Lin E, Gaur A, Jones M, Ahmed A. Sonoanatomy for anesthetists. United Kingdom: Cambridge University Press; 2012. [ Links ]
17. Canella C, Demondion X, Guillin R, Boutry N, Peltier J, Cotten A. Anatomic study of the superficial peroneal nerve using sonography. AJR Am J Roentgenol. 2009;193:174-9. [ Links ]
18. Chin KJ. Ultrasound visualization of the superficial peroneal nerve in the mid-calf. Anesthesiology. 2013;118:956-65. [ Links ]
19. Lawrence SJ. The deep peroneal nerve in the foot and ankle: an anatomic study. Foot Ankle Int. 1995;16:724-8. [ Links ]
20. Antonakakis J, Scalzo DC, Jorgenson AS, Figg KK, Ting P, Zuo Z, et al. Ultrasound does not improve the success rate of a deep peroneal nerve block at the ankle. Reg Anesth Pain Med. 2010;35:217-21. [ Links ]
21. Redborg KE, Sites BD, Chinn CD, Gallagher JD, Ball PA, Antonakakis JG, et al. Ultrasound improves the success rate of a sural nerve block at the ankle. Reg Anesth Pain Med. 2009;34:24-8. [ Links ]
22. Chen J, Lesser J, Hadzic A, Resta-Flarer F. The importance of the proximal saphenous nerve block for foot and ankle surgery. Letter to the Editor. Reg Anesth Pain Med. 2013;38: 372. [ Links ]
23. De Mey JC, Deruyck LJ, Cammu G, De Baerdemaeker LE, Mortier EP. A paravenous approach for the saphenous nerve block. Reg Anesth Pain Med. 2001;26:504-50. [ Links ]
24. Fredrickson MJ, White R, Danesh-Clough TK. Low-volume ultrasound-guided nerve block provides inferior postoperative analgesia compared to a higher-volume landmark technique. Reg Anesth Pain Med. 2011;36:393-8. [ Links ]











 text in
text in