Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Colombian Journal of Anestesiology
Print version ISSN 0120-3347
Rev. colomb. anestesiol. vol.44 no.1 Bogotá Jan./Mar. 2016
Scientific and Technological Research
Effect of flumazenil on recovery from general anesthesia with isoflurane: A randomized controlled trial*
El efecto del flumazenil sobre la recuperación de anestesia general con isoflurano: una prueba aleatoria controlada
Domingos Dias Cicarellia,b, Nora Elizabeth Rojas-Álvarezb, Priscila Fullerb, Marcelo Lacava Pagnoccaa,b, Elke Frerichsa, Fábio Ely Martins Bensenora,b
a Department of Anesthesiology, Hospital Universitário, University of São Paulo, Brazil
b Department of Anesthesiology, Hospital das Clinicas, Faculdade de Medicina, University of São Paulo, Brazil
* Please cite this article as: Dias Cicarelli D, Rojas-Álvarez NE, Fuller P, Lacava Pagnocca M, Frerichs E, Martins Benseñor FE. El efecto del flumazenil sobre la recuperación de anestesia general con isoflurano: una prueba aleatoria controlada. Rev Colomb Anestesiol. 2016;44:8-12.
** Corresponding author at: Av. Dr. Enéas de Carvalho Aguiar, n° 155, 8° andar, Prédio dos Ambulatórios, Cerqueira César, São Paulo, SP CEP 05403-000, Brazil.
E-mail address: dcicarelli@uol.com.br (D. Dias Cicarelli).
Article info
Article history: Received 25 April 2014 Accepted 28 May 2015
Abstract
Background and objectives: The inhalational anesthetic isoflurane is widely used in general anesthetics. Its mechanism of action involves interaction with the receptor of gamma-aminobutyric acid (GABA), which is also the binding site for benzodiazepines. Flumazenil, benzodiazepine antagonist, reverses the effects of these drugs in GABA receptors and could therefore also reverse the effect of isoflurane. In anesthesia practice, extubation and early anesthetic recovery reduce morbidity and incidence of complications. The objective of this trial is to determine whether the use of lumazenil may contribute to faster recovery from anesthesia.
Methods: Forty patients scheduled to undergo general anesthesia with isolurane were enrolled in this prospective, double-blind, randomized trial. Patients were randomized to receive, at the end of anesthesia, lumazenil or placebo as allocated into two groups. The anesthetic technique was standardized. The groups were compared concerning values of cerebral state index (CSI), heart rate, blood pressure and oxygen saturation from the application of flumazenil or placebo until 30 min after injection. Data regarding time to extubation, time to reach 10 points in the Aldrete-Kroulic score (AK = 10) and Vigilance score (VS = 10) was also collected. ANOVA test was applied to analyze the results, considering p < 0.05. Results:Patients receiving flumazenil achieved faster extubation than the control (p = 0.033). No differences were observed in values of CSI, the time until AK = 10 and until VS = 10.
Conclusions: Administration of lumazenil at the end of isolurane general anesthesia resulted in earlier extubation in studied patients.
Keywords: Randomized controlled trials as topic, Isoflurane, Flumazenil, Anesthesia general, Receptors, GABA.
Resumen
Introducción y objetivos: El isoflurano es un anestésico inhalatorio ampliamente utilizado en anestesia general. Su mecanismo de acción involucra el receptor del ácido gamma-aminobutírico. Dicho receptor es también el sitio de acción de las benzodiazepinas. El flumazenil, antagonista benzodiazepínico, podría revertir los efectos del isoflurano. En la práctica, la extubación y recuperación anestésica tempranas reducen la morbilidad e incidencia de complicaciones. El objetivo del estudio es determinar la contribución del uso del flumazenil en la recuperación anestésica.
Métodos: Se realizó un estudio doble ciego, prospectivo, aleatorio de 40 pacientes bajo anestesia general con isoflurano que recibieron flumazenil o placebo según aleatorización previa. La técnica anestésica fue estandarizada. Los parámetros comparados en los 2 grupos fueron frecuencia cardiaca, tensión arterial, saturación de oxígeno y niveles del Índice Biespectral, desde la aplicación del flumazenil y durante los 30 minutos posteriores. El tiempo transcurrido entre la inyección del medicamento y la extubación, así como el tiempo requerido para alcanzar 10 puntos en la Escala de Aldrete-Kroulic y la Escala de Vigilancia, también fueron contabilizados. El análisis de la varianza fue aplicado para comparar los datos, considerando p<0.05.
Resultados: Los pacientes que recibieron flumazenil fueron extubados en menor tiempo que los del grupo placebo (P = 0.033). No se observaron diferencias entre los valores del Índice Biespectral y el tiempo necesario para alcanzar 10 puntos en la Escala de Aldrete-Kroulic y la Escala de Vigilancia.
Conclusiones: La administración de flumazenil al final de la anestesia general con isoflurano disminuyó el tiempo a la extubación.
Palabras clave: Ensayos clínicos controlados aleatorios como asunto, Isoflurano, Flumazenil, Anestesia.
Introduction
Volatile anesthetics are widely used in clinical practice of anesthesia.1 Isoflurane is one of most used inhalational anesthetics and one of the safest among currently available. Its mechanism of action, as well as the mechanism of all inhalational anesthetics, is still discussed and researched.2,3 Various experimental studies with isoflurane and also some clinical studies have shown, among other forms of action, their interaction with GABA (gamma-aminobutyric acid) receptor.4-8 This receptor, described some time ago in brain physiology, is the binding site of various anesthetics such as benzodiazepines and barbiturates.
Isoflurane is an inhalational agent with a blood-gas partition coefficient about 1.46, two times greater than sevoflurane approximately. An anesthetic agent with a high blood-gas partition coefficient will diffuse readily into the blood, thus lowering the alveolar partial pressure and causing a slow induction, with a slow recovery too. To appropriately titrate isoflurane during general anesthesia requires a gas analyzer to know exactly the expiratory concentration of isoflurane. Unfortunately the use of gas analyzer is not common in many hospitals at many countries, and sevoflurane remains an inhalational agent very expensive and not routinely used. These two factors contribute to isoflurane be the most commonly used inhalational agent in general anesthesia with a slowly recovery in many times.
Flumazenil is a drug that acts as an antagonist of benzodiazepines, through interaction with GABA-A receptor.9 Thus, it could be used to more quickly reverse the hypnotic effect of isoflurane. The literature shows that the use of flumazenil may be beneficial in reversing anesthesia with sevoflurane, but lacks studies with isoflurane in our knowledge.10-13
The evaluation of depth of general anesthesia can be performed with the use of hemodynamic monitoring (blood pressure, heart rate, etc.) and, more precisely, using level of consciousness monitors, such as cerebral state index (CSI). These monitors process a single frontal electroencephalographic signal to calculate a dimensionless number that provides a measure of the patient's level of consciousness. The values range from 100 to 0, reflecting the awake state and the absence of brain activity, respectively.14,15 Using the data provided by CSI monitors, it is possible to dose the administration of anesthetic drugs based on depth of anesthesia and to evaluate its regression.16
It is known that general anesthesia is not completely free of risks and that early extubation and recovery from anesthesia reduces the incidence of complications and morbidity, as does early discharge from post-anesthetic recovery unit.1 The aim of this study was to determine whether the use of flumazenil may contribute to faster recovery from general anesthesia based on isoflurane, by using cerebral state monitors, hemodynamic and clinical parameters.
Methods
It was conducted a randomized, placebo-controlled, double-blinded clinical experiment involving 40 patients undergoing general balanced anesthesia for minor and midsized surgeries. The sample size was determined to obtain a type 1 error of 5% and a type 2 error of 20%, based on a pilot study.17
Patients were evaluated by an anesthesiologist in pre-anesthetic visit the day before the surgery. Patients included were those aged 18-70, healthy or with minor diseases completely controlled by regular use of medications (ASA I or II according to the classification of physical state by the American Society of Anesthesiologists). Exclusion criteria were: chronic use of benzodiazepines and/or illicit drugs, seizures or panic disorder, or use of premedication.
Immediately before the start of anesthesia, each patient was assigned to one of two groups: P (placebo) or F (flumazenil). The allocation was done by random withdrawal of papers of an envelope containing initially 20 pieces of paper identified as "P" and 20 pieces of paper identified as "F". The withdrawal was conducted by an individual not participating in the anesthetic-surgical procedure and the anesthesiologist remained blinded to this allocation.
All patients underwent general anesthesia as the surgical procedure demands, and were induced with fentanyl 3-10mcg/kg, propofol 3mg/kg and cisatracurium 0.1mg/kg. Anesthesia was maintained with oxygen and air in a 1:1 ratio and isoflurane 1.3 MAC in expired fraction. Patients were followed using a cerebral state monitor (Danmeter A/S, Odense, Denmark) throughout the procedure for maintenance of cerebral state index (CSI) between 40 and 60 (surgical anesthesia). After the end of the surgery, analgesic and antiemetic medications were administered according to the routine of the service (ondansetron, dipyrone and ketoprofen) if patients were not allergic and medications were not contraindicated.
At the end of surgery, patients received the intravenous (IV) solution according to which group they had been allocated in: P group received 20 mL of saline and F group received 1 mg of flumazenil (diluted to 20 mL in saline), both administered by intravenous single and slow injection (during 1 min) right after ceasing isoflurane administration. The anesthesiologist in charge was unaware of the injected solution.
After drug administration, the anesthesiologist recorded the following data: time from injection of medication to extubation; time to reach Aldrete-Kroulic 10 (AK = 10) at the post-anesthesia recovery room; time to reach the Vigilance score 10 (VS = 10)17 at the PAR; CSI values, heart rate (HR), blood pressure (BP) and oxygen saturation at the following times: immediately before injection (T0), then 1 in 1 min until the 5th minute (T1, T2, T3, T4 and T5), at the 10th, 15th, 20th and 30th minutes (T10, T15, T20 and T30).
Groups were compared for the various values of CSI, heart rate, blood pressure and oxygen saturation, and also for time to extubation, time to AK = 10 and to VS = 10, by ANOVA test, considering p <0.05. Extubation was performed by clinical criteria, and performed by the same anesthesiologist, blinded to the group to which the patient had been allocated.
Patients were observed for the incidence of possible side effects (agitation, anxiety, seizures), although these rarely appear in patients without a history of chronic use of ben-zodiazepines, panic disorder or epilepsy.
This trial was approved by the Research Ethics Committee of the University Hospital of the University of São Paulo (CEP-HU/USP) under the protocol number CEP-HU/USP 984/10, and by the National Research Ethics (SISNEP) under the CAAE (Certificate Presentation to Ethical Consideration) 0011.0.198.000-10. The trial was performed entirely in the University Hospital of USP from January 2011 to February 2012. After being invited to join the study and being informed about the same, all participants signed an informed consent form. Retrospective registration at Clinical Trials: NCT02157428.
Results
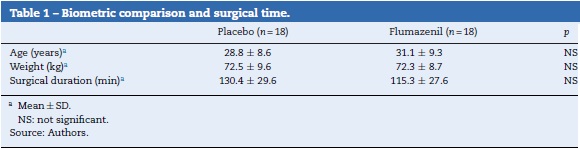
Of the 40 patients initially included in the study, 4 were excluded, 2 due to cancellation of surgery and two due to withdraw of the consent at the time before the start of anesthesia. The other 36 remained at the study until the end (discharge from post-anesthesia recovery room) and their data were analyzed. There was no difference between the two groups concerning age, weight and duration of surgery (Table 1)
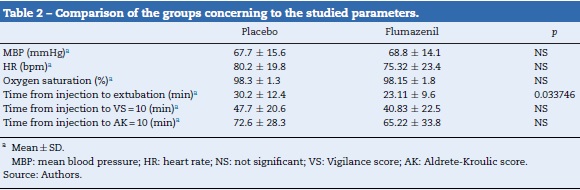
The flumazenil group presented time from injection to extubation significantly lower than the placebo group (P = 0.034). No differences were observed concerning time to reach AK = 10 or to achieve VS = 10. The mean arterial blood pressure, heart rate and saturation were also similar between the two groups (Table 2).
No patient showed signs of side effects of flumazenil (seizures, agitation, anxiety).
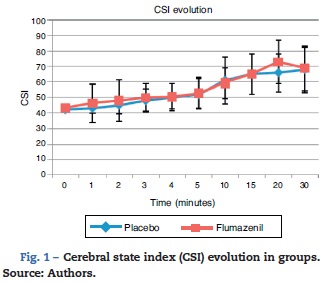
The change in the CSI values from injection until 30 min after (T0-T30) is shown in Fig. 1. Patients who were referred to the recovery room failed to be monitored by CSI. Thus, until T10, all patients (36) were still being monitored. Starting from T15, there was a decrease in the number of monitored patients: 17 (group P) and 17 (group F). At T20, the numbers dropped to 14 (P) and 13 (F) and, at T30, to 11 (P) and 8 (F).
The mean values of the CSI in group P (54.00) and group F (55.66) showed no statistical difference.
Discussion
The use of flumazenil at the end of surgery was effective in reducing the time to extubation of patients undergoing general anesthesia with isoflurane. This observation had never been found previously in literature and is in agreement with the mechanism of action of isoflurane suggested by the literature: activation of GABA-A receptors, similar to what occurs with the use of benzodiazepines.4,5,18
Other authors have shown that GABA receptors may also have a role in the hypnosis caused sevoflurane and that flumazenil provided earlier regression of general anesthesia with sevoflurane.10-13
The lack of difference in the CSI may be due to a bias in the evaluation, since an increasing trend is visible in T20 in the F group larger than the group P. This trend is not confirmed at T30, which may be due to the small number of total patients evaluated in T30 (n = 19), and a smaller number of patients in P group (n = 8) than in F group (n = 11). These excluded patients, who had already gone to the recovery room, would probably have a higher CSI. Furthermore, studies with larger number of patients could find a difference concerning time to reach AK = 10.
The extubation criteria used in our study were clinical. In an attempt to minimize variations of conduct, the same anesthesiologist was responsible for all anesthetic procedures performed.
In this study, we tried to work with patients who were not affected by serious diseases and who had no clinical complications, so that the sample was more homogeneous and interference of comorbidities at the time of regression of anesthesia and at other clinical and hemodynamic parameters studied was minimized. The effect of flumazenil at extubation of patients with more severe and/or poorly controlled illnesses and life-threatening diseases cannot be analyzed based only on the results here obtained. Studies involving ASA III and IV patients may be needed to verify the effect of flumazenil in isoflurane general anesthesia in such patients.
The absence of other medications with known action in reversing the hypnotic effect of isoflurane highlights flumazenil as a potential drug for clinical use for this purpose. The low incidence of side effects in patients without previous use of benzodiazepines and without epilepsy ensures safe use of flumazenil for these individuals. Studies with a larger sample may be required to further evaluate the feasibility and safety of large-scale use of flumazenil at the end of anesthesia with isoflurane.
In conclusion, this study shows that the use of flumazenil in general anesthesia with isoflurane was beneficial in accelerating extubation.
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Funding
The authors did not receive sponsorship to undertake this article.
Conflicts of interest
The authors have no conflicts of interest to declare.
References
1. Gempeler FE, Avellaneda MV. Evaluation of patient satisfaction and recovery time following different anesthetic techniques at the San Ignacio University Hospital. Rev Colomb Anestesiol. 2010;38:178-202. [ Links ]
2. Brown EN, Lydic R, Schiff ND. General anesthesia, sleep and coma. N Engl J Med. 2010;363:2638-50. [ Links ]
3. Vazey EM, Aston-Jones G. Designer receptor manipulations reveal a role of the locus coeruleus noradrenergic system in isoflurane general anesthesia. Proc Natl Acad Sci USA. 2014;111:3859-64. [ Links ]
4. Morgan GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. 3rd ed. New York: Lange-McGraw-Hill; 2002. p. 127-50. [ Links ]
5. Ebert TJ, Schinid PG. Inhalational anesthesia. In: Barash PG, editor. Clinical Anesthesia 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2001. p. 377-417. [ Links ]
6. Weinbroum AA, Geller E. Flumazenil improves cognitive and neuromotor emergence and attenuates shivering after halothane, enflurane and isoflurane based anesthesia. Can J Anesth. 2001;48:963-72. [ Links ]
7. Gyulai FE, Mintun MA, Firestone LL. Dose-dependent enhancement of in vivo GABAa-benzodiazepine receptor binding by isoflurane. Anesthesiology. 2001;95:585-93. [ Links ]
8. Salmi E, Kaisti KK, Metsáhonkala L, Oikonen V, Aalto S, Nâgren K, et al. Sevoflurane and propofol increase 11C-flumazenil binding to gamma-aminobutyric acidA receptors in humans. Anesth Analg. 2004;99:1420-6. [ Links ]
9. Rodnick ME, Hockley BG, Sherman P, Quesada C, Battle MR, Jackson A, et al. Novel fluorine-18 PET radiotracers based on flumazenil for GABAA imaging in the brain. Nucl Med Biol. 2013;40:901-5. [ Links ]
10. Kim YJ, Lee H, Kim CH, Lee GY, Baik HJ, Han JI. Effect of flumazenil on recovery from anesthesia and the bispectral index after sevoflurane/fentanyl general anesthesia in unpremeditated patients. Korean J Anesthesiol. 2012;62:19-23. [ Links ]
11. Liang P, Zhou C, Li KY, Guo LJ, Liu B, Liu J. Effect of flumazenil on sevoflurane requirements for minimum alveolar anesthetic concentration-awake and recovery status. Int J Clin Exp Med. 2014;7:673-9. [ Links ]
12. Dahaba AA, Bornemann H, Rehak PH, Wang G, Wu XM, Metzler H. Effect of flumazenil on bispectral index monitoring in unpremedicated patients. Anesthesiology. 2009;110:1036-40. [ Links ]
13. Karakosta A, Andreotti B, Chapsa C, Pouliou A, Anastasiou E. Flumazenil expedites recovery from sevoflurane/remifentanil anaesthesia when administered to healthy unpremedicated patients. Eur J Anaesthesiol. 2010;27:955-9. [ Links ]
14. Anderson RE, Barr G, Jakobsson JG. Cerebral state index during anaesthetic induction: a comparative study with propofol or nitrous oxide. Acta Anaesthesiol Scand. 2005;49:750-3. [ Links ]
15. Avidan MS, Zhang L, Burnside BA, Finkel KJ, Searleman AC, Selvidge JA, et al. Anesthesia awareness and the bispectral index. N Engl J Med. 2008;358:1097-108. [ Links ]
16. Recart A, Gasanova I, White PF, Thomas T, Ogunnaike B, Hamz M, et al. The effect of cerebral monitoring on recovery after general anesthesia: a comparison of the auditory evoked potential and bispectral index devices with standard clinical practice. Anesth Analg. 2003;97:1667-74. [ Links ]
17. Hulley SB, Commings SR. Designing Clinical Research: An Epidemiologic Approach. Baltimore: Williams & Wilkins; 1988. p. 215 [Appendix 13A] [ Links ].
18. Geller E, Weinbrum A, Schiff B, Speiser Z, Nero Y, Halpern P, et al. The effect of flumazenil on the process of recovery from halothane anaesthesia. Eur J Anaesthesiol. 1988;Suppl2:151-3. [ Links ]