Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Colombian Journal of Anestesiology
Print version ISSN 0120-3347
Rev. colomb. anestesiol. vol.44 no.2 Bogotá Apr./June 2016
Scientific and Technological Research
Design and performance evaluation of the "iTIVA" algorithm for manual infusion of intravenous anesthetics based on effect-site target*
Diseño y evaluación del desempeño del algoritmo "iTIVA" para la administración manual de anestesicos intravenosos según objetivo en sitio efecto
David Eduardo Ramíreza,**, José Andrés Calvacheb
a MD, Department of Anesthesiology, Universidad del Valle, Cali, Colombia
b MD, MSc, F1PP, Department of Anesthesiology, Universidad del Cauca, Popayan, Colombia. Anesthesiology & Biostatistics Department, Erasmus University Medical Centre Rotterdam, The Netherlands
* Please cite this article as: Ramírez DE, Calvache JA. Diseño y evaluacion del desempeño del algoritmo "iTIVA" para la administración manual de anestesicos intravenosos según objetivo en sitio efecto. Rev Colomb Anestesiol. 2016;44:105-113.
** Corresponding author at: Departamento de Anestesiología, Universidad del Valle, Edificio 112, Hospital Universitario del Valle, piso 4, Cali, Colombia.
E-mail address: eramirez3@gmail.com (D.E. Ramírez).
Article history: Received 23 January 2015 Accepted 2 February 2016 Available online 17 March 2016
Abstract
Introduction: Remifentanil and propofol infusion using TCI pumps has proven to be beneficial for the practice of anesthesia but the availability of these systems is limited.
Objective: Designing a pharmacokinetic model-based algorithm for calculating manual infusion regimens to achieve plasma and effect-site concentrations that may be used in volume infusion pumps, and to compare the difference between the desired and the predicted concentrations via pharmacokinetic simulation.
Methods: Using the Minto & Schnider models for remifentanil and propofol respectively, the algorithm was implemented on an iTIVA application (interactive TIVA) for iOS and Android operating systems. The performance of the algorithm was evaluated estimating the infusion regimens for achieving different effect-site concentrations for induction and maintenance in 34 theoretical patients for 240 min.
Results: The infusion regimens obtained for remifentanil and propofol resulted in less than 5% average systemic deviation versus the target effect-site concentrations during induction and maintenance. Only one induction infusion was required for remifentanil and propofol. Just one infusion rate was required for remifentanil during maintenance, and between 2 and 5 infusion rate changes for propofol to maintain a stable concentration. The iTIVA-based algorithm estimates concentrations similar to the TivaTrainer® software.
Conclusions: The performance of the algorithm to achieve effect-site concentrations during induction and maintenance for remifentanil and propofol was excellent, with a low systemic deviation versus the desired target concentrations.
Keywords: Propofol, Pharmacokinetics, Anesthesia, Computer simulation, Infusion pumps.
Resumen
Introducción: La administración de remifentanil y propofol con el uso de perfusores TCI ha mostrado beneficios en la practica anestésica, sin embargo, su disponibilidad es limitada.
Objetivo: Basados en modelos farmacocineticos, diseñar un algoritmo capaz de calcular esquemas de infusión manual para alcanzar concentraciones en plasma y sitio efecto que puedan ser utilizados en bombas de infusión volumétricas. Adicionalmente, comparar la diferencia entre concentraciones deseadas y predichas mediante simulación farmacocinética.
Métodos: Siguiendo modelos de Minto y Schnider para remifentanil y propofol respectivamente, el algoritmo se implementó en una aplicación llamada iTIVA (interactive TIVA) para los sistemas operativos iOS y Android. El desempeño del algoritmo se evaluó calculando esquemas de infusión para obtener distintas concentraciones en sitio efecto en la inducción y mantenimiento en 34 pacientes teóricos durante 240 minutos.
Resultados: Los esquemas de infusión obtenidos para remifentanil y propofol presentaron un desviación sistemática promedio menor al 5% respecto a las concentraciones en sitio efecto objetivo en la inducción y mantenimiento. En la inducción una única infusión fue requerida para el remifentanil y propofol. Durante el mantenimiento una única tasa de infusión fue requerida para el remifentanil y entre 2 y 5 cambios de tasa de infusión para el propofol para mantener una concentración estable. El algoritmo implementado en iTIVA calcula concentraciones similares que el software TivaTrainer®.
Conclusiones: El desempeño del algoritmo para alcanzar concentraciones en sitio efecto durante la inducción y mantenimiento para remifentanil y propofol fue excelente con una desviación sistemática baja con respecto a las concentraciones objetivo deseadas.
Palabras clave: Propofol, Farmacocinética, Anestesia, Simulación por computador, Bombas de infusión.
Introduction
The current practice in anesthesiology is the administration of intravenous agents using standard doses that are empirically adjusted. Such approximation fails to consider the interindividual variability of pharmacokinetics, and the variable dose-plasma concentration relationship that sometimes leads to adverse events.1
Mathematical models have been developed in the last two decades based on studying the plasma concentrations of various drugs. These models describe the process of drug distribution and clearance so as to predict the effect of administering multiple boluses, intravenous infusions, or a combination of both. The use of these models facilitates the teaching and learning process of pharmacokinetics applied to anesthesia.2,3
Computer technology has enabled the adoption of theoretical models for the pharmacokinetic simulation of drugs like propofol (Schnider's model)4 and remifentanil (Minto's model).5 These systems allow for controlling the infusions by adjusting to specific target concentrations of the particular drug.6-9 This technology is commonly referred to as TCI (Target control infusion) and has facilitated the administration of intravenous drugs including remifentanil and propofol, allowing for rapid titration to achieve different therapeutic goals with enhanced hemodynamic stability.3,10
TCI pumps are not widely available in our daily practice and few hospitals actually have the devices so the use of total intravenous anesthesia is limited. However, even in countries where the TCI technology is widely available, only 15-40% use this approach for TIVA11-13; furthermore, restrictions to access in the United States or economic limitations as in most developing countries,14,15 are an obstacle to its wide dissemination and use. Thus, the manual administration of anesthetic agents with volume infusion pumps (VIP) is a current practice.
Passive TCI systems have been developed for a realtime pharmacokinetic simulation of the drugs administered, which have proven to achieve stable plasma and effect-site concentrations, reducing the mental effort for the anesthetist.16-18 These systems are only available for some anesthesia machines (for example, Navigator Applications Suite-GE Healthcare and SmartPilot View-Drager Medical), demand careful titration, but do not suggest an infusion rate so that the anesthetist achieves the desired concentration.19
In contrast to the passive TCI systems, the TCI pumps are able to achieve plasma and effect-site concentrations swiftly and accurately, using complex infusion regimens that change every 10 s under the control of a microprocessor based on a pharmacokinetic model that maintains stable concentrations throughout.20 It is currently impossible to mimic the performance of TCI pumps with a manual approach, due to the mathematical complexity and narrow variation of infusion rates.
Using the models described by Minto5 and Schnider4 for remifentanil and propofol respectively, it is possible to achieve and maintain plasma and effect-site concentrations using a mathematical algorithm that allows for minor and tolerable variations of such concentrations. According to this hypothesis, the purpose of this study was to design an algorithm able to calculate manual infusion regimens to reach plasma and effect-site concentrations, and to contrast the difference between the desired concentrations and the concentrations predicted using pharmacokinetic simulation.
Methodology
This study was divided into two phases: first the technical information about the pharmacokinetic performance of intravenous anesthetic agents that was used to develop an algorithm to simulate plasma and effect-site concentrations, and to calculate infusion systems to accomplish specific plasma and effect-site concentrations. This algorithm was implemented on a mobile application called "iTIVA" (interactive TIVA), for the iOS and android operating systems.
The second phase used the simulation of the infusion regimens calculated based on the algorithm developed as an evaluation method, as previously described in other papers.21
Developing the algorithm
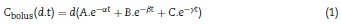
Most intravenous anesthesia models including remifentanil and propofol are based on three-compartment models,2,3 described in equation 1, that predicts the plasma concentration following a "d" bolus over time "t"21:
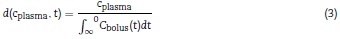
The plasma concentration of a continuous infusion at a "d" dose equals the infinitesimal repetition of "di" boluses equivalent to "d" over time "t", as described by the integral of Eq. (1):
By clearing "d" from Eq. (2), a "d" infusion dose is obtained to achieve a plasma concentration over time "t".
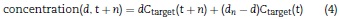
When the infusions vary over time, the difference between the new infusion dn" over time "t + n" is added to the first infusion as described in Eq. (4):
The effect-site concentrations are obtained from the plasma concentrations through a non-analytical solution described in the codes section under http://www.opentci.org/.
Eq. (3) gives a "d" infusion rate to achieve "Cp" plasma concentrations over time "t" and based on that "d" infusion rate, "d" is iteratively increased by 0.1 until dose "d" is obtained to achieve the target effect-site concentration.
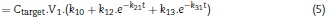
The next step is to calculate a maintenance infusion to offset the distribution and clearance losses for maintaining a pseudo-stable condition for a desired concentration. So Eq. (5) calculates a "d" infusion rate over time "t", to make up for the distribution and clearance losses and is maintained over a "t + n" time, until the simulated plasma concentration exceeds the target concentration "C" + 0.1. At this point, using Eq. (5) the new maintenance infusion is recalculated over a time "t + n" and this goes on successively for as long as we want to maintain the concentration.
Mintenanceinfusion (Ctarget,t)
During maintenance there is no difference if the target is plasma or effect-site since both compartments tend to rapidly balance out during this stage of the process.
Performance of the algorithm
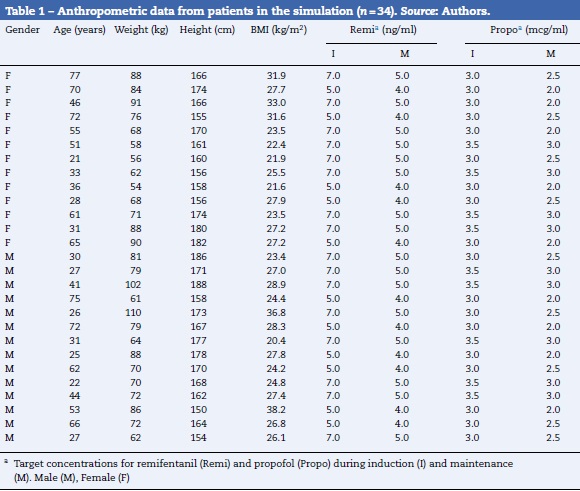
The data from 34 theoretical patients was used to evaluate iTIVA's performance in obtaining effect-site concentrations based on a manual infusion regimen. This was the basis to calculate infusion regimens for 240 min in order to achieve different effect-site concentrations, randomly assigned for remifentanil and propofol. The data used are shown in Table 1.
The data were tabulated using Microsoft Excel 2011 (Redmond, WA, USA) and exported to the statistical package R for analysis and plotting.22 The measurements and standard deviations of the simulated concentrations were calculated for each minute and the date were pooled based on the target site-effect concentrations.
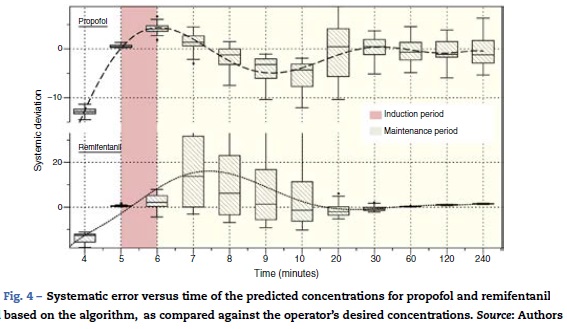
To accurately evaluate the iTIVA concentrations anticipated, the predictive error, the predictive error rate, and the systematic error (bias) were estimated versus the desired concentration (Table 2). This methodology was previously described by Lerou.23 These results are presented on a graph using summary statistics and scatterplots. The performance of the algorithm was independently analyzed to accomplish target concentrations during induction and maintenance. By definition, induction was considered as the period of time between minute 5 and minute 6, and maintenance as the period of time between minute 7 and the end of the simulation (minute 240).
Finally, the concentrations obtained in plasma and site-effect using iTIVA were compared against the concentrations estimated using TivaTrainer® software (version 8; European Society for Intravenous Anaesthesia, Glasgow, UK) (Table 3). In view of the post-hoc results, no hypotheses comparisons were done.
Results
The algorithm was successfully implemented in both iOS and Android applications that are available at no cost from App-Store and Google Play. Fig. 1 shows the App screens for iPhone, including uploading of anthropometric data, target concentrations, the calculated infusion regimen and the graphical representation of the pharmacokinetic pharmacodynamic24 behavior as time progresses.
In order to maintain a stable concentration during induction, a single infusion rate for remifentanil and propofol was required. However, to maintain a stable concentration throughout the 235 min of maintenance, a single infusion rate for remifentanil was required, and between 2 and 5 changes in the infusion rate for propofol (mode = 4).
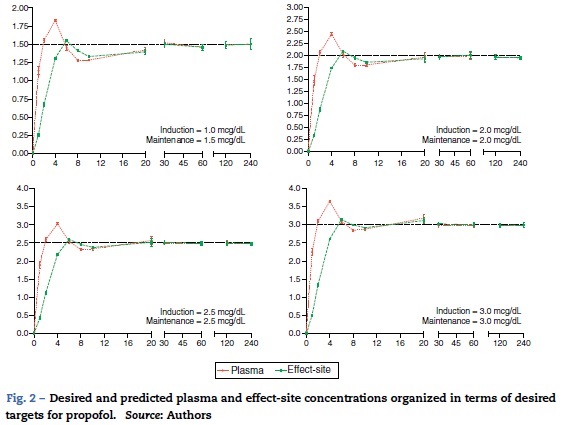
The desired and predicted plasma and effect-site concentrations obtained from the simulation and organized according to the desired targets for propofol and remifentanil are shown in Figs. 2 and 3, respectively. The time axis (X axis) emphasize the initial few minutes corresponding to the induction of anesthesia.
Fig. 4 illustrates the systematic error versus time of the predicted concentrations for propofol and remifentanil according to the algorithm, against the operator-desired concentrations.
Plasma and effect-site concentrations and their variability when simulating different infusion regimens using the algorithm implemented with iTIVA versus the concentrations estimated using the TivaTrainer® software were similar for different evaluation time points (Table 3).
Discussion
The primary results from this study are: (1) the algorithm described was successfully implemented; (2) the performance of the proposed algorithm to reach effect-site concentrations during induction and maintenance for remifentanil and propofol was excellent; (3) the algorithm has a tolerable variability regarding the desired concentrations and such variability decreases during the maintenance period; and (4) the iTIVA implemented algorithm to simulate plasma and effect-site concentrations according to an infusion regimen behaves similarly to the TivaTrainer® software.
Algorithm development and implementation
The algorithm developed was smoothly implemented assisted by Apple and Google development tools for their iOS (Xcode) and Android (Eclipse) systems, respectively. Initially the algorithm was implemented for Android because it has fewer limitations for publication in the Android App store (this fact facilitated the debugging of the programming code). Then it was adapted to the iOS operating system making use of the similar syntax of both programming languages (Java and C++).
For optimal performance (during 240 min of simulation) this algorithm the algorithm requires from 200,000 to 250,000 mathematical calculations but nowadays this is not a major limitation for the microprocessors available even inside the simplest mobile devices.
Algorithm performance and variability
During the induction of anesthesia (minute 5 and 6) the systematic error of the desired concentrations of the two drugs was <5%. Such low variability translates into a very small difference between the desired concentration and the concentration achieved with the algorithm.
During maintenance (minute 7-240), the infusion regimens showed changes in the systematic error that was less than 5% overall for propofol and 15% for remifentanil. Such variability drops significantly at 20 min for remifentanil and at 30 min for propofol. The divergence observed in the first few minutes may be related to the change from one larger target concentration to a smaller one. During this time - and to maintain a stable concentration with less than 5% variation - a single infusion rate was required for remifentanil and from 2 to 5 progressive changes in the infusion rate for propofol. This difference may be accounted for by the pharmacokinetic characteristics of remifentanil that makes it unresponsive to the environment.25
In contrast to the infusion regimens used in TCI pumps that require approximately 1400 changes in the infusion rate over 240 min, this algorithm provides simple, easy to implement regimens with VIP. It delivers very accurate information to achieve and maintain the desired effect-site concentrations, with one advantage versus the standard-dose based administration of medications. Several authors26-31 have reported these concentrations (based on therapeutic targets).
It should be stressed however, that the inter-individual variation and the large number of variables affecting the phar-macokinetics and pharmacodynamics of drugs hinder most pharmacological simulation processes. This fact curtails the accuracy of the pharmacokinetic models as well as the performance of this and several other algorithms. It is then essential to evaluate any individual effects. There are various types of systems available to measure the depth of anesthesia and using these systems in the right context may improve certain outcomes for the patient and lower the risk of adverse events such as intraoperative awareness.32
This research project does not validate a pharmacological forecast versus an actual blood concentration measurement. We chose Lerou's et al.,23 strategy now used by other authors, to simply compare our mathematical forecast as estimated with the algorithm, versus an operator-desired concentration. In the future, tt would be interesting to take a direct measurement of blood concentrations and to contrast those values against the forecasts of the proposed model.
Simulation of concentrations: iTIVA versus TivaTrainer®
The iTIVA algorithm gives plasma and effect-site concentrations of the estimated regimens in real time (in accordance with Eqs. (1) & (2)). The concentrations obtained using iTIVA are identical to those obtained with TivaTrainer/® This latter software is widely used for pharmacological research and simulation.2 This was an expected finding since both applications are based on the same mathematical algorithm and confirms its proper implementation in iTIVA.
Conclusion
Using pharmacokinetic models, the iTIVA App quantifies the infusion rates required to manually achieve effect-site concentrations for remifentanil and propofol and this facilitates its use in VIPs. Currently this application is just designed to guide the administration of manual infusions. It is not approved for use as a single strategy for managing patients and its use should be the anesthetist's responsibility. This article presents a theoretical approach based on a simulation process and its widespread use in clinical practice should be subject to a process of validation and comparison against other infusion regimens.33
Disclosures
There are no conflicts of interest.
Funding
This paper was sponsored by the Colombian Society of Anesthesiology and Resuscitation - SCARE.
Conflicts of interest
The authors have no conflicts of interest to declare.
References
1. Durieux ME. Anesthetic neurotoxicity: it's not just for children anymore. Anesth Analg. 2010;110:291-2. [ Links ]
2. Struys MM, De Smet T, Mortier EP. Simulated drug administration: an emerging tool for teaching clinical pharmacology during anesthesiology training. Clin Pharmacol Ther. 2008;84:170-1. [ Links ]
3. Muñoz L, Arévalo JJ, Reyes LE, Balaguera CE. Remifentanilo versus propofol con infusión controlada a objetivo en sitio efecto para la sedación de pacientes durante procedimientos endoscópicos gastrointestinales: ensayo clínico controlado aleatorizado. Rev Colomb Anestesiol. 2013;41:114-9. [ Links ]
4. Schnider TW, Minto CF, Shafer SL, Gambus PL, Andresen C, Goodale DB, et al. The influence of age on propofol pharmacodynamics. Anesthesiology. 1999;90:1502-16. [ Links ]
5. Minto CF, Schnider TW, Egan TD, Youngs E, Lemmens HJ, Gambus PL, et al. Influence of age and gender on the pharmacokinetics and pharmacodynamics of remifentanil. I. Model development. Anesthesiology. 1997;86:10-23. [ Links ]
6. Leslie K, Clavisi O, Hargrove J. Target-controlled infusion versus manually-controlled infusion of propofol for general anaesthesia or sedation in adults. Cochrane Database Syst Rev. 2008:CD006059. [ Links ]
7. Masui K, Upton RN, Doufas AG, Coetzee JF, Kazama T, Mortier EP, et al. The performance of compartmental and physiologically based recirculatory pharmacokinetic models for propofol: a comparison using bolus, continuous, and target-controlled infusion data. Anesth Analg. 2010;111:368-79. [ Links ]
8. Moerman AT, Herregods LL, De Vos MM, Mortier EP, Struys MM. Manual versus target-controlled infusion remifentanil administration in spontaneously breathing patients. Anesth Analg. 2009;108:828-34. [ Links ]
9. Gómez Oquendo FJ, Casas Arroyave FD, Fernández JM, Guarín Grisales Á. Anestesia total intravenosa en un sistema de lazo cerrado: reporte del primer caso en Colombia. Rev Colomb Anestesiol. 2013;41:306-10. [ Links ]
10. De Castro V, Godet G, Mencia G, Raux M, Coriat P. Target-controlled infusion for remifentanil in vascular patients improves hemodynamics and decreases remifentanil requirement. Anesth Analg. 2003;96:33-8. [ Links ]
11. Hill M, Peat W, Courtman S. A national survey of propofol infusion use by paediatric anaesthetists in Great Britain and Ireland. Paediatr Anaesth. 2008;18:488-93. [ Links ]
12. Muller T, Ludwig A, Biro P. Two distinct application habits for propofol: an observational study. Eur J Anaesthesiol. 2010;27:265-9. [ Links ]
13. Simpson RB, Russell D. Anaesthesia for daycase gynaecological laparoscopy: a survey of clinical practice in the United Kingdom. Anaesthesia. 1999;54:72-6. [ Links ]
14. Minai FN, Siddiqui KM, Qureshi R. Sedation-analgesia in non operative locations: practice trends of anaesthetists. J Pak Med Assoc. 2008;58:84-5. [ Links ]
15. Nora FS, Aguzzoli M, Oliveira Filho GR. Current attitude of anesthesiologists and anesthesiology residents regarding total intravenous anesthesia. Rev Bras Anestesiol. 2006;56:362-9. [ Links ]
16. Drews FA, Syroid N, Agutter J, Strayer DL, Westenskow DR. Drug delivery as control task: improving performance in a common anesthetic task. Hum Factors. 2006;48:85-94. [ Links ]
17. Syroid ND, Agutter J, Drews FA, Westenskow DR, Albert RW, Bermudez JC, et al. Development and evaluation of a graphical anesthesia drug display. Anesthesiology. 2002;96:565-75. [ Links ]
18. Kennedy RR. Seeing the future of anesthesia drug dosing: moving the art of anesthesia from impressionism to realism. Anesth Analg. 2010;111:252-5. [ Links ]
19. Gin T. Clinical pharmacology on display. Anesth Analg. 2010;111:256-8. [ Links ]
20. Guarracino F, Lapolla F, Cariello C, Danella A, Doroni L, Baldassarri R, et al. Target controlled infusion: TCI. Minerva Anestesiol. 2005;71:335-7. [ Links ]
21. Shafer SL, Siegel LC, Cooke JE, Scott JC. Testing computer-controlled infusion pumps by simulation. Anesthesiology. 1988;68:261-6. [ Links ]
22. R Development Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2008, ISBN 3-900051-07-0 [updated 2015 nov 1] http://www.R-project.org. [ Links ]
23. Lerou JG, Booij LH. Model-based administration of inhalation anaesthesia. 3. Validating the system model. Brit J Anaesth. 2002;88:24-37. [ Links ]
24. Kern SE, Xie G, White JL, Egan TD. A response surface analysis of propofol-remifentanil pharmacodynamic interaction in volunteers. Anesthesiology. 2004;100:1373-81. [ Links ]
25. Thompson JP, Rowbotham DJ. Remifentanil - an opioid for the 21st century. Brit J Anaesth. 1996;76:341-3. [ Links ]
26. Chang CH, Lee JW, Choi JR, Shim YH. Effect-site concentration of remifentanil to prevent cough after laryngomicrosurgery. Laryngoscope. 2013;123:3105-9. [ Links ]
27. Kim EJ, Shin SW, Kim TK, Yoon JU, Byeon GJ, Kim HJ. The median effective effect-site concentration of remifentanil for minimizing the cardiovascular changes to endotracheal intubation during desflurane anesthesia in pediatric patients. Korean J Anesthesiol. 2012;63:314-20. [ Links ]
28. Lee JY, Yang H, Choi SH, Shin DW, Hong SK, Chun DH. The optimal effect-site concentration of remifentanil to attenuate the pain caused by propofol. Korean J Anesthesiol. 2012;63:108-12. [ Links ]
29. Kwak HJ, Min SK, Kim DH, Kang M, Kim JY. Effect-site concentration of remifentanil for nasotracheal versus orotracheal intubation during target-controlled infusion of propofol. J Int Med Res. 2011;39:1816-23. [ Links ]
30. Lee B, Lee JR, Na S. Targeting smooth emergence: the effect site concentration of remifentanil for preventing cough during emergence during propofol-remifentanil anaesthesia for thyroid surgery. Brit J Anaesth. 2009;102:775-8. [ Links ]
31. Albertin A, Casati A, Federica L, Roberto V, Travaglini V, Bergonzi P, et al. The effect-site concentration of remifentanil blunting cardiovascular responses to tracheal intubation and skin incision during bispectral index-guided propofol anesthesia. Anesth Analg. 2005;101:125-30. [ Links ]
32. Bruhn J, Myles PS, Sneyd R, Struys MM. Depth of anaesthesia monitoring: what's available, what's validated and what's next? Brit J Anaesth. 2006;97:85-94. [ Links ]
33. Roberts FL, Dixon J, Lewis GT, Tackley RM, Prys-Roberts C. Induction and maintenance of propofol anaesthesia. A manual infusion scheme. Anaesthesia. 1988;43Suppl:14-7. [ Links ]











 text in
text in