Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Colombian Journal of Anestesiology
versão impressa ISSN 0120-3347
Rev. colomb. anestesiol. vol.44 no.3 Bogotá jul./set. 2016
Scientific and Technological Research
Estimation of the optimum length of endotracheal tube insertion in adults*
Estimación de la longitud óptima de inserción del tubo orotraqueal en adultos
Juan Camilo Gómeza,**, Lina Paola Melob, Yuliana Orozcob, Gustavo Adolfo Chicanganac, Diana Carolina Osorioc
a Anesthesiologist, Director of Anesthesiology, Universidad de Caldas, Manizales, Colombia
b Anesthesiologist, Universidad de Caldas, Manizales, Colombia
c Third Year Anesthesiology Resident, Universidad de Caldas, Manizales, Colombia
* Please cite this article as: Gómez JC, Melo LP, Orozco Y, Chicangana GA, Osorio DC. Estimación de la longitud óptima de inserción del tubo orotraqueal en adultos. Rev Colomb Anestesiol. 2016;44:228-234.
** Corresponding author at: calle 68a N° 9-100, casa 23, conjunto residencial Rincón de la Palma, Manizales, Colombia.
E-mail address: juan.gomez@ucaldas.edu.co (J.C. Gómez).
Article history: Received 9 February 2016 Accepted 1 May 2016 Available online 11 June 2016
Abstract
Introduction: An accurate estimation of the optimal length of endotracheal tube insertion can prevent complications such as endobronchial intubation, airway trauma and accidental extubation, all of which have a negative impact on patient safety and are associated with an increase in both morbidity and mortality.
Objective: To determine the optimal insertion length of endotracheal tubes in female and male adults according to their height.
Materials and Methods: A cross-sectional analytical study conducted with 516 adult ASA III female and male patients who had different surgical procedures requiring endotracheal intubation. The mouth-carina distance was obtained using a flexible fiberoptic bronchoscope. The data analysis was performed using the SPSS 15.0 software.
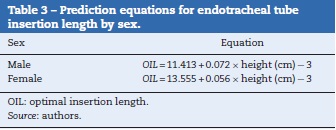
Results: Height and mouth-carina distance showed a direct and statistically significant correlation. Two equations for estimating optimal endotracheal insertion length were obtained, according to sex: men = 11.413 +(0.072 x height in cm) -3; and women = 13.555 + (0.056 x height in cm) - 3.
Conclusion: The traditional method of determining the insertion length of the endotracheal tube, 21 cm for women and 23 cm for men, shows a high incidence of endobronchial intubations in the analyzed population. The optimal insertion depth of the endotracheal tube can be reliably estimated through the use of prediction equations based on patient height, as proposed in this study.
Keywords: Bronchoscopy, Intubation, Airway management, Adult, Intraoperative complications.
Resumen
Introducción: Una correcta estimación de la longitud óptima de inserción del tubo orotraqueal puede prevenir complicaciones como: intubación endobronquial, trauma de la vía aérea y extubación accidental, las cuales inciden de manera negativa en la seguridad del paciente y se asocian con aumento en la morbimortalidad.
Objetivo: Determinar la longitud de inserción óptima del tubo orotraqueal a partir de la talla en pacientes adultos de ambos sexos.
Materiales y métodos: Estudio analítico de corte transversal en 516 pacientes adultos de ambos sexos, ASA I o II, intervenidos quirúrgicamente, quienes requirieron intubación oro-traqueal durante su procedimiento. La distancia boca-carina fue obtenida con la ayuda de un fibrobroncoscopio. El análisis de datos se efectuó con el software SPSS 15.0.
Resultados: La talla y la distancia boca-carina mostraron una correlación directa y estadísticamente significativa. Se obtuvieron dos ecuaciones para estimar la longitud de inserción óptima del tubo orotraqueal discriminadas según el sexo: hombres = 11,413+ (0,072 x talla en cm) - 3; mujeres = 13,555 + (0,056 x talla en cm) - 3.
Conclusión: El método tradicional para establecer la longitud de inserción del tubo oro-traqueal de 21 cm para mujeres y de 23 cm para hombres, muestra una alta incidencia de intubaciones endobronquiales en la población estudiada. La longitud de inserción óptima del tubo orotraqueal se puede determinar de forma segura a partir de las ecuaciones de predicción, basadas en la talla, propuestas en este estudio.
Palabras clave: Broncoscopía, Intubación, Manejo de la vía aérea, Adulto, Complicaciones intraoperatorias.
Introduction
The incorrect placement of an endotracheal tube can lead to serious complications including endobronchial intubation, vocal cord paralysis, accidental extubation, collapsed lung, hypoxemia, and pulmonary barotrauma, among others.1,2 Endobronchial intubation is the most common critical incident that can cause arterial desaturation during orotracheal intubation. According to the ASA Closed Claims Project, selective intubation accounts for 2% of adverse respiratory events in adults,3 and considering the more serious or fatal consequences of these events, including cerebral damage in up to 85% of patients,4 the correct placement of the tip of the endotracheal tube is a vital element in the practice of anes-thesiology and emergency and critical care medicine.
There are many methods to check the placement of the endotracheal tube, including the clinical method (auscultation of respiratory sounds, observation of the symmetry of chest expansion), palpation techniques (palpation of the endotracheal cuff in the suprasternal notch), imaging methods, capnography, direct visualization of the tip of the tube in relation to the carina using a fiberoptic bronchoscope1 and ultrasound,5 by either visualizing the tube directly in the airway or corroborating bilateral pleural sliding using a linear probe. However, these methods are not always based on evidence, nor are they always cost effective or applicable to every scenario of a given situation.1
Some authors have found that in 28% of patients with cardiac arrest, intubated by staff trained in advanced life support, the tip of the tube was endobronchial.6,7 Using the traditional insertion method of the endotracheal tube of 21 and 23 cm in women and men respectively as proposed in the literature several years ago,8 some publications show figures of more than 33.4% of endotracheal tubes incorrectly placed,9,10 this being a more frequent adverse event in women than in men (61.9% vs 38.1%).2 This gap is not considered ideal and is a big unknown when referring to populations with different anatomical proportions to those used in the initial study.
These considerations then raise the question: in adult patients requiring orotracheal intubation for whatever reason, what is the optimal distance for endotracheal tube insertion?
After an exhaustive search of all available electronic databases (Medline, Embase and Virtual Health Library), no literature was found that dealt with Latin American or Colombian populations.
Based on this, the objective of this study was to determine the length of optimum insertion of the endotracheal tube based on height for patients undergoing surgical procedures using intubation in two local tertiary hospitals.
Materials and methods
A cross-sectional study was conducted with a total population of 516 adults of both sexes, between the ages of 18 and 90, undergoing surgery in the Santa Sofia and SES Hospitals in Caldas, Colombia, between September 2011 and February 2015, classified as ASA I or II, and requiring orotracheal intubation during the procedure.
The minimum sample size (359 patients) was determined with the variance obtained from the height (69.4) from an estimated population of 1800 patients intubated per year in the operating rooms of Santa Sofia Hospital and 1500 patients in the SES Hospital of Caldas.
The criteria of exclusion were patients with hemodynamic instability, decompensated cardiorespiratory disease, and anatomical changes to the face, cervical region and upper airway.
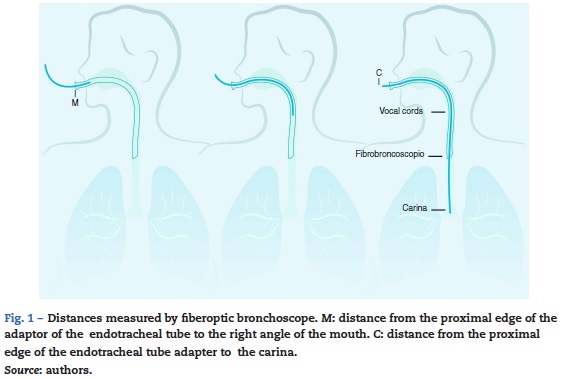
The variables studied were simple and grouped by age (under and over the age of 60), sex, height, distance from the proximal edge of the endotracheal tube adaptor to the right angle of the mouth (M), distance from the proximal edge of the tube adaptor to the carina (C) and mouth-carina distance (C-M).
Techniques and procedures
Previous authorization from the bioethics committees of the University of Caldas, the Santa Sofia Hospital and SES Hospital of Caldas was obtained in accordance with the Helsinki declaration, as well as authorization from each patient by signed, informed consent. Before admission to surgery, data was obtained from the preanesthetic evaluation form to record height, age and sex. In the cases where no height was registered, this was taken by researchers using a height rod with a sensitivity of 1 mm and 190 cm in length.
The data was obtained from patients who were undergoing general anesthesia in supine position, with the head in neutral position, and monitored using pulse oximetry, capnography, non-invasive blood pressure and electrocardiogram (ECG) with three leads. Each anesthesiologist selected the intubation technique as well as the size of the endotracheal tube and insertion length.
Once the patient was intubated with the endotracheal tube secured to the right labial commissure at a distance considered appropriate by the anesthesiologist, an OLYMPUS LB-GP fiberoptic bronchoscope of dm 4.1mm was inserted through a double lumen tube adaptor to prevent anesthetic circuit disconnection. The distances obtained during the procedure using direct vision of the anatomical structures were the following (Fig. 1).
Later, each distance marked on the fiberoptic bronchoscopy was measured using a metallic measuring tape with a sensitivity of one millimeter (Fig. 2). The distance obtained from the proximal edge of the tube to the carina (C) was measured and subtracted from the labial commissure, corresponding to the protruding portion of the mouth tube (M), which is how the carina-mouth distance (C-M) was finally determined.
Data analysis and software
All primary data was recorded on an instrument designed in Excel and was submitted to a preliminary pilot test for evaluation by experts, who considered the instrument to be adequate and sufficiently clear to collect the necessary data for the study. The statistical analysis was done using SPPS software v 15.0, licensed to the University of Caldas.
The qualitative variable was described using absolute and relative frequency. The quantitative variables were described with the average, confidence interval of 95%, standard deviation, mean, 5 and 95 percentiles and minimum and maximum values. For the prediction of the mouth-carina distance from the height of the patient, a Pearson correlation analysis was conducted after proving the normality of the dependent variable with the Kolmogorov Smirnov test. After this, various linear regression equations for sex and age group were estimated. The results are presented in tables according to the characteristics of the variables.
Results
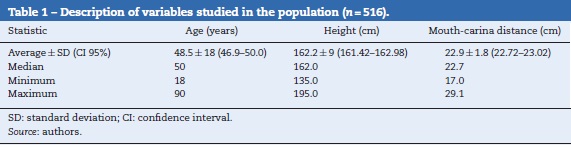
516 adults were studied between the ages of 18 and 90. Most of the population was under the age of 60 (71.3%) and a little over half (55.2%) were female.
The results of the study showed that in 41.1% of men and 14% of women the mouth-carina distance was under 23 and 21cm, respectively. In Table 1, a description of the quantitative variables of the studied population is provided.
After disaggregating the population data by sex and doing a mouth-carina distance analysis to confirm the normality of the variable, the average mouth-carina distance for men was 23.5 cm, and 22.4cm for women. For both sexes the differences between the median and the mean were minimal.
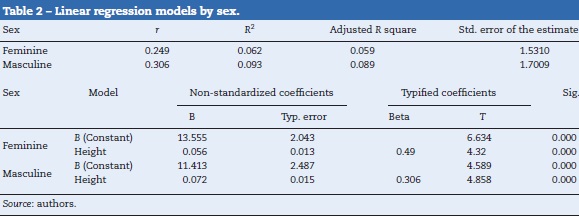
After doing a linear correlation analysis between the mouth distance variables and height, a direct and statistically significant correlation was found in all cases, for men and women both over and under the age of 60. The highest determination coefficient was for the population equal to or above 60 years of age.
Without controlling for age, and grouping the population by sex and using height as the independent variable, the following linear regression models were obtained (Table 2) along with their respective prediction equations (Table 3).
3 cm was subtracted from each of the equations obtained. This corresponds, according to the literature, to the distance that the tube should remain from the carina.8,11
The mouth-carina distance estimated with the prediction equations, without discriminating based on age (Table 3), and taking into account the median height for Colombian men (167 cm) and for women (155 cm) according to the National Survey of Nutritional Situation in Colombia (Encuesta Nacional de la Situación Nutricional de Colombia, ENSIN 2010), was as follows.
Men: Mouth-carina distance = 20.4 cm
Women: Mouth-carina distance = 19.2 cm
Discussion
The findings of this study are coherent with those published by other researchers in different contexts and with different populations,1,7,12-14 with regard to the controversy about the appropriate endotracheal tube insertion length for women and men, respectively. Were we to take these measures as a reference in our study, the tube would be endobronchial in 41.1% of men and in 14.1% of women. However, if the equations estimated in this study are considered, endo-bronchial intubation would be reduced to 2.6% and 5% in men and women, respectively.
Several studies exist of populations of different ethnic origin that relate the length of the airway with height. In 2002, in the Taiwanese population, the length of the airway from the mouth to the carina and its relationship with height was evaluated in 293 patients via fiberoptic bronchoscopy, obtaining a linear regression equation as a result: [height (cm)/5] - 13.8 Applying this equation to a Colombian woman with an average height of 155 cm, the optimal insertion length of the tube should be left at 18 cm. If the same exercise were done, but this time with the equation proposed in this study, the length would be 19.2 cm, representing a variation of 1.2 cm between the models.
In another study performed in Thailand in 2005 with a population of 100 patients, the Chula formula [4 + (height (cm)/10)] was used to determine the insertion length of the endotracheal tube, which, according to the conclusions, was successful in 99% of patients, insuring that the end of the tube remained at least 2 cm above the carina, and that the upper edge of the endotracheal cuff remained at least 2 cm below the vocal cords.6 When the equations are compared (the Chula formula and the equation from this study) with a 155 cm tall woman, the difference in the optimal insertion length of the tube would be 0.3 cm.
In India in 2011, a study was carried out with 200 patients, concluding when the endotracheal tube is positioned at between 21 and 23 cm, the end may come in contact with the carina or become endobronchial. As such, they proposed the following equation for determining the insertion length of the endotracheal tube: [height (cm)/7] -2.5.14 If we again consider a 155 cm tall female patient, the difference in the insertion length when comparing this equation with the proposed equation, would be 0.4 cm longer in the patients from India.
The three studies mentioned above were developed with non-Latin American populations,6,8,14 which may in part explain the difference in their results and those obtained here.
Contrary to what this study reports, some authors have found little correlation between height and airway length,7,13,15 arguing that this measure correlates between with external topographic measurements such as the distance from the corner of the mouth to the sternal manubrium,7 the distance from the upper incisors to the sternum,16 the distance from the cricoid cartilage to the xiphoid process, the sternal length, the length of the phalanges, the length of the ulna, and length of the foot,13 among others. Nevertheless, the difficulty of obtaining these measurements in emergency situations limits their usefulness and could increase the risk for the patient.
In agreement with other reports from the literature, the results of this study did not show differences related to sex in relation with the length of the airway6: if a man and a woman of equal heights are considered, and the formulas obtained in this study are applied, the mouth-carina distance is minimum.
Therefore, it would not be appropriate to propose an optimal endotracheal tube insertion length based exclusively on the sex of the patient, since the height ranges are wide in both men and women.
The limitation of this study lies in the fact that the sample of men and women was not selected at random. The patients included represent those scheduled for surgery during the time assigned for data collection.
Conclusion
The traditional method of determining the endotracheal tube insertion length as 21 cm for women and 23 cm for men shows a high incidence of endobrachial intubations. The results of this study present a statistically significant correlation between height and mouth-carina distance. Therefore, the proposed equations based on height dependably predict the optimal endotracheal tube insertion length.
Recomendations
The authors propose the used of Table 4, developed with heights for each sex, in which the optimal insertion length of the endotracheal tube is approximated in accordance with the prediction equations obtained in this study. Validating these values in later studies is proposed. Ideally, the above should be complemented with other strategies, such as auscultation, the direct viewing of the endotracheal tube balloon in its passage through the vocal cords, or thorax radiography.
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Financing
The present study was partially financed by the University of Caldas through recurring resources paid to the main researcher for teaching work and by contributions from Colciencias as support for the young researchers Drs. Lina Paola Melo and Yuliana Orozco as postgraduate residents during the initial phases of this project.
Conflicts of interest
The authors declare having no conflicts of interest.
References
1. Choi BR, Lee SY, Chung JY, Park SW, Kang WJ, Kang JM. Comparison of two topographical airway length measurements in adults. Korean J Anesthesiol. 2012;63:409-12. [ Links ]
2. Schwartz DE, Lieberman JA, Cohen NH. Women are at greater risk than men for malpositioning of the endotracheal tube after emergent intubation. Crit Care Med. 1994;22:1127-31. [ Links ]
3. Caplan RA, Posner KL, Ward RJ, Cheney FW. Adverse respiratory events in anesthesia: a closed claims analysis. Anesthesiology. 1990;72:828-33. [ Links ]
4. Szekely SM, Webb RK, Williamson JA, Russell WJ. The Australian Incident Monitoring Study. Problems related to the endotracheal tube: an analysis of 2000 incident reports. Anaesth Intensive Care. 1993;21:611-6. [ Links ]
5. Zamudio MA, Casas FD. El uso del ultrasonido en el manejo de la vía aérea. Rev Colomb Anestesiol. 2015;43:307-13. [ Links ]
6. Cherng CH, Wong CS, Hsu CH, Ho ST. Airway length in adults: estimation of the optimal endotracheal tube length for orotracheal intubation. J Clin Anesth. 2002;14:271-4. [ Links ]
7. Pak HJ, Hong BH, Lee WH. Assessment of airway length of Korean adults and children for otolaringology and ophtalmic surgery using a fiberoptic bronchoscope. Korean J Anesthesiol. 2010;59:249-55. [ Links ]
8. Owen RL, Cheney FW. Endobronchial intubation: a preventable complication. Anesthesiology. 1987;67:255-7. [ Links ]
9. Techanivate A, Kumwilaisak K, Samranrean S. Estimation of the proper length of orotracheal intubation by Chula formula. J Med Assoc Thai. 2005;88:1838-46. [ Links ]
10. Evron S, Weisenberg M, Harow E, Khazin V, Szmuk P, Gavish D, et al. Proper insertion depth of endotracheal tubes in adults by topographic landmarks measurements. J Clin Anesth. 2007;19:15-9. [ Links ]
11. Goodman LR, Conrardy, Laing F, Singer MM. Radiography evaluation of ETT position. Am J Roentgenol. 1976;127:433-4. [ Links ]
12. Chong DY, Greenland KB, Tan ST, Irwin MG, Hung CT. The clinical implication of the vocal cords-carina distance in anaesthetized Chinese adults during orotracheal intubation. Br J Anaesth. 2006;97:489-95. [ Links ]
13. Pang G, Edwards MJ, Greenland KB. Vocal cords/carina distance in anaesthetized caucasian adults and its clinical implications for tracheal intubation. Anaesth Intensive Care. 2010;38:1029-33. [ Links ]
14. Varshney M, Sharma K, Kumar R, Varshney PG. Appropriate depth of placement of oral endotracheal tube and its possible determinants in Indian adult patients. Indian J Anaesth. 2011;55:488-93. [ Links ]
15. Dey DK, Rothenberg E, Sundh V,Bosaeus I, Steen B. Height and body weight in the elderly: a 25-year longitudinal study of a population aged 70 to 95 years. Eur J Clin Nutr. 1999;53: 905-14. [ Links ]
16. Schellinger RR. The length of the airway to the bifurcation of the trachea. Anesthesiology. 1964;25:169-72. [ Links ]











 texto em
texto em