Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Colombian Journal of Anestesiology
versión impresa ISSN 0120-3347
Rev. colomb. anestesiol. vol.44 no.3 Bogotá jul./sep. 2016
Case report
Epidural anesthesia for posterior spinal fusion and lumbar surgery in a patient with glanzmann's thrombasthenia - Case report and systematic review*
Anestesia epidural para artrodesis e instrumentación de columna lumbar porvia posterior en paciente con tromboastenia de glanzmann - informe de caso y revisión sistematica
Sergio Hernando Cabarique-Serranoa,b,c,d, Víctor Hugo González-Cárdenasb,d,e,**, Jean Pierre Dussán-Crosbyb, Rodolfo Enrique Páez-Gonzálezb,f, María Alejandra Ramírezb
a Anesthesiologist Intensivist, Department of Anesthesiology, Hospital Infantil Universitario de San José. Bogotá D. C., Colombia
b School of Medicine, Fundación Universitaria de Ciencias de la Salud (FUCS). Bogotá D. C., Colombia
c Intensive Care Unit, Clínica Universidad de La Sabana. Chía, Colombia
d School of Medicine, Universidad de La Sabana. Chía, Colombia
e Anesthesiologist, Clinical Epidemiologist and Master in Anesthesia and Regional Analgesia. Leading Coordinator Grupo Deorum Opus-Hospital Infantil Universitario de San José/ Hospital de San José / Fundación Universitaria de Ciencias de la Salud (FUCS). Bogotá D. C., Colombia
f Orthopedist, Subspecialist in Spinal Surgery. Hospital Infantil Universitario de San José. Bogotá D. C, Colombia
* Please cite this article as: Cabarique-Serrano SH, González-Cárdenas VH, Dussán-Crosby JP, Páez-González RE, Ramírez MA. Anestesia epidural para artrodesis e instrumentación de columna lumbar porvia posterior en paciente con tromboastenia de glanzmann - informe de caso y revisión sistematica. Rev Colomb Anestesiol. 2016;44:249-254.
** Corresponding author at: Cra. 52 No. 67A-71, Oficina de Anestesiología, Hospital Infantil Universitario de San José, Bogotá, Colombia.
E-mail address vhgonzalez@fucsalud.edu.co (V.H. González-Cárdenas).
Article history: Received 9 April 2015 Accepted 21 April 2016 Available online 7 June 2016
Abstract
Introduction: Lumbar spine arthrodesis under regional epidural anesthesia provides adequate hemodynamic stability and timely treatment of acute postoperative pain to patients undergoing the procedure. However, the presence of intimidating comorbidities limits its widespread practice.
Objetives: To describe the use of epidural anesthesia for spinal fusion in a patient with Glanzmann's Thrombasthenia and high anesthetic risk of cardiovascular complications.
Methodology: Case reports and clinical discussion based on a systematic search of the medical literature.
Results: Upon selecting the strategies for a literature search on various databases, some articles were selected from Pubmed, LILACS, and sciencedirect. The articles were screened based on title and abstract and 19 full text articles were analyzed and submitted for discussion of an appointed panel of experts (Anesthesiology Group) for inclusion herein.
Conclusion: The use of epidural anesthesia in spinal surgery of a patient with significant hematological and cardiovascular complications was a successful approach and represents one further step forward in the implementation of protocols and robust clinical trials for the management of complex patients like the one herein described.
Keywords: Epidural anesthesia, Anticoagulants, Arthrodesis, Spine, Thrombastenia.
Resumen
Introducción: La artrodesis de columna lumbar, bajo anestesia regional epidural, permite a los pacientes programados para éste tipo de procedimiento mantener una adecuada estabilidad hemodinámica y ser tratados oportunamente de su dolor postoperatorio agudo. Sin embargo, la presencia de intimidantes comorbilidades limita su práctica de forma generalizada.
Objetivos: Describir la utilización de anestesia epidural para artrodesis lumbar en un paciente con Tromboastenia de Glanzmann y alto riesgo anestésico de complicaciones de predominio cardiovascular.
Metodologia: Reporte de Casos y discusión clínica basada en búsqueda sistemática de la literatura médica.
Resultados: Tras la selección de estrategias para la búsqueda de la literatura en diferentes bases de datos, se obtuvieron artículos de Pubmed, LILACS y sciencedirect. Posterior a exclusión por titulo y resumen, analizamos 19 artículos en texto completo, los cuales fueron sometidos a sesiones de discusión por parte de un panel de expertos designado (Grupo de Anestesiología), y fueron incluidos en esta revisión.
Conclusión: Para este caso, el uso de la anestesia epidural en cirugía de columna, en un paciente con importantes comorbilidades hematológicas y cardiovasculares, fue una medida exitosa, y representa un paso más en la implementación de protocolos y estudios clínicos robustos para su uso en pacientes complejos como el descrito.
Palabras clave: Anestesia epidural, Anticoagulantes, Artrodesis, Columna vertebral, Trombastenia.
Introduction
Despite the development of new technologies and therapies, the objectives of anesthesia remain unchanged. The primary goal is still based on achieving five objectives: analgesia, hypnosis, relaxation, amnesia and hemodynamic stability, keeping the patient's characteristics and the surgical requirements in mind. Throughout the years, the choice between regional and general anesthesia has been debated in various scenarios, favoring the approach that ensures maximum safety and efficacy.
Regional anesthesia (RA) may provide stability and comfort both for the patient and the medical staff, optimal surgical times, timely discharge from the Post-Anesthesia Care Unit (PACU) and improved satisfaction; these are all valid considerations for the anesthesia team when making a decision.
Though general anesthesia (GA) for the lumbar spine1 has historically been the cornerstone for anesthesiology, various studies have questioned this approach, indicating that RA has a lower impact on hemodynamic stability during induction and maintenance of anesthesia and is associated with a considerable decrease in the use of pain killers as a result of lower immediate postoperative pain levels2-6 and less intra and postoperative bleeding.4
RA has shown improved cost-effectiveness as compared to GA in lumbar spine surgery.5 Furthermore, there is evidence that RA is associated with lower mortality during the first 30 days after surgery, which is particularly relevant in high cardiovascular risk patients.7 In contrast, other trials have described similar surgical times, satisfaction, surgeon comfort and length of stay in the recovery room, with no significant differences versus GA data.4,5,7
One of the big challenges the anesthetist faces in RA is in patients with prophylactic or therapeutic anticoagulation, dual anti-aggregation, and coagulopathies who are more likely to develop spinal or epidural hematoma (1 per 3000 to 150,000 patients).8-10 Increased bleeding and the need for blood products transfusion defy the decision to stop the prescribed anticoagulant medications due to the high risk of thrombosis or perioperative embolism.
Despite the strategies agreed by the ASRA (bridge therapy), the implementation of such strategies is still controversial under extreme cases such as the patienthereindiscussed.11-13
This is a report of a case that exemplifies the above arguments, followed by a discussion based on the information gathered from a systematic data search.
Case description
64-year old male with intermittent lumbar pain after three months of evolution. The level of pain is severe, with frequent paresthesia irradiating to the hips and lower extremities, with considerable difficulty to ambulate.
The relevant medical history included smoking, high blood pressure, and ischemic heart disease (two vessels treated with two stents five years back); the patient is under cardiology control due to persistent ischemic symptoms. Additionally, a femoral pseudo aneurysm developed in the right thigh which was managed with thrombin occlusion and Glanzmann coagulopathy.
The patient was evaluated by a spine orthopedist who diagnosed L4-L5 facet joint syndrome, with root compression. The initial therapies included: combined oral therapy with no improvement of the condition and failed posteromedial branch neurolysis of the lumbar plexus. The patient returned three months later and in view of the persistence of symptoms, was scheduled for percutaneous interspinous spacers.
The pre-anesthesia evaluation classified the patient as ASA III, non-assessable functional class and cardiac high risk (based on AHA and Lee's revised cardiac index). The patient was programmed for an intermediate bleeding risk procedure; the ECG indicated a right branch blockade and the most recent echocardiogram revealed adequate biventricular function (LVEF 65%), with diastolic dysfunction and non-dysfunctional aortic sclerosis. In view of the patient's condition, the decision was made to transfuse platelets prior to surgery and prepare ICU admission.
Medical intervention: Following the transfusion of four units of platelets and in accordance with the patient's refusal to undergo general anesthesia, we administered sedation and loco-regional anesthesia. Basic monitoring was provided, in addition to continuous invasive blood pressure monitoring; (40%) oxygen was administered via Venturi, Remifentanil (0.5 mcg/kg bolus and maintenance at 0.02 mcg/kg/min); Midazolam (1 mg) and Fentanyl (50 mcg), for achieving the sedation target (RASS-2). During surgery there was a need to convert to open surgery (Lumbar Arthrodesis), so in addition to sedation, epidural anesthesia was administered (point of insertion at L1-L2 with the tip of the catheter at T8). Intravascular or spinal - conventional test - placement was ruled out,14 and 50 mg of Bupivacaine plus 100 mcg of Fentanyl were administered.
Continuous range of hemodynamic stability was achieved in the course of the procedure, with the support of intermittent doses of phenylephrine for optimal cerebral and myocardial perfusion. Surgery was completed maintaining an adequate RASS throughout the procedure that lasted 95 min, with approximately 40 cc of blood loss. The patient was transferred to the ICU for hemodynamic monitoring and after obtaining a reasonable Aldrete score and satisfactory resolution of the lumbar pain with no need for additional care, we removed the epidural catheter early in order to restart anticoagulation therapy. The patient was then transferred to the inpatients unit and two days later was discharged.
Materials and methods
Our study designed the case description and openly discussed the most recent information on the topic, in an attempt to answer the following questions: Is epidural anesthesia the right choice for patients undergoing lumbar spine fusion? Is there any scientific support for the use of epidural anesthesia in cardiac patients and/or patients with a predisposition to bleed or taking anticoagulants?
With a view to analyze and discuss the case, in February 2015 a systematic data search was undertaken, complemented with a snowball strategy, in PubMed, Lilacs, Cochrane, and Ebsco as the Primary sources and ACP Journal Club, and National Library of Medicine Health Service Research as secondary sources; Graduate Dissertation and grey literature: OPENSIGLE, New York Academy of Sciences Grey Sources, Clinical Medicine Netprints.
The acronym "PICOS" was used to refer to the studies (PRISMA Declaration): "P": cardiac Patients and/or with predisposition to bleed, using anticoagulants, undergoing lumbar spine fusion; "I" (Intervention): regional anesthesia (epidural); "C": (Comparison) general anesthesia, and "O": (Outcomes) 1: Changes in hemodynamic stability during induction and maintenance of regional versus general anesthesia. 2: Potential adverse outcomes in patients with prophylactic or therapeutic anticoagulation, dual aggregation and/or coagulopathies, associated with regional anesthesia for lumbar spine fusion. "S": (Studies) Experimental trials in human subjects.
Similar search strategies were used for each one of the above databases. The Medline-PubMed - based approach was as follows:
- For oral anticoagulation and regional anesthesia: (("mouth"[MeSH Terms] OR "mouth"[All Fields] OR "oral"[All Fields]) AND ("anticoagulants"[Pharmacological Action] OR "anticoagulants"[MeSH Terms] OR "anticoagulants"[All Fields]) AND ("regional anaesthesia"[All Fields] OR "anesthesia, conduction"[MeSH Terms] OR ("anesthesia"[All Fields] AND "conduction"[All Fields]) OR conduction "anesthesia"[All Fields] OR ("regional"[All Fields] AND "anesthesia"[All Fields]) OR"regional anesthesia"[All Fields])) AND ("2005/02/06"[PDat]: "2015/02/03"[PDat]).
- For lumbar surgery and anesthesia: (("lumbar vertebrae"[ MeSH Terms] OR ("lumbar"[All Fields] AND "vertebrae"[All Fields]) OR "lumbar vertebrae"[All Fields] OR ("lumbar"[All Fields] AND "spine"[All Fields]) OR "lumbar spine"[All Fields]) AND ("surgery"[Subheading] OR "surgery"[All Fields] OR "surgical procedures, operative"[MeSH Terms] OR ("surgical"[All Fields] AND "procedures"[All Fields] AND "operative"[All Fields]) OR "operative surgical procedures"[All Fields] OR "surgery"[All Fields] OR "general surgery"[MeSH Terms] OR ("general"[All Fields] AND "surgery"[All Fields]) OR "general surgery"[All Fields]) AND ("anaesthesia"[All Fields] OR "anesthesia"[MeSH Terms] OR "anesthesia"[All Fields])) AND ("loattrfull text"[sb] AND "2005/02/06"[PDat]: "2015/02/03"[PDat] AND "humans"[MeSH Terms]).
- For lumbar fusion and anesthesia: ("lumbosacral region"[MeSH Terms] OR ("lumbosacral"[All Fields] AND "region"[All Fields]) OR "lumbosacral region"[All Fields] OR "lumbar"[All Fields]) AND interbody[All Fields] AND ("Nucl Eng Des/Fusion"[Journal] OR "fusion"[All Fields] OR "FUSION"[Journal] OR "fusion"[All Fields]) AND ("anaesthesia"[ All Fields] OR "anesthesia"[MeSH Terms] OR "anesthesia"[All Fields]).
- For Glanzmann thromboasthenia and surgery: (("thrombasthenia"[ MeSH Terms] OR "thrombasthenia"[All Fields] OR ("glanzmann"[All Fields] AND "thrombasthenia"[All Fields]) OR "glanzmann thrombasthenia"[All Fields]) AND ("surgery"[Subheading] OR "surgery"[All Fields] OR "surgical procedures, operative"[MeSH Terms] OR ("surgical"[All Fields] AND "procedures"[All Fields] AND "operative"[All Fields]) OR "operative surgical procedures"[All Fields] OR "surgery"[All Fields] OR "general surgery"[MeSH Terms] OR ("general"[All Fields] AND "surgery"[All Fields]) OR "general surgery"[All Fields])) AND systematic[sb].
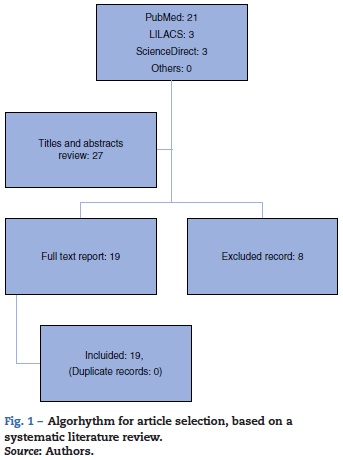
We considered article published between 2005 and 2015, in English and/or Spanish, and on experimental methodology applied to human subjects. The sessions to discuss the research articles and questions submitted before the experts panel at the Service of Anesthesiology of the San José Children's University Hospital required an analysis of the bibliography corresponding to each of the 19 articles considered relevant (for this study: included) (Fig. 1).
Results
Based on the selection strategies to undertake the literature search in the various databases suggested, 27 articles were collected: 21 in Pubmed, three in LILACS and three more in sciencedirect. Eight articles were excluded based on title and abstract, leaving 19 full text articles for evaluation. These were submitted for expert panel discussions and in the end were included in the discussion.
Discussion
Both Glanzmann's Thromboasthenia - a hereditary autosomal recessive predisposition with low incidence rates among the general population - (1:1000.000),15-17 and the presence of severe, difficult to manage, ischemic heart disease, further complicated our anesthetic and surgical approaches in a patient undergoing lumbar spine fusion, and required significant changes in the usual techniques to ensure better results, avoiding the most likely adverse outcomes in this type of interventions.
For decades, GA has been the gold standard for lumbar spine procedures1; however, several studies have shown that epidural RA results in optimization of analgesics, lower postoperative acute pain intensity, adequate hemodynamic stability, improved cost-effectiveness, and reduced mortality.2,7
Notwithstanding the lack of explicit literature on the management of anesthesia in patients with special characteristics (such as our patient), undergoing lumbar spine fusion, we argue that such predisposition to bleed should be approached similarly to the group of patients receiving anticoagulation or platelet anti aggregation. In other words, we must prepare ideal pro-coagulation conditions to prevent bleeding complications (similar to those recommended by ASRA)11-13 allowing for the manipulation of the neuraxis. The significance of having reliable, affordable, and quick methods available during the coagulation study for the right use of therapies that maximize the coagulation ability should be emphasized. This is the case with conventional or rotational thromboelastography.18,19 In our case, these interventions were secured with pre-surgical platelet concentrate transfusion and availability of recombinant Factor Vila,15,20 (specifically recommended by the FDA in Glanzmann's Thromboasthenia).21 However, we lack the relevant diagnostic devices to provide qualitative platelet recommendations beyond the conventional thrombus formation times which in the end are poorly effective to approach the intervention.
Whilst hemodynamic stability during surgery is an individual, multidimensional analysis, research has shown that this type of epidural anesthesia has the least impact on changing the vital signs and target organ perfusion pressures. Consequently, in selected cases and under selective and ultraselective techniques, may yield significant benefits.2,7 According to Popescu,22 epidural anesthesia in patients with ischemic heart disease, not only reduces the level of postoperative pain, but also the sympathetic load decreasing the cardiac oxygen demand and preventing cardiac decompensation. In our patient, these factors were probably the key toward achieving such encouraging results.
Conclusions
The use of epidural RA in lumbar arthrodesis procedures (particularly in patients with Glanzmann's Thromboasthenia and severe ischemic heart disease) needs further specific supportive research. Consequently, the successful anesthetic intervention in this particular case highlights the importance of researching alternative approaches to widely used general balanced anesthesia or total intravenous anesthesia (TIVA). The unbeatable outcomes achieved make us believe that RA could be the technique of choice in patients with the characteristics described above. Lastly, we recommend embarking on in-depth studies about the characteristics of RA in patients at high anesthetic risk undergoing similar procedures, including studies of stronger epidemiological impact and the potential to make general recommendations.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Funding
This study was funded by the authors' resources.
Conflict of interest
The researchers have no conflict of interests to disclose with regards to the data reported and the systematic literature review.
References
1. Sadrolsadat SH, Mahdavi AR, Moharari RS, Khajavi MR, Khashayar P, Najafi A, et al. A prospective randomized trial comparing the technique of spinal and general anesthesia for lumbar disk surgery: a study of 100 cases. Surg Neurol. 2009;71:60-5. [ Links ]
2. Schroeder KM, Zahed C, Andrei AC, Han S, Ford MP, Zdeblick TA. Epidural anesthesia as a novel anesthetic technique for anterior lumbar interbody fusion. J Clin Anesth. 2011;23:521-6. [ Links ]
3. Nagashima K, Sato S, Hyakumachi T, Yanagibashi Y, Masuda T. A prospective evaluation of anesthesia for posterior lumbar spine fusion: the effectiveness of preoperative epidural anesthesia with morphine. Spine (Phila Pa 1976). 2005;30:863-9. [ Links ]
4. De Rojas JO, Syre P, Welch WC. Regional anesthesia versus general anesthesia for surgery on the lumbar spine: a review of the modern literature. Clin Neurol Neurosurg. 2014;119:39-43. [ Links ]
5. Kahveci K, Doger C, Ornek D, Gokcinar D, Aydemir S, Ozay R. Perioperative outcome and cost-effectiveness of spinal versus general anesthesia for lumbar spine surgery. Neurol Neurochir Pol. 2014;48:167-73. [ Links ]
6. Chowdhury T, Narayanasamy S, Dube SK, Rath GP. Acute hemodynamic disturbances during lumbar spine surgery. J Neurosurg Anesthesiol. 2012;24:80-1. [ Links ]
7. Guay J, Choi P, Suresh S, Albert N, Kopp S, Pace NL. Neuraxial blockade for the prevention of postoperative mortality and major morbidity: an overview of Cochrane systematic reviews. Cochrane Database Syst Rev. 2014;1:Cd010108. [ Links ]
8. Parvizi J, Viscusi ER, Frank HG, Sharkey PF, Hozack WJ, Rothman RR. Can epidural anesthesia and warfarin be coadministered? Clin Orthop Relat Res. 2007;456:133-7. [ Links ]
9. Green L, Machin SJ. Managing anticoagulated patients during neuraxial anaesthesia. Br J Haematol. 2010;149:195-208. [ Links ]
10. Horlocker TT. Regional anaesthesia in the patient receiving antithrombotic and antiplatelet therapy. Br J Anaesth. 2011;107 Suppl. 1:i96-106. [ Links ]
11. Horlocker T, Benzon H, Brown D, Enneking K, Heit J, Mulroy MF, et al. Anestesia Regional en el paciente anticoagulado: Definición de Riesgos. Rev Colomb Anestesiol. 2005:59-64. [ Links ]
12. Gogarten W, Vandermeulen E, Van Aken H, Kozek S, Llau JV, Samama CM. Regional anaesthesia and antithrombotic agents: recommendations of the European Society of Anaesthesiology. Eur J Anaesthesiol. 2010;27:999-1015. [ Links ]
13. Benzon HT, Avram MJ, Green D, Bonow RO. New oral anticoagulants and regional anaesthesia. Br J Anaesth. 2013;111 Suppl. 1:i96-113. [ Links ]
14. Galindo Gualdróna LA. Dosis de prueba para anestesia regional. Rev Colomb Anestesiol. 2014;24:47-52. [ Links ]
15. Lison S, Spannagl M, Heindl B. Perioperative haemostatic management of Glanzmann thrombasthenia for abdominal surgery. Blood Coagul Fibrinolysis. 2009;20:371-3. [ Links ]
16. Varkey I, Rai K, Hegde AM, Vijaya MS, Oommen VI. Clinical management of Glanzmann's thrombasthenia: a case report. J Dent (Tehran). 2014;11:242-7. [ Links ]
17. Nurden AT. Glanzmann thrombasthenia. Orphanet J Rare Dis. 2006;1:10. [ Links ]
18. Sulaiman OM, Pabón GA, Cortés CC, Munoz LA, Reyes LE, Arevalo JJ. Un resumen de la investigación en tromboelastografía. Rev Colomb Anestesiol. 2014;42:302-8. [ Links ]
19. Gempeler FE, Perea AH, Díaz L. Tromboelastografía: evaluación global de la coagulación. Aplicaciones en el periodo perioperatorio. Rev Colomb Anestesiol. 2011;39:410-23. [ Links ]
20. Uzunlar HI, Eroglu A, Senel AC, Bostan H, Erciyes N. A patient with Glanzmann's thrombasthenia for emergent abdominal surgery. Anesth Analg. 2004;99:1258-60. [ Links ]
21. Biological License Application Supplement Noteworthy Approvals U.S: FDA; 2014 [updated 01.20.15; cited 25.02.15] . Available from: http://www.fda.gov/biologicsbloodvaccines/developmentapprovalprocess/biologicalapprovalsbyyear/ucm385849.htm. [ Links ]
22. Popescu WM, Gusberg RJ, Barash PG. Epidural catheters and drug-eluting stents: a challenging relationship. J Cardiothorac Vasc Anesth. 2007;21:701-3. [ Links ]











 texto en
texto en