Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Colombian Journal of Anestesiology
Print version ISSN 0120-3347
Rev. colomb. anestesiol. vol.45 supl.1 Bogotá Jan. 2017
Case report
Severe anaphylaxis reaction from dipyrone without a history of hypersensitivity. Case report☆
Reacción de anafilaxia grave por dipirona sin antecedente de hipersensibilidad. Informe de caso
Jorge Enrique Machado-Albaa,*, Sivia Fernanda Urbano-Garzóna, Yeinson Nabor Gallo-Gómeza, Sergio Zuluaicab, Yuly Henaob, Ilsa Yadira Parrado-Fajardob
a Pharmacoepidemiology and Pharmacovigilance Research Group, Universidad Tecnológica de Pereira-Audifarma S.A., Pereira, Colombia
b Management, Pharmacoepidemiology, Audifarma S.A., Pereira, Colombia
☆ Please cite this article as: Machado-Alba JE, Urbano-Garzón SF, Gallo-Gómez YN, Zuluaica S, Henao Y, Parrado-Fajardo IY. Reacción de anafilaxia grave por dipirona sin antecedente de hipersensibilidad. Informe de caso. Rev Colomb Anestesiol. 2017;45:8-11.
* Corresponding author at: Calle 105 No. 14-140. Pereira, Colombia.
E-mail address: machado@utp.edu.co (J.E. Machado-Alba).
Article history: Received 19 March 2015 Accepted 5 November 2015 Available online 30 May 2016
Abstract
Introduction: The safety of dipyrone has been the object of numerous debates, since severe allergic reactions to it can occur with an estimated incidence of 1 in 5000 parenteral administrations.
Clinical findings: We report the case of one patient who, after an infusion with dipyrone, presented coughing, pharynx itch, dyspnea, generalized cyanosis, and decreased consciousness. The diagnosis of anaphylactic shock without a history of hypersensitivity to the medication was made, and despite treatment with orotracheal intubation, adrenaline, hydrocortisone, sodium chloride, and sodium bicarbonate, it was fatal for the patient.
Conclusion: Cases of severe hypersensitivity without antecedents can be present in patients, which makes it important to recognize this risk in our patients.
Keywords: Dipyrone, Anaphylaxis, Pharmacovigilance, Drug-related side effects and adverse reactions Drug hypersensitivity.
Resumen
Introducción: La seguridad de la dipirona ha sido objeto de numerosos debates, ya que pueden aparecer reacciones alérgicas graves cuya incidencia estimada es de 1 en 5.000 administraciones parenterales.
Hallazgos clínicos: Se reporta un caso de una paciente que luego de una infusión con dipirona presenta tos, prurito faríngeo, disnea, cianosis generalizada y deterioro del estado de conciencia. Se hizo el diagnóstico de shock anafiláctico sin antecedentes previos de hipersensibilidad al medicamento, que a pesar del tratamiento con intubación orotraqueal, adrenalina, hidrocortisona, cloruro de sodio, y bicarbonato de sodio, resultó fatal.
Conclusión: pueden presentarse casos de grave hipersensibilidad en pacientes sin antecedentes de ésta, lo que hace importante reconocer este riesgo en nuestros pacientes.
Palabras clave: Dipirona, Anafilaxia, Farmacovigilancia, Efectos colaterales y reacciones adversas relacionados con medicamentos.
Introduction
Dipyrone (metamizole), derived from pyrazolone, is a non-opioid analgesic used for treating acute and chronic pain. It possible acts at the spinal and supraspinal level, and in the traumatized tissue. It is believed that it inhibits isoenzyme cyclooxygenase-3 especially in the central nervous system. It has antispasmodic properties, relaxing smooth muscle, and antipyretic effects at the level of the hypothalamic thermoregulatory center.1,2
Nevertheless, its safety generates numerous debates due to its association with agranulocytosis and anaphylaxis, for which it is banned in countries like the United States, while in others it is freely and widely used since is it cost effective and can be administrated through different routes.1,2 Although infrequent, allergic reactions as severe and lethal as anaphylactic shock and Stevens-Johnson syndrome can appear, even with fatal outcomes.1,3
Case description
Patient information and medical history
72-Year-old patient, female sex, of mestizo race, with a clinical picture of 12 hours of evolution characterized by general malaise, myalgia, arthralgia mainly in the knees, polyuria, and non-quantified fever. Medical history of arterial hypertension treated with 25 mg of captopril per day. Surgical history of lipoma resection and unspecified eye surgery; also an ex-smoker. She attended the same clinic four months previously with fever and urinary tract infection, which was treated with 1 g of intravenous (IV) dipyrone in a single dose in the hospital. She was released with acetaminophen and ciprofloxacin, without any drug-related adverse reactions.
Clinical findings
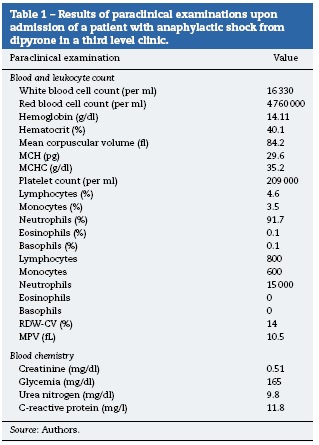
Admitted with 150/80 mmHg blood pressure, heart rate of 110ybpm, a respiratory rate of 20 breaths per minute, temperature of 38.5 °C, conscious and oriented without other findings in the physical examination. A diagnosis only of urinary tract infection and febrile syndrome was made. Paraclinical examinations are described in Table 1. There was insufficient time to perform urinalysis.
Therapeutic intervention
1 g of dipyrone was administered in 250 mL of 0.9% sodium chloride via IV. After injection of less than 20 mL of the solution, within two minutes from the start of the infusion, the patient referred to pruritus in the extremity where the venous access was located. Later, she presented coughing, pharyngeal pruritus followed by dyspnea, generalized cyanosis, and decreased consciousness with pupils unreactive to light. The infusion was immediately suspended, but the patient entered cardiorespiratory arrest. Cardiopulmonary resuscitation was initiated. Ventilation was performed with a bag valve mask and, later, with orotracheal intubation.
Pharmacological intervention
1 mg of adrenaline was administered via IV every 5 min to a total of 5 doses along with 200 mg of hydrocortisone and 500 mL of 0.9% sodium chloride via IV. In addition, defibrillation was performed on 3 occasions and 300 mg of amidarone (IV) was administered due to the presence of fine ventricular fibrillation. Later, the decision was made to administer 50 mEq of sodium bicarbonate, considering acidosis. After 40min of resuscitation efforts, a return to spontaneous circulation was not achieved. Without brainstem reflexes and with an idioventricular rhythm in the electrocardiograph monitor, the patient was declared deceased.
Informed consent
To acquire the information, informed consent was obtained from the patient's family. The following report is classified as research without risk in accordance with Resolution 8430 of 1993 of the Ministry of Health. The principles of beneficence and confidentiality outlined by the Declaration of Helsinki were respected.
Discussion
Dipyrone can be used for pain of varying origins. Its spasmolytic effect is used against colic pains and it is a useful antipyretic in adults and children.2 The incidence of anaphylactic reactions has been estimated at approximately 1 in 5000 parenteral administrations.2 The reactions may develop immediately or hours later, without depending on the dose administered. Rare cases have occurred without any antecedent of adverse reactions whatsoever.2 One study demonstrated a relatively low risk of intra-hospital severe anaphylactic reactions-similar to that of acetaminophen-associated with dipyrone. Nevertheless, reports describe serious allergic reactions, some with fatal outcomes as in this case.3-5
The mechanism of production of this severe disorder from dipyrone may be due to an anaphylactic reaction mediated by IgE antibodies or an anaphylactoid reaction mediated by the release of histamine in a nonspecific way.2 Anaphylaxis is an allergic reaction with multi-system effects. Severe cases can result in complete blockage of the respiratory tract and cardiovascular collapse due to vasogenic shock.6 Anaphylaxis is responsible for considerable potentially avoidable morbidity and mortality.7 The first symptoms are often unspecific: tachycardia, erythema, urticaria, wide-spread or localized pruritus, and a feeling of imminent death. There is compromise of the respiratory tract, with rhinitis or coughing. As the respiratory compromise becomes more severe, the edema of the upper airway may cause stridor and, in the lower airway, wheezing.6,8
Cardiovascular collapse is common in severe anaphylaxis. If not corrected rapidly, vasodilation and the increase in capillary permeability cause a decrease in the preload and relative hypovolemia that may quickly lead to cardiac arrest. Myocardial ischemia, acute myocardial infarction (AMI), arrhythmias, and cardiovascular depression can contribute to rapid hemodynamic deterioration and cardiac arrest. Furthermore, cardiac dysfunction can be the result of an underlying disease, and it is worth considering sepsis or the development of myocardial ischemia due to hypotension or the coincidental appearance of an acute coronary syndrome due to vasospasm secondary to allergic reaction (Kounis Syndrome).6,9 This, like cardiogenic shock, is extremely infrequent, since generally it presents as an unstable angina.10 Given the limited evidence, the management of cardiac arrest secondary to anaphylaxis should be treated according to the standard resuscitation guidelines in force, accompanied by treatment of anaphylaxia.6 It is critical to immediately initiate cardiopulmonary resuscitation and to not delay advanced airway management, given the rapid development of oropharyngeal or laryngeal edema.6
Should a permeable venous access be available, it is reasonable to consider the IV route as an alternative for the administration of epinephrine in anaphylactic shock. The recommended dosage of 0.2-0.5 mg can be repeated every 5-15 min in the absence of clinical improvement.6 Furthermore, volume replacement is essential with a bolus of 20-30 mL/kg of patient weight using isotonic crystalloids to maintain a systolic arterial pressure >90mmHg.6
Randomized clinical studies that evaluate the use of other therapeutic agents in anaphylactic shock and cardiac arrest do not exist. However, the simultaneous adjuvant use of anti-histamines, 02-agonists, and systemic corticosteroids via IV have been successful in the treatment of these patients.6 Anti-histamines are slower in their onset of action and have little effect on arterial pressure. Diphenhydramine (H1 antagonist) has been used at a dosage of 25-50 mg administered intramuscularly or in a slow IV infusion. It has been reported that treatment with a combination of H1 and H2 antagonists maybe more effective in the mitigation of manifestations than treatment with one only, and 1 mg/kg of parenteral ranitidine may be considered.6 Glucocorticosteroids, like methylprednisolone (1-2 mg/kg) or hydrocortisone (200 mg) have not proved effective for the treatment of acute anaphylaxis, but could, in theory, avoid prolonged anaphylaxis.7 Inhaled 02-agonists can be given to patients with wheezing, respiratory difficulty or coughing, especially when the bronchospasm does not respond to adrenaline.7
Limitations
Given the rapid outcome in this case, it was not possible to assess through blood cultures if the patient showed evidence of sepsis, or of acute myocardial infarction through enzyme markers.
Conclusion
The differential diagnosis should be considered with Kounis syndrome and the exacerbation of sepsis as a consequence of hypotension associated with the use of dipyrone. However, a few cases of severe anaphylaxis in patients with no history of hypersensibility have been reported. For this reason, it was believed that the clinical picture corresponded to an event associated with dipyrone. Being such a widely used analgesic in our country, it is worth being reported on so that health personal can recognize this risk in their patients, be alert to any sign of allergic response to the medication, and begin proper treatment in an opportune manner.
Main lessons
Cases of anaphylactic shock secondary to the administration of dipyrone in patients without a history of hypersensitivity may occur. This is a rare condition, but very relevant clinically due to the severity that it may have.
Financing
This work was financed by the Universidad Tecnológica de Pereira and Audifarma S.A.
Bioethical declaration
This case report was prepared with the informed consent of the patient's family in compliance with resolution No. 8430 of 1993 from the Ministry of Health of Colombia, guaranteeing the confidentiality of the patient's personal information in accordance with the principles of the Declaration of Helsinki.
Conflict of interest
The authors have no conflicts of interest to declare.
References
1. Stamer UM, Soehlea M, Park TW, Fischera M, Stubera F. Anaphylactic reaction after intravenous dipyrone. Acute Pain. 2007;9:221-7. [ Links ]
2. Nikolova I, Tencheva J, Voinikov J, Petkova V, Benbasat N, Danchev N. Metamizole: a review profile of a well-known "forgotten" drug. Part I: pharmaceutical and nonclinical profile. Biotechnol Biotechnol Eq. 2012;26:3329-37. [ Links ]
3. Machalett H. Case report on an anaphylactic shock following intravenous administration of analgin (sodium noraminophenazonemethanesulfonate) with fatal outcome. Z Arztl Fortbild (Jena). 1978;72:280-2. [ Links ]
4. International Collaborative Study of Severe Anaphylaxis. Risk of anaphylaxis in a hospital population in relation to the use of various drugs: an international study. Pharmacoepidemiol Drug Saf. 2003;12:195-202. [ Links ]
5. Hernandez C, Aragones N, Estanyol N, Bartra J, Castillo I, Villalonga A. Two cases of anaphylactic shock after metamizol given during postoperative recovery. Rev Esp Anaesthsiol Reanim. 2004;51:168-9. [ Links ]
6. Vanden Hoek TL, Morrison LJ, Shuster M, Donnino M, Sinz E, Lavonas EJ, et al. Part 12: cardiac arrest in special situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S829-61. [ Links ]
7. Alrasbi M, Sheikh A. Comparison of international guidelines for the emergency medical management of anaphylaxis. Allergy. 2007;62:838-41. [ Links ]
8. Williams KW, Sharma HP. Anaphylaxis and Urticaria. Immunol Allergy Clin North Am. 2015;35:199-219. [ Links ]
9. Martínez Juste JF, Ruiz Garces T, Gonzalez Enguita R, Cia Blasco P, Altemir Trallero J. Cardiac complications in a metamizole-induced type I Kounis síndrome. Rev Bras Anestesiol. 2014;66:194-6. [ Links ]
10. Garcipérez de Vargas FJ, Mendoza J, Sánchez-Calderón P, Ortiz C, Porro R, Mogollón-Jiménez MV. Cardiogenic shock secondary to metamizole-induced type II Kounis syndrome. [ Links ]











 text in
text in