Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Colombian Journal of Anestesiology
versão impressa ISSN 0120-3347
Rev. colomb. anestesiol. vol.45 supl.1 Bogotá jan. 2017
Case report
A diagnostic dilemma in an alert patient with pulmonary oedema following craniotomy: A case report☆
Dilema diagnóstico en un paciente despierto con edema pulmonar tras craneotomía: reporte de caso
Kosuke Tsubaki, Satoki Inoue*, Masahiko Kawaguchi
Division of Intensive Care and Department of Anesthesiology, Nara Medical University, Nara, Japan
☆ Please cite this article as: Tsubaki K, Inoue S, Kawaguchi M. Dilema diagnóstico en un paciente despierto con edema pulmonar tras craneotomía: reporte de caso. Rev Colomb Anestesiol. 2017;45:71-75.
* Corresponding author at: Division of Intensive Care and Department of Anesthesiology, Nara Medical University, 840 Shijocho Kashihara, Nara 634-8522, Japan.
E-mail address seninoue@naramed-u.ac.jp (S. Inoue).
Article history: Received 13 April 2016 Accepted 14 October 2016 Available online 6 December 2016
Abstract
Introduction: We present a case developing idiopathic pulmonary oedema following craniotomy without any neurological symptoms.
Case description: A 70-year-old female, who had unremarkable medical history, underwent removal of brain tumour under general anaesthesia. Craniotomy was uneventfully performed and her respiratory and haemodynamic conditions during the operation were normal. Immediately after the operation, she regained consciousness and was neurologically intact. However, her oxygenation was not sufficient without oxygen administration, her chest X-ray showed pulmonary oedema. Gradually, her pulmonary oedema in the chest X-rays disappeared. There was no specific reason of pulmonary oedema except for intracranial manipulation, therefore, it was considered as neurologic pulmonary oedema.
Conclusion: In this case, we merely might have followed the restoration process from neurologic pulmonary oedema developing during the operation.
Keywords: Neurosurgery, Pulmonary edema, Perioperative period, Meningioma, General Anesthesia.
Resumen
Introducción: Presentamos un caso de desarrollo de edema pulmonar idiopático tras craneotomía sin síntomas neurológicos.
Descripción del aso: Una paciente de sexo femenino de 70 años de edad con una historia médica sin interés se sometió a una extirpación de tumor cerebral bajo anestesia general. La craneotomía se realizó sin eventos notables y sus condiciones respiratorias y hemodinámicas durante la operación se mantuvieron normales. Inmediatamente al concluir la operación la paciente recobró su conciencia y se encontró en estado neurológico intacto. Sin embargo, su oxigenación no era suficiente sin administración de oxígeno, y las radiografías indicaban edema pulmonar. Gradualmente su edema pulmonar visualizado en las radiografías torácicas desapareció. No había ninguna razón para el edema pulmonar excepto manipulación intracraneal, así que fue considerado como un edema pulmonar neurológico.
Conclusión: En este caso, habríamos simplemente seguido el proceso de restauración del edema pulmonar neurológico que se desarrolló durante la operación.
Palabras clave: Neurocirugia, Edema pulmonar, Periodo perioperatorio, Meningioma, Anestesia general.
Introduction
Pulmonary oedema is fluid accumulation in the air spaces and parenchyma of the lungs.1 It leads to impaired gas exchange and may cause respiratory failure. Neurogenic pulmonary oedema (NPE) is a clinical syndrome characterised by the acute onset of pulmonary oedema following a significant central nervous system (CNS) insult. The aetiology is thought to be a surge of catecholamines that results in cardiopulmonary dysfunction.2 It has been proposed that neurologic conditions that cause abrupt, rapid, and extreme elevation in intracranial pressure (ICP) appear to be at greatest risk of being associated with NPE although the pathophysiological mechanisms remain obscured.3,4 We present the case of a patient developing idiopathic pulmonary oedema following craniotomy without any neurological symptoms.
Case description
Patient information
The consent of patient and institutional review board approval were obtained for this case presentation. A 70-year-old female was admitted to our hospital for undergoing removal of the brain tumour. She previously underwent neck clipping and coil embolisation for an unruptured intracranial aneurysm. She was medicated with antihypertensive agents. The brain tumour was in the right parietal lobe adjacent to the falx, which was speculated to be the falx meningioma based on the imaging study. Her tumour happened to be discovered by follow-up CTs for her intracranial aneurysm. Therefore, her neurological symptoms were absent; however, the tumour was showing tendency to expand. Except for hypertension, she had no clinical evidence of cardiac disease, or respiratory disease. Preoperative Chest X-ray was unremarkable.
Clinical findings, diagnostic assessment and interventions
Craniotomy and removal of the brain tumour was performed. Under general anaesthesia, the patient was put on the operating table in the left park-bench position. During surgery, cardiac output as well as intensive arterial blood pressure were monitored using FloTracTM sensor and VigileoTM monitor.
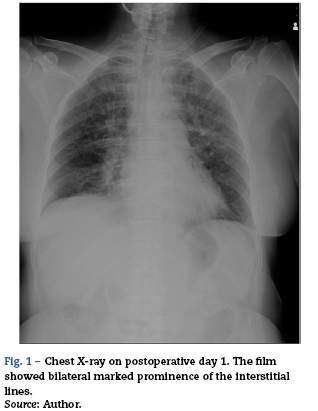
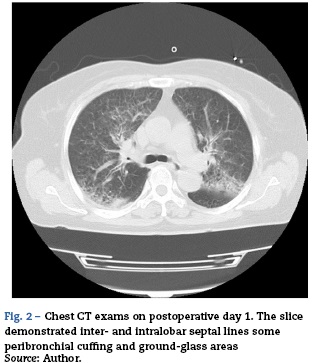
Saturation of peripheral oxygen (SpO2) and end-tidal carbon dioxide concentration (ETCO2) were also continuously monitored. The operation time for the procedures was 99 min. Fluid balance was 1290 ml. No transfusion was performed. During the operation, the patient's haemodynamics were stable with blood pressure of around 120/80 mmHg and 3.5-IL/min of cardiac output. Respiratory condition was also stable; however, SpO2 was slightly decreased as the end of operation neared. Immediately after the operation, she was returned to the supine position and her trachea was suctioned; however, only a small amount of frothy sputum was observed. Simultaneously, she regained consciousness and spontaneous breathing was sufficient, then the tracheal tube was removed and she was transferred to the intensive care unit (ICU). After admission to the ICU, she remained alert and neuro-logically unchanged. Oxygen was administered by facemask at 6Lmin-1; however, her SpO2 showed 90-96% and PaO2 was 89 torr with deep breathing urged. She never complained of dyspnoea no matter how many times we asked although she were coughing up and spitting out. Her haemodynamics was stable throughout the ICU stay. Transthoracic echocardiogram showed normal left ventricular function and normal chamber size. On the next day, her bladder temperature was 37.1 °C. Inflammatory markers, such as C-reactive protein (CRP) and white blood cell (WBC) counts, were 1.3 mg/dl and 11,000/[xl with prophylactic administration of cefazolin 2 g/day for surgical site infection. Presentation of active pneumonia seemed negative. However, a chest X-ray taken on that day, which showed bilateral marked prominence of the interstitial lines, were consistent with pulmonary oedema (Fig. 1). A subsequent CT exam, which demonstrated inter- and intralobar septal lines some peribronchial cuffing and ground-glass areas, confirmed the diagnosis of pulmonary oedema (Fig. 2).
Follow-up and outcome
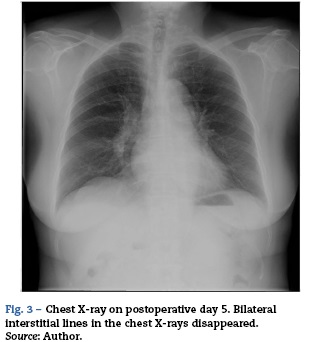
She was still monitored closely in the ICU according to the institutional standard care for neurosurgical patients but was observed only with oxygen administration. Diuretics or any specific therapies were not applied. Gradually, bilateral interstitial lines in the chest X-rays spontaneously disappeared (Fig. 3). On the 5th postoperative day, she was finally weaned from oxygen therapy.
Discussion
Two main types of pulmonary oedema are recognised: first, cardiogenic (or hydrostatic) pulmonary oedema from an elevated pulmonary capillary pressure from left-sided heart failure; second, noncardiogenic (increased permeability) pulmonary oedema from injury to the endothelial and epithelial barriers.1 The pathophysiology of NPE probably involves an adrenergic response to the CNS insult, which leads to increased pulmonary hydrostatic pressure and increased lung capillary permeability related to the inflammatory response.2 In some patients, cardiac dysfunction may predominate, in others, capillary leak is the primary manifestation.5 These patterns have obvious implications for the diagnosis and treatment of individual cases, including cardiac evaluation, fluid management, and choice of inotropic or vasoactive substances.6 Reviewing our case, it is a fact that she developed pulmonary oedema although its severity was not so critical. Considering the timing of its development was thought to be during the operation and there was no specific reason of pulmonary oedema except for intracranial manipulation, it is reasonable to conclude that it was a kind of NPE. Regarding the positive fluid balance during the operation (1290 ml), it may not be denied that this fluid balance could have contributed to the pulmonary oedema; however, the fluid balance like this for the elective neurosurgery is common in our institute because of preoperative fasting. We cannot completely deny that she developed acute congestive cardiac failure since we did not measure the pulmonary artery wedge pressure. However, this was very unlikely to cause pulmonary oedema considering her haemodynamics were stable. That's a natural enough suspicion why the patient's neurological condition did not get worse because NPE has been reported usually to accompany with abrupt, rapid, and extreme elevation in ICP.3,4 The patient might have gotten worse during a follow-up observation because there is a report showing a case developing NPE prior to neurological deterioration and elevation in ICP.7 Therefore, pulmonary oedema could have been one of signs for impending neurological deterioration. However, her pulmonary oedema was spontaneously resolved. Alternatively, we merely might have followed the restoration process from NPE developing during the operation, which had been masked by positive pressure ventilation. Suppose it were so, many NPE cases might have been overlooked in the clinical settings.
It has been reported that moderate or pronounced brain swelling accompanying with elevated ICPs occurred in 35.7% of patients during craniotomy for supratentorial brain tumours.8 Thus, there is no doubt that temporary neuronal compression, ischaemia, or damage should occur during any intracranial manipulations, which might cause NPE in a certain neurosurgical population. So-called "NPE trigger zones" include the hypothalamus and the medulla, specifically area A1, A5, nuclei of solitary tract and the area postrema have been proposed to be anatomical origins.9 The surgical field in our case did not directly involve these areas; however, we cannot unconditionally deny that surgical insults indirectly affected these areas. In addition, there is a case report presenting NPE during a neurosurgical procedure not involving NPE trigger zones and raid improvement after the procedure.10 Development of NPE might not always require direct stimuli to these areas. Either way, it is safe to say that any intracranial manipulations have possibility to induce temporary NPE. Whether the temporary NPE developing during neurosurgery is sustained, deteriorate, or, resolved may depend on postoperative intracranial status.
Negative pressure pulmonary oedema (NPPE), acute lung injury, or anaphylaxis is can be considered as differential diagnoses. Upper airway obstruction and forceful inspiration are usually observed in developing NPPE.11 Upper airway obstruction and stridor are occasionally observed in postoperative neurosurgical patients. However, our patient was alert and upper airway was patent enough even in the early postoperative period. The possibility of acute lung injury due to aspiration or equivalents was negative according to her clinical course. It is not possible to deny anaphylaxis because many drugs were used during the perioperative period. However, she did not present typical anaphylactic reactions including hypotension, wheeze, or skin rash. Therefore, it is reasonable that her pulmonary oedema was diagnosed as NPE. As another differential diagnosis, pulmonary oedema seen after large air emboli occurring during craniotomy is a recognised phenomenon and has been reported.12 In addition, there is a report available that an unrecognised low level of intravenous air aspiration without haemodynamic sequelae can produce life-threatening pulmonary oedema.13 However, significant depression of ETCO2 was detected and recognised as a significant event even in this report although haemodynamic sequelae was not accompanied. Such an event was absent in our case; however, any craniotomy has the risk of intravenous air aspiration. Therefore, it is liable to objection or debate that unrecognised microemboli during craniotomy might have contributed to the development of this pulmonary oedema.
Conclusions
In conclusion, we had a case developing idiopathic pulmonary oedema following craniotomy without any neurological symptoms. It was considered that her pulmonary oedema was a kind of NPE. We merely might have followed the restoration process from NPE developing during the operation. However, the knowledge and awareness of this kind of clinical entity should guide perioperative evaluation and treatment because supportive care will allow spontaneous resolution for this case if further neurological deterioration does not happen.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Financing
This case report was supported only by the departmental source.
Conflict of interest
The authors have no conflicts of interest to declare.
References
1. Murray JF. Pulmonary edema: pathophysiology and diagnosis. Int J Tuberc Lung Dis. 2011;15:155-60. [ Links ]
2. Davison DL, Terek M, Chawla LS. Neurogenic pulmonary edema. Crit Care. 2012;16:212. [ Links ]
3. Ducker TB, Simmons RL. Increased intracranial pressure and pulmonary edema. Part 2: the hemodynamic response of dogs and monkeys to increased intracranial pressure. J Neurosurg. 1968;28:118-23. [ Links ]
4. Kosnik EJ, Paul SE, Rossel CW, Sayers MP. Central neurogenic pulmonary edema: with a review of its pathogenesis and treatment. Childs Brain. 1977;3:37-47. [ Links ]
5. Sedy J, Zicha J, Kunes J, Jendelova P, Sykova E. Mechanisms of neurogenic pulmonary edema development. Physiol Res. 2008;57:499-506. [ Links ]
6. Davidyuk G, Soriano SG, Goumnerova L, Mizrahi-Arnaud A. Acute intraoperative neurogenic pulmonary edema during endoscopic ventriculoperitoneal shunt revision. Anesth Analg. 2010;110:594-5. [ Links ]
7. Quader K, Manninen PH, Lai JK. Pulmonary edema in the neuroradiology suite: a diagnostic dilemma. Can J Anaesth. 2001;48:308-12. [ Links ]
8. Rasmussen M, Bundgaard H, Cold GE. Craniotomy for supratentorial brain tumors: risk factors for brain swelling after opening the dura mater. J Neurosurg. 2004;101:621-6. [ Links ]
9. Colice GL. Neurogenic pulmonary edema. Clin Chest Med. 1985;6:473-89. [ Links ]
10. Jacob FD, Wheatley MB, Sinclair DB. Acute neurogenic pulmonary edema after depth electrode placement for epilepsy surgery. Can J Neurol Sci. 2010;37:885-7. [ Links ]
11. Krodel DJ, Bittner EA, Abdulnour R, Brown R, Eikermann M. Case scenario: acute postoperative negative pressure pulmonary edema. Anesthesiology. 2010;113:200-7. [ Links ]
12. Chandler WF, Dimcheff DG, Taren JA. Acute pulmonary edema following venous air embolism during a neurosurgical procedure. Case report. J Neurosurg. 1974;40:400-4. [ Links ]
13. Frim DM, Wollman L, Evans AB, Ojemann RG. Acute pulmonary edema after low-level air embolism during craniotomy Case report. J Neurosurg. 1996;85:937-40. [ Links ]











 texto em
texto em