Introduction
Blood transfusions are frequent perioperative procedures that are usually life-saving.1 However, keep in mind that this is a costly procedure involving multiple risks2-4;so there is a need to clearly identify which patients will benefit from having a red blood cells reserve.5
In terms of transfusion strategies, these have been evolving from a liberal approach to the use of red blood cells, to a restrictive approach aimed at reducing the number of patients requiring a transfusion through the implementation of protocols designed to reduce costs and procedure-associated morbidity.6
There is a need to rethink which patients need perioperative blood reserves, based on the procedure itself and the patient's risk factors.7
The purpose of this study was to establish the transfusion index and any risk factors associated with the perioperative transfusions administered at a third-level hospital in Bogotá, Colombia.
Methodology
Historical cohort trial including patients above 18 years of age, for whom a red blood cells reserve was prepared to undergo ambulatory or emergency surgery at a University Hospital in Bogotá, Colombia, from January 1 and December 31, 2014. Patients with incomplete medical records with missing variables were excluded. The mean age was 51.8 years, and 55% were males. A total of 1455 red blood cells (RBC) units were reserved and only 481 were administered. The point in time when the red blood cells reserve was made was the baseline and at this point the number of red blood cells units reserved was recorded. Patients were followed for 24hours postop, and the number of RBCs transfused in that time period was recorded. Based on an ideal usage number of 40% of the units reserved, with an actual use of 16.2%,8 the sample size was estimated at 164 patients with a 90% power.
Analysis of the data
The analysis was bivariate, using the SPSS statistical software package (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.). x2 tests were done with a significant statistical difference of P < 0.05. The transfusion relative risk (RR) was estimated for each type of surgery using tetrachoric tables; similarly, an individual analysis with each variable studied was carried out to identify risk factors. The reserve/transfusion indices were estimated proportionally to these data.
Ethical considerations
This research was compliant with the Declaration of Helsinki and the Colombian regulations (Resolution 8430 of 1993 of the Ministry of Health and Resolution 2378 of 2008 on colombian good clinical practices). The study was submitted to, and approved by, the ethics committee of the University Hospital where the trial was performed.
Results
The underlying hypothesis was that the clinic used a number of reserved units below the recommended level (minimum 40%). A total of 8490 medical records of patients that underwent surgery throughout 2014 were reviewed, of which 840 had a preoperative order for red blood cells reserve; this was the eligible population. However, incomplete medical records were identified that prevented the investigators from doing all the proposed calculations. Consequently, in order to avoid a selection bias, an estimate of the results was done with the available data and no significant differences were found. Finally, 490 patients were included in the trial.
In order to verify the information collected, a comparison was made against the database of patients transfused at the anesthesia service and the blood bank; furthermore, in addition to checking the data from the pre-anesthesia evaluation, the laboratory database was used to access the missing information in the pre-anesthesia evaluation.
In order to identify the perioperative transfusion-associated factors in our setting, the variables used in other trials were recorded, including age (the sample mean was the cut off point), sex, body mass index (BMI) for the malnutrition range (<18.5),9 preoperative hemoglobin based on the WHO cutoff point (13g/dL in males and 2g/dL in females),10 preexisting cardiovascular disease, emergency surgery, and surgical time exceeding the institutional average (Table 1).11
Table 1 Description of the population (n=490)
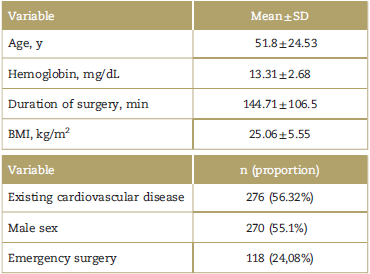
Note: BMI=body mass index, SD=standard deviation.
Source: Authors.
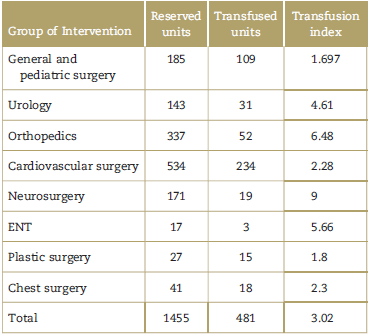
Then, in order to meet the objective of establishing the transfusion index for each group of surgical interventions, a ratio was used with the number of reserved units divided by the units transfused in each group. The same procedure was repeated in the consolidated for all the interventions (Table 2).
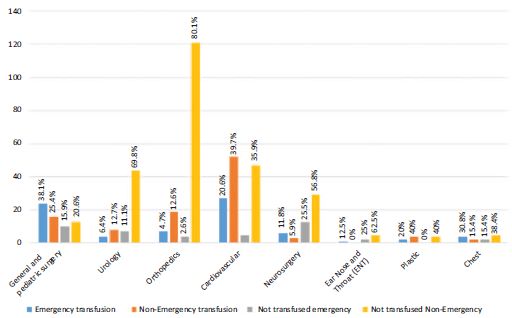
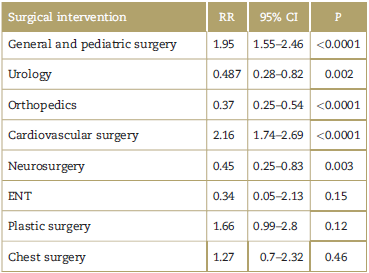
The next step in the analysis was to determine whether the type of surgical procedure plays an important role in determining the possibility of being transfused. Figure 1 shows that the procedures where patients are most frequently transfused are cardiovascular surgery and general surgery; likewise, these interventions present a higher risk of requiring perioperative transfusions. Other procedures did not show a statistically significant relationship (Table 3).
Among the categorical variables, emergency surgery was identified as a risk factor for requiring transfusions during the perioperative period (RR 2.27, 95% confidence interval [CI] 1.84-2.81), while regional anesthesia was identified as a protective factor (RR 0.347, 95% CI 0.23-0.51) (Table 4).
Table 4 Analysis of categorical variables
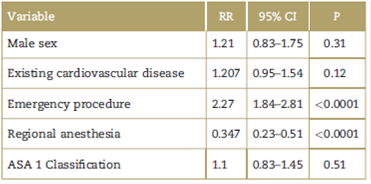
Note: ASA=American Society of Anesthesiologist.
Source: Authors.
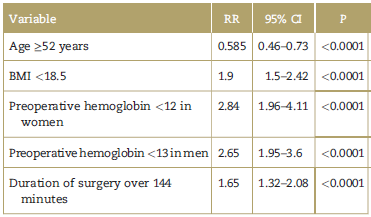
A BMI below 18.5, preoperative hemoglobin less than 12 g/dL in females and less than 13 g/dL in males, and above average surgical times (144 minutes) were all risk factors for perioperative transfusion, while age over 52 years was a protective factor (Table 5).
Discussion
Patient safety is a priority to all healthcare staff members. A rational use of red blood cells shall therefore become a management standard since it is well known that despite being a requirement under certain conditions, it is not risk-free and the risk-benefit ratio shall always be evaluated beforehand.12
Keeping in mind that one of the cost-reduction strategies and blood-saving techniques is to identify patients at risk of perioperative transfusion, this cohort study was developed identifying the reserve/transfusion indices and evaluating the variables perceived as risk factors for RBC transfusion at a third-level hospital.
With regard to the transfusion index, the pooled data of all the surgeries performed resulted in a 3.02 index, exceeding the recommended level. As compared against the ideal number (<2.5), neurosurgery procedures (index 9) exhibit excessive reserves that are not justified based on the actual usage of red blood cells.
Similarly, orthopedic procedures have a transfusion index of 6.48, also exceeding the recommended levels. For this group of interventions, a large number of units were reserved (337 reserved units for a total of 151 patients), but the actual use was only 26 units. Carling et al, reported in a recent trial that the prevalence of RBC transfusions in total hip or knee replacement is low and this is consistent with the results obtained. Furthermore, some factors were found to increase the risk of transfusion, including low preoperative hemoglobin, and low BMI1; these factors shall be kept in mind when ordering blood reserves. All other procedures exhibit transfusion indices within the recommended range.
Cardiovascular surgery was the procedure with the highest RBC transfusion requirements. The transfusion index for this group of procedures was 2.28, indicating that the reserves were consistent with the number of units used. Similar to this study, the guidelines for blood preservation of the Society of Chest Surgeons and the Society of Cardiovascular surgeons report a high percentage of blood transfusions in patients undergoing heart surgery-approximately 50%. So some recommendations are suggested to lower the transfusion indices: use medications that limit blood loss, use of coagulation factors, perform minimally invasive procedures, use of topical hemostatic agents, inter alia.13
Risk factors for red blood cells transfusion
An individualized analysis of each group of interventions showed that general and pediatric surgery represent a risk factor with an RR of 1.95 (95% CI 1.55-2.46) P < 0.0001, similar to cardiovascular surgery with an RR of 2.16 (95% CI 1.742.69) P < 0.0001. Urology, orthopedic, and neurosurgery exhibited a lower risk of transfusion among the patients studied, with an RR of 0.487, 0.37, and 0.45, respectively, with adequate confidence intervals and statistically significant P values. Ear nose and throat (ENT) procedures, plastic surgery, and chest surgery were not related to the outcome studied, indicating a considerable difference in the use of RBC among the different areas of specialization.
Among the categorical variables studied, the only one with a positive association was the emergency nature of the procedures, with an RR of 2.27 (95% CI 1.84-2.81) P< 0.0001. There is a potential explanation because trauma procedures-which more often require transfusions-are classified as emergency procedures. Another finding was that the use of regional anesthesia has a negative association, with an RR of 0.347 (95% CI 0.23-0.51) P< 0.0001; however, this association presents a selection bias since in the case of patients with a more severe condition, higher risk of decompensation and potential transfusion, anesthesiologists usually administer general anesthesia from the start. The remaining categorical variables failed to show an association with RBC transfusions.
With regard to the continuous variables, a negative association was identified with age over 52 years, with an RR 0.585 (95% CI 0.46-0.73) P < 0.0001, and this is related to the higher prevalence of interventions secondary to trauma in younger patients that require transfusions. Moreover, a BMI <18.5 (malnutrition according to the WHO definition) showed a positive correlation with an RR of 1.9 (95% CI 1.5-2.42) P < 0.0001; this is understandable considering that one of the primary causes of anemia in developing countries is malnutrition.14
Based on the WHO criteria for anemia,10 a hemoglobin of less than 12 in females-RR 2,84 (95% CI 1.96-4.11) P < 0.0001 and of less than 13 in males-RR 2.65 (95% CI 1.95-3.6) P< 0.0001 behaved as risk factors for perioperative transfusions. The new clinical practice guidelines of the American Society of Blood Banks consider the administration of therapy prior to surgery to prevent anemia a good practice that may lead to lower transfusion requirements.14 Finally, surgeries that extend beyond the average time of 144 minutes also showed a positive association with transfusion, with an RR 1.65 (95% CI 1.32-2.08) P < 0.0001. Similar to this study, Aoude et al, found that patients undergoing thoracolumbar surgery and extended surgical times, are predictors of blood transfusion requirement.15
Conclusions
Resource optimization and lower risk for patients undergoing surgical procedures should be the goal when planning blood reserves and later use of red blood cells. The results presented show that the level of RBC reserves exceeds the requirements for the number of transfusions actually administered. A case in point is orthopedic procedures with a high level of RBC reserves but a small number of transfusions; this proportion should be reviewed, keeping in mind the ideal transfusion reserve index of less than 2.5 units resered per each unit transfused.
Being aware of the risk factors involved with patients undergoing surgery and their RBS transfusion requirements improves our preparedness and helps to mobilize all the available prevention resources such as blood-saving measures, including preoperative anemia treatment, the use of medications such as tranexamic acid or the use of cell-saving agents, inter alia.16
Perioperative patient care is a shared responsibility among all the specialists involved in the surgical procedure. Therefore, there is need to unify criteria and to establish the parameters to decide which patients do require RBC reserves and which patients are at higher risk of requiring a transfusion, in order to educate the patient about this possibility and to make sure that the resources are available before surgery begins. Our findings show that there are some variables that could be considered for decision-making purposes.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.











 text in
text in