1. Introduction
To allow controlled ventilation, the airway must meet two primary characteristics, mentioned in order of priority: the airway must be open (allow airflow with minimal resistance); and it must be sealed (protected against bronchoaspiration and without air leakage). Failure to meet these conditions leads to a difficult airway (DAW), but classically, and from the operational point of view, it is better defined based on the difficulty to ventilate using a facemask (DFMV), difficult tracheal intubation (DTI), or both. Although rare (1-5%),1-3 these conditions are a significant source of morbidity and mortality, and of claims directly associated with the anesthetic practice.4) Their management tends to be difficult because of the large number of rapidly interacting time-dependent factors. Particulary, quick and sound decision making, which may determine the outcome but leaves no room for improvisation and on the contrary, demands a well-supported predesigned strategic plan.
2. Evidence, guidelines, and algorithms
In addition to the study design, the details on the circumstances under which the study was carried out are also important. There is good quality evidence with regards to forecasting and prevention strategies (sections 3,4, and 5). In the case of critical and rare situations (DFMV or DTI, sections 6,7, 8, and 9), the double-blind, randomized design has little applicability; the recommendations are based on a few low-quality trials, in real-life situations (comparative, noncontrolled series or case reports) or are extrapolated from controlled experiments under parallel situations such as forecast or simulated DAW. The validity of trials performed in normal airway patients, dummies, or bodies is even poorer.5
Several scientific anesthesia societies worldwide have tried to compile the available evidence and process it in the light of expert consensus for publication as management guidelines; some are expressed graphically as algorithms.6-24 However, the applicability of such guidelines may be limited, as they comprise recommendations not available in our setting, either because excessive complexity, or ambiguous suggestions, or because the recommendations are too specific for a particular clinical situation or a particular type of patient.
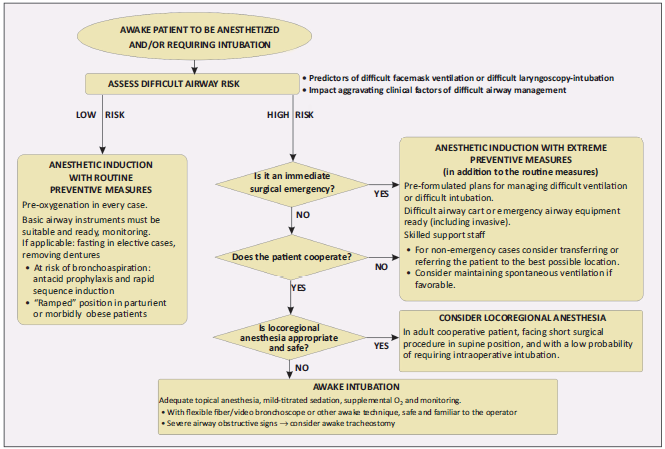
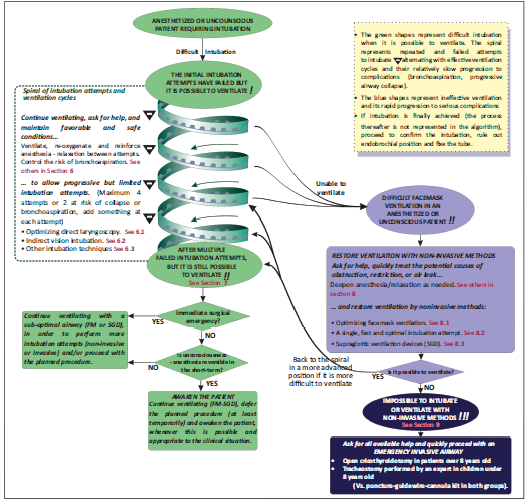
This article is intended to summarize and organize the current recommendations and trends, prioritizing them in terms of their effectiveness (possibility to achieve the expected result), safety (low incidence of adverse effects), and universality (applicable to most patients, operators, institutions, and clinical situations), but making the corresponding exceptions to the general recommendation. Since this review basically consolidates the recent guidelines and expert consensus, the level of evidence attributed is IV and grade of recommendation is D. The guidelines are summarized graphically in the attached algorithms (Figs. 1 and 2). The article focuses on the management of the patient that will undergo anesthesia and requires intubation, but it could also be applicable to other critical care settings. The options available in our environment are emphasized, as well as those that should be available based on adequate support. The suggestions herein presented can not be considered mandatory and should be subject to individualized clinical judgment. The techniques are described just superficially but require formal theoretical-practical training prior to their implementation. The generic names of the devices are used, and just a few brand names are mentioned as an example, though other brand names may be of similar value.
3. Risk prediction
As already known, risk assessment is based on searching clinical predictors for DFMV or DTI; the higher the number of predictors, the higher the risk (Table 1).6,10,12 Forecasting scales that contribute with a qualitative or quantitative risk value have been developed using multivariate analysis. Some of the scales that have shown improved precision for DTI are those developed by Arné et al, Wilson et al and Naguib et al2,3 and for FMDV those of Langeron et al, Yildiz et al and Kheterpal et al.1 Notwithstanding the above, prediction is still an inexact science, since even scales exhibit a moderate discriminatory power, with a tendency to over-predict the problem with false positives and creating a slight but real possibility of false negatives resulting in the unexpected occurrence of the problem.3,12
Table 1 Predictors and impact aggravating factors of difficult airway management
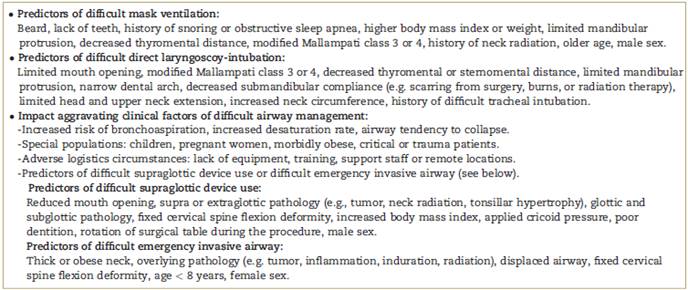
Source: Extracted and adapted from Kheterpal et al,1 Baker et al,2 Naguib et al,3 Black et al,8 Apfelbaum et al,10 Law et al,11 Mhyre et al.16
Source: Author.
In addition to probability, other variables should be considered based on clinical circumstances that do not alter the probability of the problem occurring, but if present, could make management difficult, increase the tendency to result in serious adverse outcomes, or worsen the morbi-mortality. These variables may be called impact aggravating clinical factors and include the risk of bronchoaspiration,6,7,25 increased desaturation rate,12,25) and the tendency of the airway to collapse by repeated trauma.8,19 Several of these factors often converge in special populations: children (particularly younger),8-19 pregnant women,7,16,17 morbidly obese patients,12 and critically ill and traumatized patients.23,24 Also, adverse logistical and operational circumstances such as lack of adequate equipment, or familiarity with the equipment, untrained staff, the absence of expert assistance and remote locations must be considered.12 The risk of difficult use of supraglottic devices (SGD) and difficult surgical access to the airway are additional aggravating factors and variables to consider as part of the management plan.12,25
4. Low risk
In this case, the induction of anesthesia may proceed, provided the routine preventive measures are in place to avoid problems, facilitate management, or reduce the severity of complications. Some of the standard measures include fasting in elective cases, removing dentures or mouth piercings. In patients at risk of bronchoaspiration, the use of antacid prophylaxis and rapid sequence induction is advised.26
Both conventional oxygenation (3 minutes of tidal volume with 100% oxygen) and rapid oxygenation (4-8 forced volumes in 30-60 sec), significantly increase the oxygen reserve and time prior to desaturation during apnea,27 providing valuable time to take action before the development of hypoxia. The superiority of the former method has been shown, and it is important to maintain the contact of the mask with slight pressure. An expired oxygen fraction of over 90% has been suggested as objective parameter of adequate preoxygenation.7,28 In parturient and morbidly obese patients, the "ramped position" (elevating the patient's thorax and head until the external auditory meatus and the sternal notch are in the same horizontal plane) improves the quality of pre-oxygenation and facilitates ventilation and intubation after induction.5,9,12,16
The availability and functionality of equipment for airway management is mandatory before any anesthetic induction. The equipment must be ready, tested and suitable for the size of the patient.22 Many routine situations can become critical if the equipment is absent or inoperable.4 The pediatric population requires a broad range of sizes of devices.8-14 It is advisable to have a difficult airway cart or kit at every surgical location, containing additional and specific material for managing these emergencies. This cart must be complete, organized, and subject to regular inspection.10,14,18 Some of the devices that the cart should contain will be mentioned in the text.
5. High risk
When several DFMV or DTI predictors are present, particularly in combination with aggravating factors, the safest and most supported option is awake intuba-tion.12,17,18,25 The strategic advantage of this approach is that spontaneous ventilation is maintained during intubation attempts as well as the protection by reflexes against bronchoaspiration, and if it fails, it could give the opportunity to desist, defer and reconsider the conditions of induction.6,12,18 It requires patient collaboration, adequate topical anesthesia of the upper airway and the trachea, mild and titrated sedation, supplemental oxygen and variable doses of patience, skills, and time.18,21 The most supported device for awake intubation is the flexible fiberoptic/video bronchoscope (FOB).10,12,18,22 This technique requires the availability, proper functioning, and prior operator training that every anesthesiologist should have. Given the aforementioned strategic advantages of awake intubation, in the absence of a flexible fibro-bronchoscope, other intubation devices can be considered if they are at least safe and familiar to the operator. The examples include the use of direct laryngoscopy,10,12,17 videolaryngoscopy, or other indirect vision instruments.10 Only under special circumstances and when the resuscitation practitioner has specific expertise, semi-invasive or poorly supported awake intubation methods would be justified, including retrograde intubation9,29,30 or blind nasotracheal intubation.10,18
One exception is patients with clinical signs of critical airway obstruction (tumors, laryngeal angioedema, severe croup or epiglottitis), since attempts at awake oro/nasotracheal intubation may increase the inflammation and finally collapse the airway, leading to an extremely critical situation.31 In this case, the safest option is also awake intubation but through a surgical approach (awake tracheostomy), performed by an experienced surgeon, under the same conditions as described above, and a judicious infiltration of local anesthetic.12,17,32
The role of locoregional anesthesia in patients at high risk of DAW is subject of debate; some consider it a strategic way to avoid difficulties in high-risk air-ways,10,12,17,21 while others warn that a hasty intubation will be needed under a less controlled situation in case of failure in locoregional anesthesia.5,18,33 Locoregional anesthesia may be an option when appropriate and with low probability of failure, in an adult cooperative patient, facing a short procedure, in supine position, as long as an intraoperative deterioration of the state of consciousness, breathing, or perfusion is not expected. In case intubation is needed, it may be performed awake, under the above-described conditions.10,12
Another major exception is non-cooperative patients (children, psychiatric adult patients, delirium or severe cognitive disorder) or immediate surgical emergencies (e.g. severe ongoing bleeding, fetal distress with bradycardia, etc.),7,12,15,24 where awake or regional options are not feasible. In these cases, you may proceed with anesthetic induction, as long as extreme preventive measures are adopted (in addition to the routine measures listed under section 4). This means selecting the most favorable location and having several pre-planned back-up strategies for difficult ventilation or intubation as well as the necessary staff and devices, including invasive devices (e.g., DAW cart and surgeon on site).10,12,34 In the pediatric population or in patients with non-critical airway obstruction, anesthetic induction maintaining spontaneous ventilation could be advantageous.11,15
6. In the anesthetized/unconscious patient, the initial intubation attempts have failed but it is possible to ventilate
In this difficult managment situation, the patient is requiring FM or SGD ventilation, which is effective; the airway is patent though unprotected, and intubation is required, but the initial attempts have failed. The general recommendation would be: continue ventilating, ask for help, and maintain favorable and safe conditions to allow progressive but limited intubation attempts using available techniques that are effective, safe and familiar to the operator (optimization of direct laryngoscopy, indirect vision methods and others)6-11,15-19,23,24 This situation is represented by the spiral tracing of the algorithm that comprises effective ventilation cycles, alternating with intubation attempts; the downward spiral progression symbolizes the progressive risks of bronchoaspiration7,9,23,24 and airway collapse as a result of repeated trauma.5,15,19,35 Such risks are constantly present, but vary based on the patient's condition (see section 3). Repeating the same failed intubation maneuver indefinitely is ineffective and increasingly risky35; therefore, the attempts must be progressive (adding favorable conditions at each step, in terms of maneuvers, devices, or operator expertise) and limited to a number considered to be safe,7,11 suggesting 34 in the usual cases6,11 and 2-3 in the above-mentioned cases of risk.7,9,14,19
As examples offavorable and safe conditions, the following can be mentioned: ventilate and reoxygenate in-between failed attempts, using 100% oxygen, unless contraindi-cated8,9 (e.g. risk of retinopathy in premature children or in some heart diseases), atraumatic suction of secretions as needed, and ocular protection. The recommendations in case of risk of bronchoaspiration are: rapid sequence induction,7,11,23 avoid ventilating before intubation, but if needed, limit the inspiratory pressures to the minimum required for chest expansion (eg, 20 cmH2O in parturi-ents),7,11 maintain continuous cricoid pressure (Sellick's maneuver).7,9,11,23 However, inappropriate or exaggerated cricoid pressure could interfere with ventilation, laryn-goscopy, tube advancement or a SGD; hence, the pressure shall be lowered or released as needed.7,9,12 In parturient and morbidly obese patients, maintain the "ramped position."6,7,12,16 When cervical spine trauma is suspected, keep at least the back part of the stabilization collar, and have an assistant maintain alignment manually during the ventilation and intubation maneuvers.23,24
An important favorable condition that must be maintained is anesthetic depth; since the effect of the anesthetic induction doses fades away quickly, additional repeated doses of intravenous or inhaled anesthetic agents, opioids and even muscle relaxants are usually required. This improves intubation conditions, decreases hemodynamic or respiratory responses and prevents awareness.6,7,8,21 A valuable strategy is to use only short-acting or pharmacologically reversible drugs, to maintain the possibility of waking the patient when the situation persists for a long time.
6.1 Optimizing direct laryngoscopy intubation
The following suggestions help to optimize glottis visualization or tube insertion and advancement: correct any errors in the maneuver or inadequate selection of tools; adapt the sniffing position to the size of the patient (in adults, one low round pillow maybe useful, children over 2 years old should be on a flat surface, and in children under 2 years, a bolster under the shoulders may be useful).6,8,36 When the mouth opening is limited, the operator may force it open using crossed fingers to facilitate initial laryngoscope placement; also traction on the right labial commissure may enhance the visual field.36 Thyroid pressure (different from Sellick), called BURP or OELM, consistently improves visualization of the glottis6-9,11,14,15; however, an exaggerated pressure may hinder laryngoscopic vision or tube advancement, especially in children.8 Exchanging laryngoscope blades randomly may be useless; but, if the epiglottis is too far or covers the glottis, exchanging for a longer curved blade or a straight blade may be considered.11 Selecting cuffed tubes that are narrower than usual may reduce the number of failed attempts or the need for exchange.7,8,11,17
To intubate a partially visible glottis (Cormack-Lehane 2 or 3a), a semi-rigid pre-inserted stylet, which molds the tube in a "hockey stick" shape, improves tube tip guidance. It is important to make sure that the guide does not extend beyond the tip of the tube to avoid trauma and use a smooth or lubricated guide to allow withdrawal at initial insertion into the glottis.10,21 An alternate - and probably more effective - option,22,37 is the Eschman type introducer (or Bougie, 60 cm, flexible, malleable, with an angled atraumatic tip), inserted into the trachea during conventional laryngoscopy. Here, it is advisable to slide the tube without removing the laryngoscope.6,7,23 In case of any difficulty, turning the tube 90 degrees counterclockwise may prevent the tube from snagging on the epiglottis.6 The original reusable Bougie has been shown to be more effective and less traumatic than disposable versions,9,38 and there are also pediatric variants.14
6.2 Indirect vision intubation
There are two groups of techniques considered effective: the use of video-laryngoscopes and flexible fiberoptic bronchoscope (FOB) intubation through a SGD. Video-laryngoscopes (e.g. Glydescope, McGrath, Airtrach, King Vision) have shown increasing evidence of moderate quality under difficult intubation situations,10,39,40 in diverse patients and clinical settings,6-9,10 tend to be intuitive, and allow for better visualization of the glottis. There is some on-going discussion on whether any one of them has a superior effectiveness,40 or prevents major complications in comparison to conventional laryngoscopy.41 However, in our clinical settings, these devices pose difficulties in terms of costs and maintenance needs.
Fiberoptic intubation through a SGD - such as the laryngeal mask (LM) - is more time-consuming but has the advantage of simultaneously maintaining ventilation. The intubation LM (eg, Fastrach, limited to patients with more than 30 kg) allows for direct sliding of the tube9,10,42-45; the classical LM usually requires a series of consecutive steps consisting of inserting a guide into the trachea using the FOB, then removing the LM and the FOB, and finally sliding the tube over the guide.6,8,11,45 Depending on the patient's size, the tube, and the LM, a hollow guide may be used externally pre-inserted into the FOB in adults (eg, Aintree catheter),9,6,11 or a long flexible, metallic guidewire, with an atraumatic tip may be introduced through the work/suction canal of the FOB in children.14,15,46 Other second-generation SGDs could facilitate the fiberoptic bronchoscope intubation, usually with the above-mentioned SGD-FOB-guide-tube sequence.44,45
6.3. Other devices and intubation techniques
Other intubation techniques have insufficient or inconsistent effectiveness data, or their effectiveness heavily depends on the operator's training. These techniques may be considered based on availability, functionality and operator familiarity. Some examples include blind intubation through the intubation LM,13,42,43 with rigid-angled bronchoscope15,40 (e.g. Bonfils), and straight rigid bronchoscope in children.10,12,14,15,19 There is less support for the use of the flexible fiberoptic bronchoscope as a single device in an apneic patient,18,20,22 the retrograde intubation,29,30 and the use of trans illumination guides.10,22 Blind intubation through the conventional LM9,19 and blind oro-nasotracheal intubation or through manual or digital manipulation are not recommended.19,20
If the intubation succeeds, it should be confirmed with clinical parameters, and ideally using capnography, rule out selective intubation and fix the tube adequately. Otherwise, refer to the next section.
7. After multiple failed intubation attempts, but it is still possible to ventilate
In this moderately severe situation, the safe limit of failed intubation attempts has been reached (2 to 4, depending on the risk of collapse or bronchoaspiration), but adequate ventilation is still possible using the FM or SGD. The primary recommendation would be: continue ventilating, defer the planned procedure (at least temporarily), and awaken the patient.6-11,15-19 If awaking the patient is not possible or applicable: continue ventilating with a sub-optimal airway (FM or SGD), in order to perform more intubation attempts (noninvasive or invasive) and/or continue with the planned procedure.6-11,15-19,23,24
The most prudent and supported option is to awaken the patient, if possible and appropriate for the clinical situation (anesthetized patients for elective cases or non-inmediate surgical emergencies). Continue FM or SGD ventilation, maintaining the safety measures described under Section 6; discontinue anesthetic-relaxants, or use reversal agents as needed. Sugammadex (up to 16mg/kg) is used for early drug reversal of profound relaxation with rocuronium.6,8 Once the patient is awake, reassess the situation with the knowledge of the risk (see section 5).7,11
When it is not possible to awaken the patient (state of unconsciousness or nonreversible anesthesia in the short term) or it is not applicable (immediate surgical emergencies that cannot be delayed even for minutes), other options must be considered.6,7,11 When the risk of bronchoaspiration or collapse is low, additional intubation attempts can be performed but these should be optimized, and plans should be ready to support ventilation emergencies, including invasive options.6,11 Continuing ventilation in order to perform a semi-emergency tracheostomy is more appropriate in trauma or critically ill patients, or in cases of extremely high risk of bronchoaspiration.11 When these options fail or are not suitable, or in an immediate surgical emergency, the only option is to continue with the procedure, ventilating with a sub-optimal airway6-8,16,23 (usually SGD), even when this implies risks of bronchoaspiration and/or intraoperative ventilation failure. In this case, it is advisable to restrict any surgical maneuvers that may facilitate regurgitation (abdominal pressure, peritoneal insufflation, Trendelem-burg, etc).7 Some second-generation SDGs with enhanced sealing and airway protection (eg, LMA ProSealTM, LMA SupremeTM ) may be advantageous under such circumstances.11,16,44,45,47-49
8. Difficult facemask ventilation in an anesthetized or unconscious patient
This potentially critical situation may arise any time after induction or following the intubation-ventilation cycles. In this case, the recommendation would be: ask for help, quickly treat the potential causes of obstruction, restriction or air leak and restore ventilation by noninvasive methods, such as facemask ventilation optimization, a single, fast and optimal intubation attempt or supraglottic devices.6-11,15-19 Waking the patient is not an option, since in the absence of ventilation, there would be significant morbidity/mortality prior to recovering consciousness or spontaneous ventilation.50
Light anesthesia may cause bucking, thoracic rigidity or laryngospasm that hinder ventilation; hence, additional titrated doses of anesthetic (in this case intravenous) are justified, and also of a muscle relaxant if required.6,8,11,14 The reason for the obstruction may be a foreing body, secretions, regurgitation, or exaggerated Sellick. Bronchospasm, pneumothorax, gastric insufflation (particularly in children), and leak due to poor sealing are other causes of difficult ventilation that need to be managed specifically.6,8,11,14,51,52
8.1. Optimization of facemask ventilation
This should be the first step when FM ventilation is not effective.51,52 It is recommendable to use 100% oxygen, correct any maneuver errors or inadequate selection of tools, adjust the sniffing position based on patient's size6,8,9,36 (see section 6.1), and use an oro-pharyngeal cannula of proper size and positioning. Four-hand ventilation with two operators helps with the protrusion of the mandible, improves mask sealing, increases the effectiveness of ventilation, and reduces operator fatigue.14,16,51,52 The ramped position is advantageous for parturient and obese patients.6,7,12,16
8.2. A single, fast, and optimal intubation attempt
Inability to ventilate a patient with a facemask does not necessarily mean intubation is not possible, though there is a weak statistical correlation.8,51 Almost all the patients included in the largest group studied in a real situation of impossible ventilation with a facemask could be intubated in 1 or 2 attempts.1 The recommendation of the attempt of intubation is also advisable in this case, in order to rule out the possibility of foreign body that may cause the obstruction. For this reason, the attempt of intubation must be made before inserting a SGD.14,15 It is particularly suitable when prior attempts have not been made and there is a pressing need to protect the airway or when there is the suspicion of an obstructive foreign body; however, the attempt must be expeditious and optimized (see section 6.1).
8.3. Supraglottic ventilation devices
SGDs may reestablish ventilation when FMV has failed.6-8,10,11 The classical LM6-8,53 and the combitube are the most supported, 9,17,22,25,54 though the latter tends to be more traumatic and limited to patients over 120 cm in height. Other disposable or reusable SGDs, though less supported, may be effective, and some of the second generation may offer some advantages such as improved airtightness, or facilitating fiberoptic intubation.44,45
If any of the previous options succeeds in reestablishing ventilation, the situation returns to the mentioned spiral of intubation attempts and ventilation cycles (sections 6 and 7), but in a more advanced position if it is more difficult to ventilate. In children, a minimum pulse oximetry limit of 80% without cardiovascular effects has been suggested to be sufficient to maintain transient short-term options, such as awakening, intubation attempt or surgical airway (but not proceeding with surgery).8 If ventilation is not possible, move on to section 9.
9. Impossible to intubate or ventilate with non-invasive methods
In this extremely critical and life-threatening situation in which intubation or ventilation have not been possible using all the available noninvasive methods, the result is rapid progressive deoxygenation, complications with sequelae or death within minutes, unless ventilation can be reestablished. In this case, wakening the patient is not an option, and the use of invasive methods of intubation or at least ventilation is justified. The recommendation would be: ask for all available help and quickly proceed with an emergency invasive airway: open cricothyrotomy in patients over 8 years old or tracheostomy performed by an expert in children under 8 years old (vs. puncture-guidewire-cannula kit in both groups).6-11,15-19
In adults and children over 8 years old, the method of choice is open cricothyrotomy.6,7,9,18,24,55 This method involves making an incision in the more superficial and avascular point of the airway (the cricothyroid membrane) to be channeled with a tracheostomy cannula or an endotracheal tube, ideally cuffed and of a slightly thinner diameter than would be used through the orotracheal approach (e.g., 6 mm ID in an adult). This allows for rapid re-oxygenation with a protected airway and is a transient method that lasts for hours or days, that allows to perform the procedure, awaken the patient or switch to conventional intubation or tracheostomy in less urgent and better controlled circumstances. The simplified "four step" technique has been described, which could be effective in urgent situations, even in the hands of an inexperienced rescuer.9,55 Several guidelines advise against emergency tracheostomy because it is a laborious, time-consuming technique and it can lead to serious complications when performed under stress, unless performed by an experienced surgeon.9,20,21,55
In contrast, in children under 8 years old, the cricothyroid space is too narrow and less accessible, and the cricothyrotomy may result in severe laryngeal trauma8,14,56 In this case, an emergency tracheostomy performed by an experienced surgeon is the method of choice.8,9
One option for both groups is the use of specially designed equipment, adapted to the patient's size, for the puncture-guidewire-cannula sequence55 (crico-thyro, crico-tracheal, or tracheal). Wide bore cannulas are suggested (>4mm ID) for patients over 8 years old6,11 while narrow bore cannulas (<4mm ID) are suggested for children under 8 years old.6,8,11,56 When the diameter is slightly narrower than the trachea, rapid oxygenation is enabled with no air entrapment55,56; some of them are cuffed to provide protection and sealing. When thin, uncuffed cannulas are inserted (narrower in comparison to tracheal size), ventilation requires high flows and pressures (usually jet ventilation) to compensate for high resistance and leakage; and exhalation occurs by passive retrograde leakage into the pharynx and not out through the cannula. They are contraindicated in case of complete upper airway obstruction due to the risk ofair entrapment and barotrauma.56
Improvised methods by puncture with large diameter intravenous cannulas (14-16 g) are not effective in adults and children over 8 years old, due to their extremely high resistance and excessive leakage, kinking tendency, risk of tissue insufflation, and barotrauma.6,7,11,55 Some believe that these cannulas may work in children under 8 years old, since they require lower inspiratory volumes.56 They are contraindicated in complete high obstruction, are only justifiable in the absence of other more effective methods, require adequate coupling to the circuit and jet ventilation, and only contribute a few minutes of oxygenation, while the patient awakens or more reliable methods are established.8,11
10. Conclusion
When predicting risk, in addition to looking for difficult airway predictors, it is important to consider the clinical circumstances that could further complicate the problem if it emerges. Recently developed devices and novel techniques are valuable tools to respond to airway emergencies; however, the knowledge and skills in managing the conventional intubation and ventilation techniques and their optimization strategies are irreplaceable. In addition to focusing on solving the intubation problem, the general clinical condition of the patient must be simultaneously addressed (ventilation, level of anesthesia, risk of bronchoaspiration, the urgency of the procedure, etc). Besides focusing on maneuvering to reestablish ventilation, any potential causes hindering ventilation shall be ruled out or treated (superficiality, air leak, foreign body, respiratory restriction, etc). A simple, practical, and well-supported thought process helps to deal with complex situations, foresee and prevent any difficulties, make right and timely decisions, and improve outcomes.
Ethical responsibilities
Protection of people and animals. The author declares that no experiments have been conducted on humans or animals for this research.
Confidentiality of the data. The author states that patient data does not appear in this article.
Right to privacy and informed consent. The author states that patient data does not appear in this article.











 text in
text in