Introduction
The treatment of chronic pain requires medications and interventions aimed at improving the patient's quality of life. Among these medications, opioids stand-out, particularly when pain persists despite optimal non-opioid therapy.1 The route of administration affects the effectiveness of analgesia and tolerability.2 Intrathecal administration is an option for chronic pain, regardless of whether it is cancer associated or not, when patients are intolerant to other routes of administration (ie, oral, transdermal), or when there is poor response to conventional therapy or to interventional therapy.3 Moreover, the intrathecal route enables a combination of drugs and different mechanisms of action, variable programming, and even self-administered boluses in case of incidental pain.4 Intrathecal infusion pumps were used for the first time in humans in 19825 and have shown analgesia effectiveness, improved quality of life, reduced drug dose, and less adverse effects.2,5
The refill process is essential for intrathecal therapy. The manufacturer recommends using a template to localize the puncture site and access to the refill port.6 The template shall be aligned-through palpation-with the pump edges, a process called the blind technique.7 This method has some potential limitations such as the need for multiple punctures and the risk of pocket fill, a potentially fatal complication due to the accidental injection and infiltration of medication into the subcutaneous tissue.5 Maino et al7 reported that the deviation to the refill port using the blind technique may be as high as 16 mm. From 1996 through 2010, Medtronic Inc. (710 Medtronic Parkway, Minneapolis, MN 55432-5604, USA) received 351 pocket fill reports, including 8 fatalities.5 The use of the fluoroscope has been suggested as an alternative to optimize refill and reduces such deviation in up to 8mm.7 However, its routine use is limited because of the ionizing radiation exposure, poor portability, and availability. Ultrasonography (US) is widely used for pain management. It may optimize the localization of the pump'srefill port and avoid the limitations of the blind technique and fluoroscopy.8
A successful case of static refill of the intrathecal pump through ultrasound localization of the refill port, with no need of continuous observation of coordinates and with coordinates, allowing for a precise puncture is described.
Patient information
A 39-year-old male patient, with a history of anchylosing spondylitis with 15 years of evolution, diagnosed in 2000. The patient was followed by rheumatology and managed with adalimumab 40 mg every 15 days, with adequate progress. However, the somatic axial chronic pain persisted and then the patient was treated with high potency opioids (ie, morphine, fentanyl, methadone) with minor side effects that were refractory to treatment and limited their use, despite a favorable analgesic response. The patient underwent interventionist analgesic management with poor response.
Clinical findings
The patient presented with a history of essential hypertension, gastroesophageal reflux disease with secondary esophagitis and chronic gastritis. No familyhistory. Physical examination with adequate vital signs, limitation to lumbar flexion-extension, and positive Schober test; the rest of the systems remained unaffected. Paraclinicals with elevated acute phase reactants. Blood test, renal and liver function were normal. The radiographic images were compatible with ankylosing spondylitis. HLA-B27 results not available.
Diagnostic approach and evaluation
Analgesia optimization was suggested in June 2011, with the implantation of a SynchroMed II 8637-20 (20 mL reservoir, 870950 catheter) intrathecal pump (Fig. 1), leading to improved symptoms. Currently the patient is being managed with intrathecal hydromorphone 349.7 mg/dl with refill interval of 102 days, adequate pain modulation and no adverse effects. The template provided by the supplier was used during refill, making it necessary to do multiple punctures and needle redirection to localize the refill port; the decision was then made to do ultrasound-guided puncture.
Therapeutic approach and evaluation
A novel and simple method to localize the US-guided intrathecal pump refill port with static technique is described, developed on the basis of previous experiences,8 as an alternative to the continuous method described by Gofeld et al.8 As far as we know, this is the first description of the use of this technique for this particular indication.
The procedure was performed in the operating room under basic monitoring.
The reservoir arrangement and residue was checked using telemetry. The subcutaneous pump was localized through a palpation method.
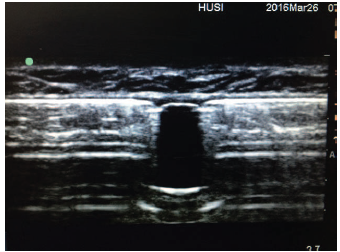
Using a high frequency lineal transducer Sonosite EDGE US machine, and parameters for soft tissues, depth 2.7 cm, and resolution definition, the transducer was placed on the abdominal wall in the pump area to identify the anterior aspect and contours. The body of the pump was localized, visualizing a hyperechoic line with acoustic shadow.
An entry port was localized, which was visualized as an anechoic area interrupting the hyperechoic line described (Fig. 2). The port is located in the middle of the screen, which corresponds to the center of the transducer.
A line perpendicular to the center of the transducer on the skin of the patient is drawn with a permanent marker. The line is drawn on both sides of the transducer.
The transducer rotates 90 degrees to shift the axis and once again scans to identify the port, which is found in the middle of the screen. A line perpendicular to the center of the transducer on both sides is drawn again, and the transducer is removed.
This is the method to draw the lines that in a target-like manner (ie, 2 axes), project over the skin the exact location of the refill port. When prepping the skin, the marker may be erased, so the recommendation is to place a soft pressure mark (eg, needle cap) at the intersection of the lines, and then proceed with the usual puncture and refill.
Follow-up and outcomes
The patient has adequate pain modulation, complies with treatment and has less side effects. Control visits to the pain clinic are scheduled every four months. Pump refills continue to be performed with the technique described, with no complications and satisfactory results. The pump's adequate performance indicates that the refill procedure is both feasible and effective.
Discussion
The technique describes the use of US for intrathecal infusion pump refill using a static coordinates methodology that is simple, safe, and low cost. This tool is presented as an option for intrathecal pump refill, with potentially shorter refill times and enhanced risk profile.
The use of intrathecal analgesia is a useful option for chronic pain management (cancer and non-cancer)3 and will probably become increasingly frequent due to the aging population.9
Pump refill based on anatomical localization presents a rare but significant risk of injection and infiltration into the subcutaneous tissue, with the possibility of drug overdosing or underdosing, as is the case with baclofen, leading to a potential fatal outcome.7,10 A fluoroscopy-guided approach has been presented as an option to reduce such risk.7 However, this involves high costs, limited availability and portability, in addition to radiation exposure of the patient11 and the healthcare staff.12 Ultrasonography is a valuable option for chronic and repetitive refill5: lower costs, increased portability, no radiation exposure, and does not rely on infrastructure.13 Furthermore, ultrasonography allows for the identification of complications associated with the need for repeated pump refills14 or associated with the pump's position.5 Gofeld et al8 described the benefits of ultrasound in a cadaveric model for intrathecal pump refill under continuous observation of the port. Shankar14 described its use in a patient with seroma over the refill port, identifying the wider port diameter to establish the ideal puncture site; the pump refill was accomplished under continuous observation.
Though the advantages of the technique seem unde-batable, one of the limitations when using any US-guided technique is the need to complete a learning curve.15,16 Gofeld et al8 reported that a professional with no experience in US-guided procedures is able to master the refill technique after practicing for approximately 30 minutes.5 This suggests that this methodology may involve a short learning curve and an acceptable safety profile of the procedure, as has been suggested for ultrasound interventions in anesthesiology.17
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent: The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.











 texto em
texto em