Introduction
Chronic pulmonary thromboembolism (PTE) is a frequent cause of pulmonary hypertension (PHT). A pattern of chronic embolic pulmonary hypertension may develop (CEPHT) as a result of a partial resolution of a PTE or a relapse thereof. It is characterized by the presence of fibrous and organized thrombus in the vessel lumen, which may lead to total occlusion of the pulmonary arteries, with increases pulmonary vascular resistance (PVR) and subsequent right heart failure.1 The incidence reported for CEPHT in patients with acute PHT ranges from 0.57% to 3.8%.2-4
CEPHT is the only curable cause of PHT with surgical management through pulmonary endarterectomy (PE). This procedure is intended to optimize the hemodynamic condition and reduce PVR (reduce the right ventricular work), optimize the ventilation/perfusion ratio (reduce dyspnea), and avoid arterial disease in the vessels not involved (reduce the progression).5
The objective of this retrospective study of a series of cases was to do a clinical characterization of patients undergoing PE at a Colombian Level IV referral center over a 5-year period of time and analyze the perioperative events and significant associated outcomes.
Material and methods
An active search of subjects undergoing PE from January 2009 through January 2017 was conducted, based on a database developed from 2009 for cardiovascular surgery. This information system was designed on an electronic platform (FileMaker Pro 10 for MacOS; Santa Clara, California). The database included all the relevant bio-metric and clinical data of the preoperative evaluation, anesthetic approach, intraoperative complications, postoperative details, and surgical morbidity during the patients' hospital stay. Particular care was exercised to ensure the confidentiality of the subjects included in the database. The records were made through updates, as applicable, with the information of patients undergoing cardiovascular procedures in 1 single center, having the electronic medical record as the primary source of information.
The preoperative data collected to conduct this study included age, sex, weight, height, ventricular function, preoperative medications, surgical history, relevant cardiovascular history such as high blood pressure, metabolic disorders, renal function, inter alia. Intraoperatively, the perfusion times, aortic clamping, and total heart arrest time, number of circulatory arrests and total arrest time, crystalloids, transfusions, use of inotropic agents and vasoactive drugs, as well as any complications were recorded. In addition, hemoglobin levels and initial and final excess bases were also noted.
The postoperative data included endotracheal intubation time (measured after OR discharge), ICU length of stay, the volume of fluids received during the first 24 and 48hours, as well as the global water balance at 48hours, based on the actual initial weight of the patient. The use of vasoactive and inotropic agents was also recorded, in addition to any morbid events and postoperative complications until patient discharge.
Intraoperative management
All patients received a standardized anesthetic induction that included midazolam (0.1-0.2 mg/kg) and fentanyl (23 mg/kg) administration. Then, a neuromuscular block with vencuronium (0.1mg/kg) was administered, in accordance with the ideal weight, followed by the endotracheal intubation with a dual-lumen tube, as part of the strategy for managing any potential airway bleeding. The invasive monitoring included a pulmonary artery catheter and an arterial line, preferably femoral, to avoid underestimating as described in the values measured in the radial artery following circulatory arrest with profound hypothermia.6 Monitoring of the bilateral cerebral perfusion was done using near-infrared spectroscopy (NIRS; INVOS Oximeter; Somanetics, Minneapolis, Minnesota).
Transesophageal echocardiography was performed in all patients from the moment immediately after induction. Maintenance was administered with age-adjusted sevofluorane at 0.6 isoCAM and infusion fentanyl, in accordance with the hemodynamic behavior. Circulatory arrest and extracorporeal circulation conducted under profound hypothermia (20°C), allowing maximum 20-minute intervals, with reperfusion times of 10 minutes or less, according to the NIRS values, with the objective of recovering regional cerebral venous saturation back to its initial surgical values and never below 40% for over 10 minutes.7 Local cold, methylprednisolone (15mg/kg), phenytoin (15mg/kg), propofol (1-2mg/kg), and mannitol (0.25-0.5 gr/kg) were used as cerebral protection estragies during circulatory arrest, in accordance with a recent review published by Banks DA et al.5 In every case, the dual-lumen tube was replaced by a single-lumen tube at the end of the procedure, and the patient was transferred to the ICU where the initial management was continued along with subsequent de-escalation of the ventilation and hemodynamic support.
Statistical analysis
The continuous variables are presented as means and standard deviation or as medians and interquartile ranges (IQE), in accordance with the Smirnov-Kolmogorov normality test. The categorical variables are presented as percentages or absolute figures.
Results
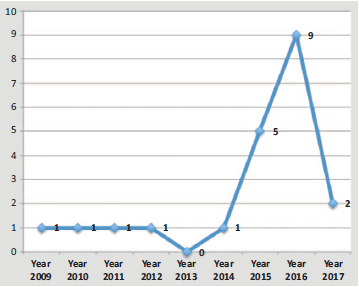
Over the study period (2009-2017), 21 subjects were identified, and no one was ruled out. The median values (IQR) for age, weight, and size for this series of cases were 48 (30-70) years, 73.4 (55-110) kg, and 165 (155-180) cm, respectively. Most of the patients were females with decline of their functional class (NYHA III and IV) (Table 1). A growing number of cases was observed as of 2015 (Fig. 1).
Table 1 Demographic data and intraoperative characteristics.
| Females, n (%) | 12 (57.1) | |
| Age, mean (IQR) | 48 (30-70) | |
| Average BMI, kg/m2 (SD) | 27 (5.4) | |
| Functional class NYHA, n (%) | ||
| I-II | 5 (23.8) | |
| III | 11 (52.4) | |
| IV | 5 (23.8) | |
| Pre-existing comorbidities | ||
| DVT, n (%) | 2 (9.5) | |
| HBP, n (%) | 11 (52.4) | |
| Heart failure, n (%) | 15 (71.4) | |
| LVEF < 50%, n (%) | 12 (57.1) | |
| Tricuspid regurgitation, n (%) | 7 (33.3) | |
| Cases transfused n (%) | 21 (100%) | |
| RBCs, n (%) | 12 (57.1) | |
| FFP, n (%) | 6 (28.6) | |
| Cryoprecipitates, n (%) | 13 (61.9) | |
| Platelet concentrates, n (%) | 16 (76.2) | |
| Average extracorporeal perfusion time, mean (SD) (minutes) | 242.9 (82.8) | |
| Intraoperative nitric oxide, n (%) | 9 (42.9) | |
| ICU stay, h; mean (IQR) | 179 (27-528) | |
When analyzing the preoperative conditions, 12 subjects had a diagnosis of heart failure; 57% (n = 12) has an ejection fraction between 40% and 50%, and 42.9% (n = 9) had ECG-diagnosed tricuspid regurgitation. Coronary disease (1 vessel) was documented at the time of the procedure in 1 patient; the remaining angiographies were negative for coronary disease. The mean perfusion time (SD) was 242.9 (82.8) minutes. The median (IQR) of ICU stay was 179 (27-528) hours and of orotracheal intubation was 50 (0-260) hours.
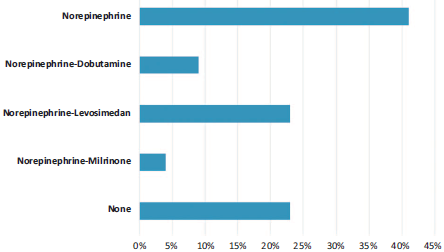
During the postoperative period, 77% of the subjects required some type of postoperative hemodynamic support (Fig. 2). The most frequent complications were cardiac complications (right and bi-ventricular dysfunction) and pulmonary (pulmonary edema and severe diffusion disorders). One case required venous-arterial extracorporeal membrane oxygenation (ECMO) and another one required mechanical ventilation > 72hours. Three cases of postoperative acute renal failure were identified. Ten percent (n = 3) of the patients required reintubation due to pulmonary edema. Two patients died (9.5%), one of them associated with multiple organ failure and another one as a result of massive bronchoalveolar bleeding (Table 2).
Table 2 Postoperative complications.
| Postoperative morbidity and mortality | n (%) |
| Pulmonary | 3 (14.3) |
| Hypoxia | 2 (9.5) |
| Bronchoalveolar hemorrhage | 1 (4.8) |
| Cardiovascular | 12 (57.1) |
| Right ventricular failure | 6 (28.6) |
| Bi-ventricular failure | 2 (9.5) |
| Vasoplegic syndrome | 3 (14.3) |
| Extracorporeal support (ECMO VA) | 1 (4.8) |
| Coagulopathy and bleeding | 3 (14.3) |
| Renal failure | 3 (14.3) |
| Permanent neurological damage | 1 (4.8) |
| Sepsis | 1 (4.8) |
| Death | 2 (9.5) |
ECMO VA=extracorporeal membrane oxygenation - venous arterial.
Source: Authors.
Discussion
HPCTE is a condition with a poor prognosis. Its estimated survival is 30% when mean pulmonary arterial pressure (PAPm) is > 40 mm Hg and 10% for PAPm > 50 mm Hg.8 The current management of the condition involves anticoagulation and PE,9 which is considered potentially curative. In order to make this decision, the hemodynamic status, the associated comorbidities, and a sound surgical plan based on diagnostic images must be taken into account. The institutional experience and the experience of the team caring for CEPHT patients are critical for a maximum reduction of severe perioperative events.10,11
The analysis of previously published PE series of cases indicates a heterogeneous morbidity and mortality, closely linked to the cumulative experience and surgical technique used. The group from the University of San Diego (San Diego, California) is probably the group that has described a larger number of cases (over 2700 to date), with an initial mortality of 17% in the first 200 cases (1970-1990).11 Then, the mortality dropped to 2.2% according to their publication in 2012.12 In Latin America, Favaloro et al13 reported an experience of 41 cases in 18 years, with a hospital mortality of 17% at 30 days. These reports with results very close to those reported in our paper show a similar rate of complications and postoperative problems. To this date, no randomized clinical trials analyzing the long-term morbidity and mortality of medical management, as compared with EP, are available.
Selecting the patients who are candidates for surgery is an ongoing controversial topic. The benefits including the potential cure shall be evaluated, but on the contrary, the risk of perioperative complications must not be neglected. However, currently, several groups suggest that no patient should be considered inoperable is the source of the PHT is thromboembolic.12 The major risk factor traditionally described is PVR. PVR values of > 1000 and 500 dines/ seg/cm5, during the pre and postoperative period, respectively, have been independently associated with residual distal vascular disease and right postoperative ventricular failure. However, it has been recently suggested that even PVR values > 1500dines/seg/cm~5 could undergo PE, with no significant increase in morbidity and mortality.14
During the PE intraoperative period, multiple interrelated factors should be considered that may result in genuine surgical catastrophes. Some of these factors are the severity of PHT, pre-existing of acute unset right ventricular failure, the usual hypercoagulability status, the deleterious effects of profound hypothermia, and prolonged extracorporeal circulation, the total arrest time, vasoplegia, and perfusion-related lesion, inter alia. Our perioperative management is based on the recently published management guidelines.5 While PE was initially described over 40 years ago, it is an emerging surgery in developing countries, with a significantly smaller case series as compared against the referral centers in developed countries. Some of the reasons for this considerable difference in the number of cases are situations such as under-diagnosis that limits the surgical option, poor training of the surgical teams, and the difficulty to access health care services for the general population, particularly patients with these high-cost pathologies.
To conclude, it can be said that the largest case series of patients with CEPHT undergoing PE has been described in Colombia. There are multiple interrelated factors that condition the success of the procedure or the occurrence of postoperative adverse events and death. The frequent cardiac and pulmonary complications make it mandatory for centers intending to conduct these procedures to consider cardiopulmonary support therapies such as ECMO, and to have a multidisciplinary team ready to identify and treat early any associated complications. Further research is required on the prognostic factors and intervention strategies associated with lower morbidity and better postoperative quality of life in these patients.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.











 texto en
texto en