Introduction
Complications during airway management are an important cause of morbidity and mortality in the practice of anesthesia; hence, the constant adoption of devices to facilitate the approach and the use of multiple algorithms specifically for the management of the difficult airway. According to an analysis of the American Society of Anesthesiologists (ASA) Closed Claims Database,1 with the introduction of modern respiratory monitoring in the mid 1980s and the adoption of guidelines for the management of the difficult airway in 1993, death and permanent brain damage due to difficult intubation have declined significantly; however, difficult intubation accounted for 27% of adverse respiratory events between 1990 and 2007.
The incidence of failed intubation is estimated at 0.05% and 0.35%, and it is higher among patients with neck masses, among others. The incidence of difficult intubation ranges between 5.8% and 10.3%,2 and, interestingly, up to 93% of all cases of difficult intubation occur in patients with unanticipated difficult airway, according to the Danish Registry.3
Anaplastic thyroid cancer accounts for 1.3% of thyroid malignancies, and it is 1 of the most aggressive solid tumors, with a mean survival of 4 months.4 Peak incidence is found between 65 and 70 years of age, and treatment is usually palliative because of very rapid decline. In advanced cases where the patency of the upper airway is compromised, tracheostomy is a valid alternative.
Tracheostomy is 1 of the oldest surgical procedures, the first descriptions dating back some 4000 years. However, due to the growing interest in minimally invasive procedures, variants of the classical procedure have now been developed, and percutaneous tracheostomy has gained popularity. Additionally, the use of ultrasound guidance has emerged as an option for a large number of procedures, including airway assessment and manage-ment,5 and guidance for real-time percutaneous trache-ostomy.6
Case description
Patient information
The patient was a 62-year-old female patient, weighing 65 kg, and with a history of noninsulin-dependent diabetes mellitus type II, arterial hypertension, and chronic obstructive pulmonary disease. She has had a mass in the left side of the neck for the past 20 years, which started to grow rapidly three months ago, causing dysphonia and dysphagia solid food.
Clinical findings, diagnostic assessment, and interventions
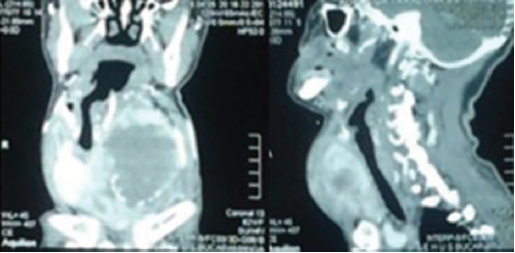
Neck and chest computed tomography (CT) imaging revealed a thyroid tumor and right internal jugular vein thrombosis, and metastasis to the lung and rib cage. The tumor was 9.3 x 8.7 cm in size on its axial dimension, and 10.2 cm on the vertical axis, causing significant lateral displacement of the trachea to the right, and posterolateral displacement of the vascular structures (Fig. 1). Histopathology reported a grade IV anaplastic thyroid cancer. Thyroid function tests showed evidence of hypothyroidism, prompting the initiation of propranolol.
The patient was assessed by the head and neck specialist who identified the need for palliative tracheostomy in view of the advanced stage of the disease. The preansthesia assessment found clear predictors of a difficult airway, Mallampati III, diminished neck mobility and mouth opening, and a large mass on the left side of the neck, associated with dysphagia and dysphonia. The electrocardiogram was normal, prior functional class I/IV, whole blood time, coagulation times and electrolytes were also normal, with the only finding being a slightly lower albumin value.
Before the procedure, the case was reviewed with the head and neck surgeon who thought that the significantly distorted surgical site was associated with a high risk of complications and difficulty accessing the trachea in case of an open approach, and decided to use a percutaneous approach. The need for securing the airway with orotracheal intubation was defined jointly, based on the risk of losing patency if the procedure was performed under deep sedation. Repeated review of the images showed displacement in the infraglottic region with mild involvement of the glottic and supraglottic areas and of the calibre of the airway. This information prompted the use of awake intubation with a flexible reinforced orotracheal tube. The first choice, given the mild compromise of the glottic and supraglottic regions, was videolanryngcospy, thinking about orotracheal intubation in the event adequate visualization of the vocal cords was achieved. The second choice was the use of a fiberoptic bronchoscope. The informed consent was obtained after a detailed explanation about the need for the procedure. Upon admission to the operating room, monitoring was initiated with electrocardiography, pulse oximetry, and noninvasive blood pressure monitoring. After preoxygenation, sedation and analgesia were achieved with fentanyl 65 |xg(1 mg/ kg) and ketamine 13mg (0.2mg/kg), maintaining spontaneous ventilation. Topical 4% lidocaine was administered to the oropharynx and the supraglottic region, video-laryngoscopy was performed with CMAC, achieving adequate visualisation of the glottis on the first attempt with no noticeable patient discomfort, and a #7.0 tube was advanced with no difficulty. Propofol 120 mg, remifentanil 0.2 mg/kg/min, and 1.5% sevoflurane were administered after capnographic verification (Fig. 2).
Upon initiation of the procedure, the surgeon was unable to localize the trachea to perform the percutaneous approach, so the anesthesia team proposed the option of using ultrasound guidance to identify the trachea and perform the puncture. The anesthetist proceeded to localize the trachea under ultrasound guidance using the linear transducer of a SonoSite machine. When the trachea had been localized and the other anatomical structures had been identified, the TRACOE kit was opened, and the head and neck surgeon performed an ultrasound-guided puncture in the transverse plane (Fig. 3) using a #14G catheter and secured the airway on the first attempt, with no complications. The metal guide wire was then advanced smoothly, the opening was progressively dilated with the help of a dilator, and a #7.5 cannula was introduced (Fig. 4), confirming correct placement by means of capnography.
Follow-up and outcome
The patient remained hemodynamically stable throughout the procedure. She was alert, oriented and breathing spontaneously through a patent tracheostomy when she was transferred to the recovery room. A gastrostomy was performed on the 10th hospitalization day and the patient was discharged home 20 days after the first intervention.
Discussion
Successful airway management is critical to avoid debilitating and fatal complications. Tracheal intubation may be achieved in several ways, direct laryngoscopy being the most frequently taught. However, in patients with an anticipated difficult airway, it is not the first option. In this setting, standard management is intubation using the fiberoptic bronchoscope with the patient awake. More recently, videolaryngoscopy has been included as an option for the initial approach in these patients, in accordance with the Guidelines for Difficult Airway Management of the ASA.7
The use of videolaryngoscopy is relatively new, and it is aimed at improving the success of intubation. It is effective for difficult airway management,8 and improves glottic visualization when compared with the traditional Macintosh blade.9 A recent study compared 4 video-laryngoscopes (CMAC, Vividtrac, McGrath, Kingvision), and found that the CMAC, because of its design, allows to observe more relevant details, improving intubation time.10 For cases of unanticipated difficult airways, the English management guidelines mention the importance of training in the use of videolaryngoscopy and the need for its immediate availability in urgent cases. Some anesthetists actually consider it as the first option in laborious intubation.11
There is a growing body of evidence on awake intubation using the videolaryngoscope in obese patients.12,13 A recent clinical study compared video-laryngoscopy and fiberoptic bronchoscopy for awake intubation in patients with anticipated difficult airway taken to bariatric surgery. The study found that video-laryngoscopy resulted in significantly faster intubation times.14 However, in patients with neck masses, the literature is scant, making our case interesting.
When the intubation was accomplished and the surgeon found difficulty localizing the trachea and was unable to perform percutaneous cannulation using the traditional landmarks, the airway was then identified with the help of ultrasound to guide the puncture for the percutaneous tracheostomy. The theoretical advantages of the use of ultrasound include the identification of the trachea and of the puncture site, the assessment of the vascular structures, and, above all, visualization of the tracheal puncture in real time. The current literature supports the use of ultrasound for percutaneous trache-ostomy as a fast, safe, and reliable tool,6,15 which offers a plausible advantage over the traditional use of anatomical landmarks, especially in selected groups of patients such as the morbidly obese or those in whom palpation of the neck anatomy is difficult.16
Airway management in patients with neck masses that distort the anatomy is very challenging. Successful management is key to avoid debilitating complications and even death. In our case, we believe that CMAC videolaryngoscopy, and also fiberoptic bronchoscopy, were adequate options considering that the main compromise was infraglottic and there was no critical the upper airway stenosis. Videolaryngoscopy was selected as the first choice because of greater experience with its use. This case points to the need for efficient coordinated work among the members of the team to ensure successful management, by the anesthetist and the surgeon. Additionally, ultrasound must be immediately available in the management of patients with a difficult airway because it is indispensable for guiding percutaneous airway cannulation in situations where even an experienced surgeon has difficulty performing the procedure because of significant anatomical distortion of the neck.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.











 texto em
texto em